For the industry to fulfill its role in the just transition to a sustainable future, health care leaders are more likely to find the resolve for the “how to get to net-zero” by first embracing a compelling “why net-zero.”
NEJM Catalyst
By Peter Boyd, Joseph Bialowitz, MS, MSc, Terri Scannell, MBA & Jodi D. Sherman, MD
November 4, 2021
At the core of health care is the duty of care and to do no harm.
This central concept is becoming even more urgent and important as population and economic growth are resulting in the burden of civilization exceeding Earth’s carrying capacity.
Reaching the goals of the Paris Agreement requires bold action from all sectors and levels of our society to rapidly reduce greenhouse gas (GHG) emissions.
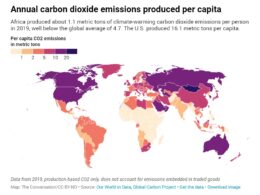
Health care’s climate footprint accounts for nearly 5% of global net emissions so it is reasonable to assume this industry should “do its fair share.”
Health care’s climate footprint accounts for nearly 5% of global net emissions so it is reasonable to assume this industry should “do its fair share.”
There is an emerging body of work examining how health care organizations might reach a goal of net-zero emissions, defined for a corporation as a state in which it is reducing emissions across its value chain to zero or to a residual level that is consistent with reaching net-zero emissions at the global or sector level in eligible 1.5°C-aligned pathways, and neutralizing any residual emissions at the net-zero target date and any GHG emissions released into the atmosphere thereafter.
WHAT IS NET ZERO?
Reducing emissions across its value chain to zero or to a residual level that is consistent with reaching net-zero emissions at the global or sector level in eligible 1.5°C-aligned pathways,
and neutralizing any residual emissions at the net-zero target date and any GHG emissions released into the atmosphere thereafter.
We argue here that to strengthen the industry’s resolve — and the resolve of each individual hospital, clinic, and staff member within — we must address why we’re targeting net-zero.
Indeed, even as we see leaders taking the early steps we need to get there, without a compelling purpose we risk not pushing far enough or fast enough. Especially when times get tough, as they have during the Covid-19 pandemic, it is easy to be distracted by other pressing priorities. For health care leaders, we offer here a few reasons why this is a priority that cannot be delayed, and that can serve as drivers to get to the how and when to act.
We argue here that to strengthen the industry’s resolve — and the resolve of each individual hospital, clinic, and staff member within — we must address WHY we’re targeting net-zero.
Linking Sustainability Purpose to Our Ultimate Purpose
Proponents of corporate social responsibility — the authors of this paper included — often rely upon a theory of enlightened self-interest to persuade business leaders that actions in the best interest of all stakeholders are also in the fiduciary best interest of their company.
However, actions to protect stakeholders — including employees, patients, communities, and even animals and whole ecosystems — can be based on moral principles.
The health care sector harms human health by generating significant and largely avoidable pollution:
- Despite the increasing availability of cost-effective, nonpolluting technologies, the United States health care sector alone releases pollutants that cause a loss of 388,000 disability-adjusted life years (DALYs) annually.
It follows that each of us in health care has a moral imperative to find ways to heal patients without sickening others in our communities and in future generations.
… each of us in health care has a moral imperative to find ways to heal patients without sickening others in our communities and in future generations.
Two important exemplars of this ethos of moral imperative include
- the Catholic Health Association and
- Kaiser Permanente.
The Catholic Health Association consists of more than 600 hospitals in the United States alone (and 5,500 hospitals worldwide) and has a faith-based mission of love and healing at its core.
Many of its members are heeding the call from Pope Francis to join the fight against climate change, which he has passionately characterized as an urgent moral issue because it compromises the future of our common home, threatens human life and human dignity, and adds to the hardships already experienced by the poorest and most vulnerable people both at home and abroad.
To the extent that the health care sector harms the health of both humans and the natural environment by generating avoidable pollution, there is a clear moral imperative for providing care without carbon.
To the extent that the health care sector harms the health of both humans and the natural environment by generating avoidable pollution, there is a clear moral imperative for providing care without carbon.
Kaiser Permanente is an integrated health care provider and not-for-profit health plan serving 12.5 million members.
Its mission includes the objective of “improving the health of our members and the communities we serve.”
In recognition that people can’t be healthy if the environment in which they live is not,
- Kaiser Permanente became a Certified Carbon Neutral,organization in 2020 and
- aims to have a healing effect on the environment by becoming carbon net-positive by 2025.
