the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
October 23, 2023
One page summary
What is the message?
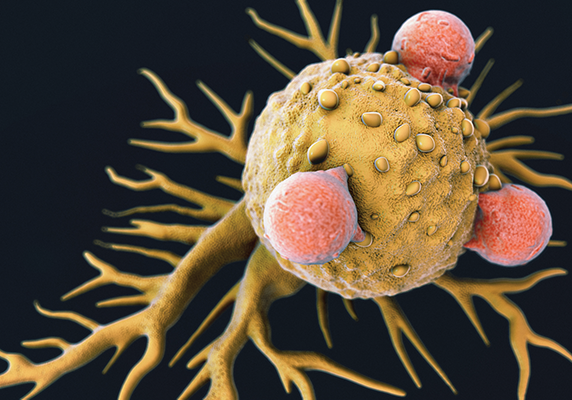
A groundbreaking wave of cancer treatments is set to redefine how cancer is treated, employing a revolutionary approach that utilizes patients’ own cells as drugs.
This innovative cell-based therapy leverages the body’s immune system to identify and combat cancer cells, offering patient-specific and highly effective treatment.
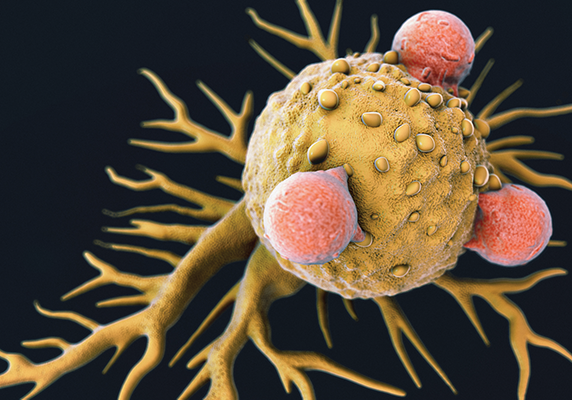
Credit: iStock
Key Takeaways
A Paradigm Shift in Cancer Treatment:
Traditional cancer treatments, such as surgery, radiation, and chemotherapy, are being complemented by cell-based therapies that harness the power of a patient’s immune cells to target and eliminate cancer.
Customized and Patient-Specific:
Cell-based cancer therapy isolates immune cells from the patient, genetically enhances them for increased potency, and then reintroduces them to specifically combat the patient’s tumor, minimizing the risk of rejection.
Remarkable Early Results:
Early trials have demonstrated dramatic results, including complete remission in advanced metastatic cases, giving hope to patients previously given only months to live.
CAR T-Cell Therapy:
One transformative approach, CAR T-cell therapy, has been approved for blood cancers, but there is an ongoing quest to extend its effectiveness to solid tumors, which constitute the majority of cancer cases.
Identifying Cancer Markers:
To enhance cell-based therapies’ effectiveness, innovative methods are being developed to identify cancer markers, both on the surface and inside tumor cells, to broaden the scope of treatable cancers.
Streamlining and Accessibility:
While these therapies are personalized, ongoing efforts are aimed at streamlining the labor-intensive process of generating therapeutic cells to make these treatments more accessible and potentially the standard of care for various cancer types.
Examples and Statistics
- Early Success: Cell-based therapies have demonstrated the complete remission of advanced metastatic disease in patients who had very limited life expectancies.
- CAR T-Cell Approval: In 2017, the FDA approved CAR T-cell therapies for blood cancers, marking a significant milestone in cell-based cancer treatment.
- Solid Tumor Challenge: Solid tumors account for approximately 90% of cancer deaths, and efforts are underway to adapt cell-based therapies to be effective against these tumors.
- Costly Personalization: The highly personalized nature of these therapies currently involves labor-intensive cell generation for each patient, highlighting the need for more efficient production methods.
Conclusion
Cell-based cancer therapies represent a promising and transformative approach to cancer treatment, offering customized and highly effective solutions.
While the journey continues to optimize and broaden their application, early successes suggest that they may become the standard of care for various cancer types in the near future, revolutionizing the fight against this devastating disease.
