JAMA
Avinash Maganty, MD1; Lindsey A. Herrel, MD, MS1; Brent K. Hollenbeck, MD, MS1
May 15, 2022
roboticoncology
New biological agents, imaging tests, and devices are among the many sectors of technology that have an important role in health care delivery.
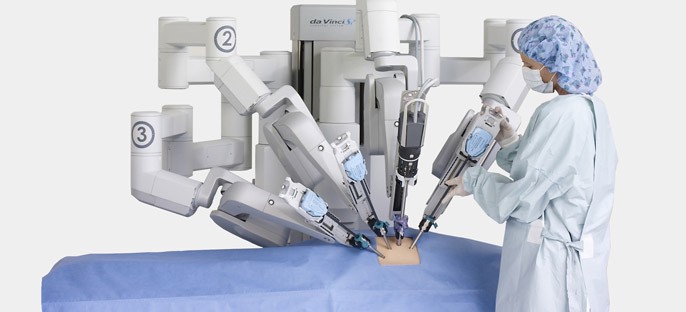
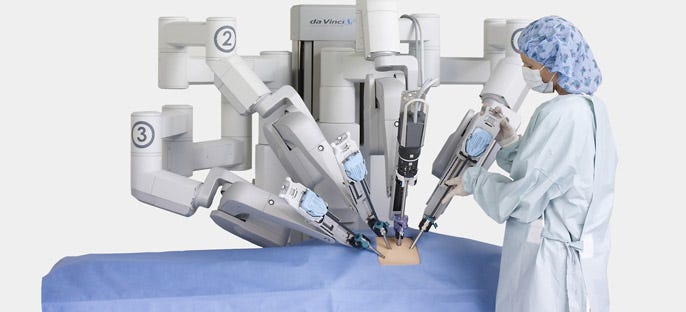
These technologies vary in the extent to which they aim to replace an existing procedure or medical therapy or provide a new way of treating patients. They also vary widely with regard to their value (ie, incremental clinical benefit and cost) to society. Following approval of the da Vinci Surgical System by the US Food and Drug Administration (FDA) in 2001, robotic surgery has disseminated rapidly across various disciplines and procedures, substituting for conventional (ie, open) or laparoscopic alternatives.1
Much of the diffusion of robotic surgery occurred prior to rigorous evidence supporting its clinical utility and value.
For example, robotic surgery for prostate cancer has largely supplanted open surgery. It has increased from an estimated 22% of procedures in 2003 to 86% in 2020,2 in the absence of large-scale clinical trials demonstrating comparable or improved cancer control and quality-of-life outcomes. While retrospective analyses of nearly 2 decades of data provide some reassurance in this context,3 the safety and efficacy of robotic surgery are not universal. A recent clinical trial that compared minimally invasive hysterectomy with open hysterectomy in 631 patients with early-stage cervical cancer found a 10.6% lower 4.5-year disease-free survival rate in the minimally invasive surgery group (survival rates, 86.0% vs 96.5%), prompting an FDA warning.4
A rigorous assessment of the value of robotic surgery is increasingly important as its application continues to expand in cancer surgery.
For patients and surgeons, robotic surgery offers the potential to reduce the perioperative morbidity commonly associated with cancer surgery. Robotic radical cystectomy, a potentially curative treatment for patients with bladder cancer, is one such procedure that has high perioperative morbidity, with a 30-day reoperation rate of up to 39% (range, 9.7%-39%) and a 90-day mortality rate of up to 3% (range, 1.7%-3%), depending on the type of urinary diversion.5 Similar to other procedures, the adoption of robotic cystectomy has increased, from 29% of cystectomy procedures in 2008 to 54% in 2018, despite limited evidence of its benefit over the open approach.6
Two large clinical trials have compared robotic and open radical cystectomy to date.
In a single institutional trial by Bochner et al 7 … that involved 118 patients,
- there was no significant difference in the primary outcome of 90-day complications (inclusive of grade 2–5 complications defined by a modified Clavien system, which included 11 categories, such as bleeding, infection, wound, etc),
- with rates of 62% in the robotic surgery group vs 66% in the open surgery group (95% CI for difference, −21% to −13%; P = .7),
- but the study did conclude that the robotic approach was associated with longer operative time, less blood loss, and a similar length of stay.
- Long-term follow-up did not reveal significant differences in cancer recurrence or survival, although the trial was not specifically powered for these outcomes.
The RAZOR trial 8 was the first multi-institutional trial that compared robotic surgery with open surgery using a noninferiority design to assess progression-free survival in 350 patients.
- The authors reported comparable 2-year progression-free survival 72.3% [95% CI, 64.3%-78.8%] in the robotic cystectomy group and 71.6% [95% CI, 63.6%-78.2%]) in the open cystectomy group.8
- In terms of secondary outcomes, the robotic group had a longer operative time but less blood loss.
- Adverse events and patient-reported outcomes were similar between the 2 groups.8
- Notably, the length of stay was modestly shorter in the robotic surgery cohort (6 days [IQR, 5–10 days] vs 7 days [IQR, 6–10 days]; P = .02).
- Given the results of these 2 trials, it would appear that meaningful differences between the robotic and open approaches have not been demonstrated.
- However, both trials involved an open incision to perform the urinary diversion, which may negate the benefits of a completely minimally invasive approach (ie, performing both bladder removal and urinary diversion intracorporeally).