Kaiser Permanente recognizes that … people can’t be healthy if the environment in which they live is not …
Enlightened Self-Interest: The Initial Business Case
Hospital leaders are stewards of the health of the communities they serve and have the duty to make responsible investments today to protect human health while ensuring high-value, equitable, and resilient care delivery for current and future generations.
Once the net-zero goal is understood as purpose-driven, the business case for transition — based on a theory of enlightened self-interest — can be approached with more fervor and operationalized across entire organizations.
Far from being simply a compliance function or the isolated responsibility of a few committed individuals on a company’s “green team,” sustainability goals are of strategic importance and should, therefore,
- be driven by the CEO and
- integrated into the purpose, mission, and strategy of an organization,
- with board oversight.
Just as with other mission-critical priorities of health care organizations — such as improving quality and reducing staff burnout — a net-zero strategy must be built upon a strong foundation including a roadmap that defines, prioritizes, and plans all required activities needed to implement a chosen pathway, and which specifies an effective operating model (including how a program will be governed and funded, with strong unit-level foundations to ensure that those closest to the relevant processes are empowered to take action and innovate when appropriate).
… a net-zero strategy must be built upon a strong foundation including a roadmap that defines, prioritizes, and plans all required activities needed to implement a chosen pathway, and which specifies an effective operating model
Here we will describe elements of a net-zero business case that have impacts on the organization.
- Improved Patient Outcomes
- Cost Savings
- Cheaper Cost of Capital
- Reusability and Resilience
- Reputational Opportunity
- Talent Attractor
- Investing in the Social Determinants of Health
Improved Patient Outcomes
As hospitals, health care organizations, and entire health systems start to innovate in sustainability, there is increasing interest in quantifying improved patient outcomes.
These better quality outcomes can be achieved in a variety of settings: whether it is improved healing conditions in a more energy-efficient hospital with ample daylight, dimmable lighting, constant temperatures, and fewer drafts; less-stressful and less resource-intensive interventions within a shared decision-making and well-managed multidisciplinary chronic disease management program,; or through intravenous general anesthesia, which has a significantly lower life-cycle climate impact than all forms of inhaled anesthesia,and also reduces postoperative nausea and vomiting.
Preventing harm from health care pollution can directly improve patient care and experience, while contributing to better public health outcomes.
The health care sector harms human health by generating significant and largely avoidable pollution: Despite the increasing availability of cost-effective, nonpolluting technologies, the United States health care sector alone releases pollutants that cause a loss of 388,000 disability-adjusted life years annually.
Cost Savings
The path to a net-zero health care system can and should address building efficiency, energy, transport, food, and procurement.
Energy is a significant percentage of building costs in health care (especially from heating, ventilation, and air conditioning) but not the core product of healing patients; it does not always get enough attention from health care leaders as an opportunity for cost reduction and environmental performance improvement.
In addition to savings and positive-return investments in each of the component areas of the value chain, the overall process by which care is transmitted (e.g., delivering telehealth when appropriate, which is far more efficient than providing avoidable advanced treatments in-person in a large hospital) is also a good example of where these systems interrelate for increased fiscal and emissions savings.
Health care leaders have a moral and fiduciary imperative to deliver care in the least resource-intensive setting.
Cheaper Cost of Capital
When accessing the credit markets, the cost of capital available to health care organizations depends greatly on their assessment by credit rating agencies.
Agencies such as Fitch Group, Moody’s Corporation, and S&P Global Ratings now evaluate companies’ environmental, social, and governance (ESG) performance, including the extent to which companies are successfully managing the risks posed by climate change to their businesses-Over the past 2 years, approximately one-fourth to one-third of rating actions in the corporate sector have been affected by ESG factors.
Effective management of climate transition risk can thus protect or improve a company’s credit rating.
This can, in turn, unlock access to and a cheaper cost of capital: on average, there is cost-of-capital spread of 35–40 basis points between high and low ESG companies.
Effective management of climate transition risk can thus protect or improve a company’s credit rating. This can, in turn, unlock access to and a cheaper cost of capital …
Reusability and Resilience
A purpose-driven approach to the sustainable transition is vital for when times get tough.
During the Covid-19 pandemic, there has been a strain on the global supply chain for much of the equipment needed to deliver care effectively, including single-use products such as personal protective equipment.