DEEP DIVE
Cells as Cancer Drugs
Horizons – National Cancer Institute
Surgery, radiation, chemotherapy and targeted therapies have been standard treatments for cancer. A revolutionary wave of cancer treatments that use patients’ own cells as drugs will permanently change how we treat the disease.
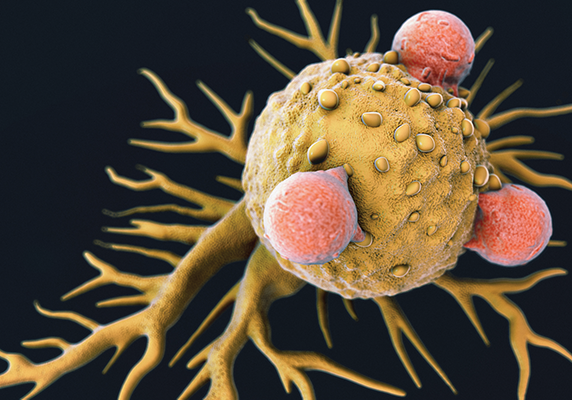
Credit: iStock
Surgery, radiation, chemotherapy and targeted therapies have been standard treatments for cancer, but they are no longer the only options. A revolutionary wave of cancer treatments that use patients’ own cells as drugs will permanently change how we treat the disease.
The general principle behind cell-based therapeutic approaches is to exploit the natural ability of the body’s immune system to recognize and neutralize invaders. In cell-based cancer therapy, immune cells that recognize cancer cells are isolated from a patient, genetically engineered to be more powerful and then multiplied before they are reintroduced into the patient to fight the tumor.
The advantages are many. The treatments are patient-specific and use only the patient’s own cells, thus avoiding the risk of the body rejecting transplanted cells. Each treatment is customized for a specific type of cancer and importantly, the transferred cells can survive, multiply and continue operating within the patient’s body so that only a single therapeutic treatment is needed.
Early results have been dramatic, including the complete remission of advanced metastatic disease in patients given only months to live. As with all therapeutic approaches, side effects can be significant and not all patients seem to benefit, so the quest to minimize toxicity and expand the efficacy of these “living drugs” continues.
One of the earliest approaches to result in cancer remission identified anti-cancer immune cells that had penetrated the environment in and around a patient’s tumor. Those cells, known as tumor-infiltrating lymphocytes (TILs), are then multiplied in the lab and reinfused into the patient.
Newer approaches genetically engineer T cells to be more effective. A potentially transformational method, known as CAR T-cell therapy (where CAR stands for the chimeric antigen receptor added to the T cell), recognizes a target on the surface of a cancer cell and destroys the cell. In 2017, the U.S. Food and Drug Administration approved the first two CAR T-cell therapies to treat blood cancers. One, axicabtagene ciloleucel (Yescarta), was initially developed in CCR.
A limitation of CAR T cells is that they recognize only targets found on the surface of a cancer cell. This is proving valuable in cancers of the blood but less so in solid tumors that account for around 90 percent of cancer deaths. To address this issue, innovative new approaches involve engineering a patient’s T cells to recognize cancer markers both inside and on the surface of tumor cells to render them effective against a broad range of solid cancers.
In many cancers, it is difficult to identify cancer-specific markers to target or predict which patients will respond to therapy. New approaches to spot potential targets using high-throughput methods to screen cells can expedite the search for targets. Most trials of cell-based therapies have involved small numbers of patients in single institutions around the world, so computational methods that can analyze results across these studies will also accelerate progress.
A different but also promising tactic is to revitalize a patient‘s cancer-fighting cells by reverting them to a stem cell-like state in the laboratory. It may be possible to coax these stem cells to develop into “younger” anticancer T cells with a greater capacity to flourish inside the body than a patient’s own aging immune cells.
All of these cell-based therapies are highly personalized and, as a result, currently require costly and labor-intensive generation of therapeutic cells for each patient. One area for progress will be the streamlining of production methods to more rapidly generate these individually tailored cells. A breakthrough on that front will boost the accessibility of these promising therapies and hopefully will make them the standard of care for many cancer types in years to come.
Originally published at https://ccr.cancer.gov/news/horizons/article/cells-as-cancer-drugs