In this issue of JAMA, Catto and colleagues 9 address this evidence gap by studying an entirely robotic approach compared with open bladder removal.
In this phase 3 multicenter trial, 338 participants were randomized to robotic cystectomy with intracorporeal urinary diversion or open radical cystectomy with urinary diversion.
The 2 groups were balanced with respect to patient characteristics and measures of disease severity (eg, tumor grade, histology, and stage).
Hypothesizing that the main benefits of robotic surgery would be most apparent in the early postoperative period, the study’s primary outcome was the cumulative number of days patients were alive and out of the hospital at 90 days after surgery.
This innovative, multidimensional outcome captures many facets of morbidity that would interest patients, including length of stay, complications severe enough to delay discharge during the initial hospitalization or require readmission, and duration of readmission, which may also reflect severity.
Although the trial was not explicitly powered for these analyses, the authors explored 20 secondary end points, including cancer control and patient-reported outcomes.
- With respect to the primary outcome, patients in the robotic surgery group had significantly more days spent outside of the hospital — a median of 82 days (IQR, 76–84 days) alive and outside of the hospital compared with 80 days (IQR, 72–83 days) for those in the open surgery group.
- Consistent with prior trials, patients undergoing robotic surgery required longer operative times, had less blood loss with fewer transfusions, and spent fewer days in the hospital initially.
- By 12 weeks, 63.4% of patients in the robotic surgery group and 67.9% of those in the open surgery group experienced a complication.
- The rates of wound-specific complications (5.6% vs 17.3%; difference, −11.7%; 95% CI, 18.59% to −4.58%) and thromboembolic events (1.9% vs 8.3%; difference, −6.5%; 95% CI, 11.43% to −1.38%) were lower in the robotic surgery group.
- Notably, a higher percentage of patients in the open surgery group were readmitted to the hospital (32% vs 22%; P = .04).
- At a median follow-up of 18.4 months (IQR, 12.8–21.1 months), there were no significant differences between the robotic surgery and open surgery groups in cancer control outcomes, recurrence rates (18% vs 16%, respectively), or overall mortality (14.3% vs 14.7%), respectively.
- Relative to the robotic surgery group, patients in the open surgery group tended to have worse measures of quality of life, disability, and physical activity within the first 12 weeks after surgery. However, these differences diminished by 26 weeks.
Several factors distinguish this study from prior trials.
First, the primary end point for which the study was powered used a composite measure to assess early postoperative recovery, which previous trials were not designed to evaluate.
This composite measure of recovery is important because the benefits of robotic surgery are perceived to be realized in the period soon after surgery.
Second, this trial stipulated the use of Enhanced Recovery After Surgery (ERAS) protocols in both groups.
Differences in postoperative recovery between open and robotic approaches may become negligible with the use of ERAS.10
However, even with ERAS use in both groups, this trial showed a benefit favoring patients undergoing robotic surgery.
Third, the robotic group included an intracorporeal approach to urinary diversion, maximizing any potential benefits of a completely minimally invasive approach.
Collectively, the current study in JAMA along with the previously published trials offer more complete evidence regarding the clinical differences between robotic and open cystectomy.
Collectively, the current study in JAMA along with the previously published trials offer more complete evidence regarding the clinical differences between robotic and open cystectomy.
In addition to radical cystectomy for bladder cancer, robotic surgery has enabled the expansion of minimally invasive approaches to include other complex cancer procedures, such as pancreaticoduodenectomy, rectal resection, oropharyngeal cancer resection, and major hepatectomy.11–14
However, most studies have primarily assessed feasibility, with few rigorously establishing efficacy relative to standard approaches.
This is likely illustrative of the challenges associated with clinical trials in surgery, which are often associated with inadequate power, low accrual, reduced generalizability, and the inability to adequately control for heterogeneity in surgeon experience.
Nevertheless, studies have generally shown associations of robotic procedures with longer operative times, decreased blood loss, and modest reductions in length of stay.3,4,8,12,13
Because evidence from clinical trials reflects average effect sizes, some patients do better while others may do worse when the benefits are modest.
Therefore, it is essential to consider whether these differences are clinically meaningful, particularly for procedures for which traditional laparoscopy is equally feasible, provides comparable outcomes, and is less expensive.1,15
As policy reforms aim to promote quality of care and constrain health care costs, it is important to determine in which clinical circumstances new technologies, such as robotic surgery, add value.
As policy reforms aim to promote quality of care and constrain health care costs, it is important to determine in which clinical circumstances new technologies, such as robotic surgery, add value.
The study by Catto and colleagues in JAMA9 is an important milestone for robotic surgery, as it is among the first to demonstrate a benefit in a multicenter clinical trial.
Whether the benefit in days spent outside of the hospital is clinically meaningful and sufficient to promote further diffusion is likely to be a source of debate, with rational arguments on both sides of quality and cost issues.
Nonetheless, robotic surgery is here to stay.
Further similar trials in other disease contexts are warranted to refine robotic surgery’s niche in the surgical armamentarium to maximize its value to patients.
Further similar trials in other disease contexts are warranted to refine robotic surgery’s niche in the surgical armamentarium to maximize its value to patients.
References & additional information
See the original publication
About the authors & affiliations
Avinash Maganty, MD1; Lindsey A. Herrel, MD, MS1; Brent K. Hollenbeck, MD, MS1
1 Dow Division for Health Services Research, Department of Urology, University of Michigan, Ann Arbor