- Reliance on reusable products such as isolation and surgical gowns can reduce emissions and shorten the supply chain,
- building resilience while creating jobs in the local communities that health systems serve, and offering better protection than is provided by disposable gowns.
Reputational Opportunity
The financial value of companies in the health care sector is, as with companies in many other sectors, influenced largely by the value of their brand.
The reputation of a health care organization is ultimately determined by how well it cares for the short- and long-term health of citizens and communities.
For these organizations, reputational risks and opportunities are quickly arising due to climate change and its impacts on patients, communities, employees, buildings, and supply chains.
The effectiveness of a hospital’s response to the physical and transition risks of climate change (e.g., increased energy prices and stressed public finances) will influence its reputation — and thus strengthens the business case for climate action.
Consumers, investors, municipalities, and countries increasingly expect leading organizations — including health care companies — to pledge to and then perform against net-zero targets (e.g., Race To Zero as part of the global climate negotiations in COP26, the 26 thannual Conference of the Parties summit).
Perhaps hospitals’ biggest opportunity to impact health is to standardize accounting of the externalities of the products and services in their value chain to align with their mission and purpose.
Far from being simply a compliance function or the isolated responsibility of a few committed individuals on a company’s “green team,” sustainability goals are of strategic importance and should, therefore, be driven by the CEO and integrated into the purpose, mission, and strategy of an organization, with board oversight.
Talent Attractor
Related to reputational opportunity is the ability to attract a strong workforce. Talent is a key driver of both costs and value to a health care organization.
In a global survey by the Global Network of Advanced Management (a network of many of the top business schools in the world), 84% of students said they would choose to work for a company with good environmental practices.
This preference would also appear to translate to a positive return in the war for talent:
- while 44% of students would be willing to accept a lower salary to work for an organization with better environmental practices,
- 19% would not accept a job at a company with “bad environmental practices” no matter how high the salary.
While this particular survey polled business school students, a portion of these will be in the health care profession, and the sentiment appears across sectors. So as organizations are increasingly becoming purpose-driven, so too is the top talent. They are voting with their feet and joining those who are leading efforts to transition to net-zero.
… 84% of students said they would choose to work for a company with good environmental practices. This preference would also appear to translate to a positive return in the war for talent…
Investing in the Social Determinants of Health
Health care organizations should also use the lever of impact investing to support long-term projects that mitigate climate change and improve community health resilience.
This allocation could be relatively easier to justify than for a company with a core product less linked to community vibrancy.
Several leading health care systems in the United States have already pledged to redirect a portion of their investable assets toward impact investments that are place-based and address community conditions that create racial, economic, and environmental disparities.
For example, CommonSpirit Health has committed to allocate 3% of its investment portfolio to place-based impact investments.
Tax-exempt status is awarded to nonprofit organizations so that, in part, they can innovate in areas where the government and private sector may be unable or unwilling to do so.
Spending to help patients and communities cope with the health effects of climate change — for example, through the implementation of community resource locator tools that physicians can use to refer patients to public programs that help them pay for food, heating and air conditioning, transportation, and housing — can protect health while enabling tax-exempt entities to meet their community-benefit spending requirements.
Health Care Leaders Must Act Now
Health care’s roots draw on a deep purpose to heal society, not to harm it.
Explicitly linking the organization’s overall purpose to tightly defined, appropriately ambitious net-zero goals will give senior administrators the strength to fully grasp the challenges and take advantage of this leadership opportunity to institute stewardship principles and practices that protect human health and strengthen access to high-quality and cost-effective care that benefits our generation and generations to come.
References
See the original publication
About the authors & affiliations
Peter Boyd
Resident Fellow, Yale Center for Business and the Environment; Lecturer, Yale School of the Environment; Lecturer in the Practice of Management, Yale School of Management, New Haven Connecticut, USA; Founder and Chief Executive Officer, Time4Good Group LLC, Westport, Connecticut, USA
Joseph Bialowitz, MS, MSc
Head of Sustainable Healthcare, ENGIE Impact, Oakland, California, USA
Terri Scannell, MBA
Senior Director, Social Responsibility and Community Benefit, Vizient, Inc., Irving, Texas, USA
Jodi D. Sherman, MD
Associate Professor of Anesthesiology, Yale School of Medicine; Associate Professor of Epidemiology in Environmental Health Sciences, Yale School of Public Health; Medical Director of Sustainability, Yale-New Haven Health, New Haven, Connecticut, USA
Originally published at https://catalyst.nejm.org on November 4, 2021.