The Lancet
Kojo Nimako, DrPH, Prof Margaret E Kruk, MD
September 07, 2021
Summary
- The COVID-19 pandemic has made vivid the need for resilient, high-quality health systems and presents an opportunity to reconsider how to build such systems.
- Although even well resourced, well performing health systems have struggled at various points to cope with surges of COVID-19, experience suggests that establishing health system foundations based on clear aims, adequate resources, and effective constraints and incentives is crucial for consistent provision of high-quality care, and that these cannot be replaced by piecemeal quality improvement interventions.
We identify four mutually reinforcing structural investments that could transform health system performance in resource-constrained countries:
- revamping health provider education,
- redesigning platforms for care delivery,
- instituting strategic purchasing and management strategies, and
- developing patient-level data systems.
Countries should seize the political and moral energy provided by the COVID-19 pandemic to build health systems fit for the future.
LONG VERSION

Introduction
The COVID-19 pandemic is among the worst health catastrophes of the last century; it has caused devastating health effects in some countries and severe economic downturns in many more, and is still far from over.
In all countries, regardless of income level, the pandemic has focused attention on health systems, both their struggles and their vital role.
Citizens, politicians, and the global development community are asking more from health systems than ever before: the expectation is that health care must deal with COVID-19 without neglecting the myriad other health conditions.
For the last two decades, with the impetus of the Millennium Development Goals and Sustainable Development Goals, substantial investments have been made in the health sector in low-income and middle-income countries (LMICs).
However, large gaps in the quality of service delivery and health outcomes amenable to health care persist in many of these countries.
For instance, an analysis by the Lancet Global Health Commission on High Quality Health Systems showed that, among patients with cardiometabolic diseases in seven LMICs, only about half are advised on dietary changes and less than a third receive counselling on exercise.
Similarly, most maternal deaths are preventable through timely, competent care in and around labour, but mothers in LMICs continue to die at exceptionally high rates.
Unsurprisingly people across many lower-income countries express low confidence in the competence of their health systems.
Improvement efforts have generally been at the micro level, targeting the provider or facility.
But interventions such as in-service training, job aids, supervision, and checklists have been minimally effective in improving health outcomes and have proven difficult to scale.
More importantly there is no historical precedent showing that, in the absence of strong foundations (including strong and accountable governance, adequate financing, meaningful regulations, and expert workforce), such an incremental approach can promote a health system from low to high performance.
For institutions often perceived as static, health systems in some settings have shown a surprising degree of adaptation during the COVID-19 pandemic, for example turning to telehealth in place of in-person visits.
How can health systems capitalise on the rise of health on political agendas and the COVID shakeup to refashion themselves for the future?]
In this Viewpoint, we discuss key rules that operate in a high-quality health system and propose openings provided by the pandemic for countries to transform their health systems into high-performing, quality-focused entities.
Key rules operating in high-quality health systems
High-quality health systems consistently deliver health care that can maintain or improve health for all and generate people’s trust while offering financial protection from high costs.
Successful complex adaptive systems, such as health systems, typically share a set of characteristics that complex system theorists call simple rules.
These simple rules are:
- clear aims,
- reinforcing resources,
- constraints, and
- incentives that jointly create the conditions for high performance.
These components are all required as they are mutually reinforcing and jointly nudge the system in the desired direction.
Experience from well resourced health systems confirms the importance of these rules and highlights that there is not a single, all-encompassing solution to achieve excellent care.,
These health system characteristics are situated at the macro level (national) or meso level (subnational) and tackle the social, political, economic, and organisational structures underlying the health system.
When well conceived and implemented, they generate competent and caring health services.
These are not mechanical choices-they require a broad and sustained political, technical, and financial commitment, and the ability of political leaders to delay immediate gratification.
These reforms start with an ambitious political vision but will take longer than one political cycle, thus requiring a community of supporters beyond elected officials, such as technical experts, professional associations, and consumer groups.
These reforms start with an ambitious political vision but will take longer than one political cycle …
The following simple rules are common to all successful health systems. Some are intended to guarantee a minimum floor and others to promote excellence.
Ideally any structural health system reform would consider actions on all four of the rules.
1.Aims
2.Resources
3.Constraints (checks)
4.Incentives
1.Aims
Politics, leadership, and management should combine to develop a clear and shared vision, setting high-quality care as the central goal of the health system.
Although the range of services and their complexity will be constrained by finances, the vision of high quality for the offered services should not be.
These aims should ensure that health systems continue to evolve to meet the needs of the population and that actions are undertaken with the goal of making health systems resilient to everyday and unexpected shocks, equitable in service delivery, and efficient in the use of resources. 3
2.Resources
There is no high-quality health system without highly skilled, committed, motivated providers.
The objective is not solely to train more clinicians.
Rather it is about updated training reflecting the latest pedagogy, extensive post-training supervision to achieve high competence, and professional management to support and enforce excellent practice.
Other vital resources are basic equipment, medications, technologies, and clinics that clinicians want to work in and people want to visit.
3.Constraints (checks)
Safety and clinical effectiveness as well as respectful treatment for patients are all requirements that need to be much more firmly stated and enforced.
This is typically done through a mix of self-governance through managerial supervision, and review and admonition processes administered by professional societies and by external accountability mechanisms, such as audits, complaints processes, patient protection and malpractice legislation, relicensing requirements, and others.
4.Incentives
Incentive systems should begin with strengthening intrinsic motivation — pride in one’s job and altruism.
High-performing health systems place a premium on selecting individuals with these motivations alongside good grades.
A culture of excellence in medical and nursing training is then transmitted through mentorship by senior clinicians and later by health system managers.
Appropriate salary, respect, and professional advancement are the minimum requirements to support extrinsic motivation of highly skilled workers in any field, including health care.
Additional financial incentives should be carefully managed to prevent them from becoming perverse and crowding out non-targeted services, as has been shown in previous pay-for-performance programmes. 10
Competition through well conceived, meaningful comparison on items within clinicians’ control can also be helpful to stimulate improvement.
Strategies to reset health systems post-pandemic: providers, platforms, purchasing and management, and patient-level data
Given the large number of necessary health system elements, where to start?
Here we propose four strategies that we consider central to laying the foundations for high-quality health systems.
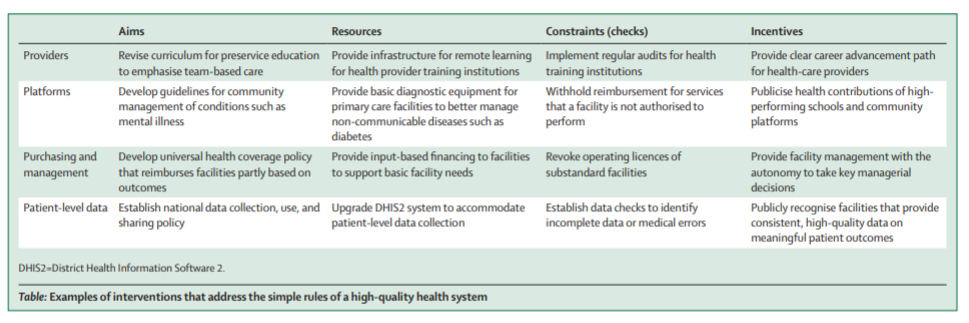
These strategies are informed by historical experience in high-quality health systems but are updated to reflect the context and challenges of legacy health systems in many countries and failures and successes from the COVID-19 pandemic. We provide an illustration of how each of the proposed strategies links to the four simple rules of a high-performing health system in the table.
- Providers
- Platforms
- Purchasing and Management
- Patient Level Data
1.Providers
Providers form the bedrock of a health system and their training shapes their skills and attitude to their work and their patients.
Clinical (preservice) education reforms are badly needed to replace didactic, passive training models in order to instil critical thinking, problem solving, and collaborative skills needed for clinicians in the 21st century.
Competency-based and problem-based learning that develops both technical and interpersonal skills, and promotes cultural and environmental adaptability, should be emphasised. 11
Multidisciplinary care teams, which are a hallmark of high-performing systems, should also be encouraged.
These teams should not only include doctors and nurses, but also professionals who cater for other important aspects of care, including dieticians, physiotherapists, and psychologists.
Partnerships with high-performing and innovative local and international institutions, as was done in Rwanda, 12 and taking advantage of increasingly ubiquitous electronic communication to provide remote support, should also be considered as components of preservice education reforms.
Health training institutions also need to be well regulated to ensure their conformance with best practices.
2.Platforms
Extant models of care provision via clinics, hospitals, and outreach that currently prevail were originally designed for infectious diseases and basic services and no longer serve people well.
With countries undergoing rapid epidemiological and demographic transitions and with lower residual mortality from infectious diseases, 13 the location and provider of care need to be reassessed to produce good health outcomes.
For instance, evidence from several countries shows that with the advent of simplified treatment regimens and point-of-care diagnostics, uncomplicated HIV, hypertension, and diabetes, among others, can now be effectively managed in primary care facilities by well trained nurses and other prescribers. 14
However, mothers and newborn babies are best served if births are attended in facilities where expert teams can provide immediate advanced care, such as caesarean sections, blood transfusion, and care for sick neonates, for life-threatening complications. 15
Furthermore, innovations in non-visit care through telemedicine and community outreach, accelerated by COVID-19, and care that uses platforms outside the health sector (eg, adolescent reproductive health provided through schools or community-based mental health care through religious organisations) should be implemented and tested at scale.
Decisions on revising care platforms need to consider the ubiquity, urgency, chronicity, and complexity for a given condition, as well as equity and cost of care.
3. Purchasing and management
Strategic purchasing is a method of health system financing that reimburses health facilities and providers on the basis of their attainment of explicitly defined outputs and outcomes. 16
Combining this method with input-based methods of financing can help to ensure that basic facility needs (eg, medicines, equipment, and staff salaries) are met to achieve a floor of quality and simultaneously motivate providers to reach higher quality standards. ]
The lessons from the World Bank’s Performance-Based Financing programme 17 suggest that an integration of strategic purchasing into the financing architecture of a country, rather than operating as a standalone top-up scheme, might assist in raising quality, although specific models need further development and evaluation.
Universal health coverage programmes are well positioned to incorporate such payment reform.
Because financial incentives are inherently limited in motivating professionals to improve performance of complex tasks, payment reforms should be instituted in concert with management reforms. 18 , 19
Increasing the number and competence of professional managers at all levels of the health system can assist with transmitting high expectations and instilling a culture of quality. 20
4.Patient-level data
Although health information systems are expanding in lower-income countries, most still do not generate individual-level patient records, as has become the norm in high-income countries.
Such records would support vital registration efforts, promote care continuity and assessment of the quality of care, and provide near-real time outcome data to guide the health system.
The District Health Information Software 2 (DHIS2) Tracker is one approach that can build on widely used DHIS web-based systems. 21
A national data platform with individual-level data would also facilitate rapid and targeted modification of care provision in response to health system shocks — eg, allowing a shift to non-visit antenatal care for some pregnant women when their regular facility is converted into an isolation centre during a disease outbreak.
LMICs should avoid the mistakes prevalent in data systems in high-income countries: lack of interoperability, data overload, and low data use, among others. 22
Considerations for implementation
Countries ready for a health system reset might begin by performing a system diagnostic,
- assessing governance and management capacity,
- financing structures,
- workforce competence and training modalities,
- tools (both hardware and software) and supply chain capacity,
- service delivery effectiveness, and
- extent of person-centredness and population participation in health system design.
The Lancet Global Health Commission on High Quality Health Systems proposed a framework that can be used to guide the assessment.
Useful instruments for this assessment include the Vital Signs Profile toolkit from the Primary Healthcare Performance Initiative, and the Service Delivery Indicators instrument of the World Bank, among others.
The coming People’s Voice Survey, E-Cohorts initiative, and other instruments focusing on people’s experience of health care can be used to gain user perspectives on what is and is not working in the health system.
Any reforms begin with clear aims and committed leadership-this is the province of health system governance.
Governments need to develop a clear definition of health system quality that is shared throughout the health system, and train competent, accountable health system managers.
he National Quality Policy and Strategy handbook developed by WHO can assist. Major reforms are most likely to succeed when they can leverage existing policy openings.
For example, a national policy to implement universal health coverage could be used as an opportunity to redefine and reorganise service delivery, provider training, purchasing, and data systems.
Additional investments in the health sector will be needed to achieve these ambitious plans.
For many African countries, for example, this might require a doubling or more of current government expenditure on the health sector.
Such an increase requires political vision and commitment at the highest levels of government and creative strategies for domestic resource mobilisation.
Additionally, development partners need to place an emphasis on assisting governments to create sustainable, resilient health systems.
Robust health systems research will be needed to understand whether and how reforms lead to a high-performing health system and, crucially, better health outcomes.
Health systems research is poorly, if at all, funded in many countries, resulting in low-quality, small studies that are of little use to policy makers.
Support is needed for studies of larger scale, greater rigour, and more ambitious scope. Implementation science that merges strong quantitative and qualitative research to answer complex questions holds promise.
Although some foundations and development agencies have stepped in to support such work, large cuts to UK funding for global health systems research in response to the COVID-related domestic economic downturn illustrate the fragility of relying on external funding for this vital work.
Conclusion
The COVID-19 pandemic provides what Ulrich Beck has termed a “cosmopolitan moment”, in which a new global appreciation of health risk has presented a new moral and political opening to improve the lot of the collective. 28
Governments and entrepreneurial leaders, supported by citizens, health professionals, and global development partners, have an opportunity to channel the attendant energy, attention, and funding into a meaningful shift towards high-quality health systems.
Contributors
MEK conceived the original idea for the paper; KN and MEK co-developed the ideas for the paper; KN wrote the first draft; MEK reviewed and edited the draft; both authors read and approved the final draft.
Declaration of interests
We declare no competing interests.
Acknowledgments
This work was supported in whole by the Bill & Melinda Gates Foundation (INV-005254). KN writes in his personal capacity; the views expressed in this paper are his and not those of the Bill & Melinda Gates Foundation.
References
See the original publication
Originally published at https://www.thelancet.com.
About the authors
Kojo Nimako
Correspondence
Correspondence to: Dr Kojo Nimako, Maternal, Newborn and Child Health Team (Consultant), Bill & Melinda Gates Foundation, PO Box AN 11671, Accra, Ghana
Margaret E Kruk
Affiliations
Department of Global Health and Population, Harvard T H Chan School of Public Health, Boston, MA, USA
TAGS: Health Reform Pandemic Proof;












