Applying the Principles of the Toyota Production System to fix it – (not fully understood yet in Health Care)
This is an Executive Summary of the classic article below (2005), with the title above, by the editor of the Blog (in 2022, considering that the principles are still applicable). For the full version of the original publication, please, refer to the 2nd part of this post.
Fixing Health Care from the Inside, Today
Harvard Business Review
by Steven Spear
From the Magazine (September 2005)
Executive Summary
by Joaquim Cardoso MSc.
Chief Editor of “The Health Strategy Blog”
@ The Healthcare Operations Excellence Unit
March 14, 2022
What is the problem?
Health care safety expert Lucian Leape compares the risk of entering an American hospital to that of parachuting off a building or a bridge.
- As many as 98,000 people die each year in U.S. hospitals from medical error, according to studies reviewed by the Institute of Medicine.
- Other studies indicate that nearly as many succumb to hospital-acquired infections … for each person who dies from an error or infection, five to ten others suffer a nonfatal infection.
- With approximately 33.6 million hospitalizations in the United States each year, that means as many as 88 people out of every 1,000 will suffer injury or illness as a consequence of treatment, and perhaps six of them will die as a result.
- 250,000 patients suffering central-line infection in U.S. hospitals, with some 15% or more deaths-are only averages.
- The mortality rate (for central line infections) at just one PRHI member, LifeCare Hospitals of Pittsburgh, was a staggering 40%, and the cost for each case was anywhere between $25,000 and $80,000.
What is the cause of the problem?
- The problem stems partly from the system’s complexity, which creates many opportunities for ambiguity in terms of how an individual’s work should be performed and how the work of many individuals should be successfully coordinated into an integrated whole.
- The problem also stems from the way health care workers react to ambiguities when they encounter them. Like people in many other industries, they tend to work around problems, meeting patients’ immediate needs but not resolving the ambiguities themselves.
- As a result, people confront “the same problem, every day, for years” (as one nurse framed it for me) regularly manifested as inefficiencies and irritations-and, occasionally, as catastrophes.
Ambiguity and the Work-Around Culture
- Typically, care in a hospital is organized around functions. Issuing medication is the responsibility of a pharmacist, administering anesthesia of an anesthetist, and so on.
- The trouble is, that system often lacks reliable mechanisms for integrating the individual elements into the coherent whole required for safe, effective care.
What are the Characteristics of Operational Excellence Organizations, in other industries?
- But as industry leaders such as Toyota, Alcoa, Southwest Airlines, and Vanguard have demonstrated, it is possible to manage the contributions of dozens, hundreds, and even thousands of specialists in such a way that their collective effort not only is capable and reliable in the short term but also improves steadily in the longer term.
- These companies create and deliver far more value than their competitors, even though they serve the same customers, employ similar technologies, and use the same suppliers.
- Operating in vastly different industries, they have all achieved their superior positions by applying, consciously or not, a common approach to operations design and management.
As argued in previous articles in Harvard Business Review, what sets the operations of such companies apart is the way they tightly couple the process of doing work with the process of learning to do it better as it’s being done.
- Operations are expressly designed to reveal problems as they occur. When they arise, no matter how trivial they are, they are addressed quickly.
- If the solution to a particular problem generates new insights, these are deployed systemically.
- And managers constantly develop and encourage their subordinates’ ability to design, improve, and deploy such improvements. (See the sidebar “Delivering Operational Excellence.”)
Delivery Operational Excellence
Four basic organizational capabilities, if properly developed and nurtured, deliver the kind of operational excellence exhibited at Toyota and companies like it:
- Work is designed as a series of ongoing experiments that immediately reveal problems.
- Problems are addressed immediately through rapid experimentation.
- Solutions are disseminated adaptively through collaborative experimentation.
- People at all levels of the organization are taught to become experimentalists.
Who is doing it in the Healthcare Industry?
The scale of the potential opportunities can be seen in the results of a number of projects the author has been following over the past five years at various hospitals and clinics in Boston; Pittsburgh; Appleton, Wisconsin; Salt Lake City; Seattle; and elsewhere.
Consider just one example. The CDC cites estimates indicating that bloodstream infections arising from the insertion of a central line (an intravenous catheter) affect up to 250,000 patients a year in the United States, killing some 15% or more. The CDC puts the cost of additional care per infection in the tens of thousands of dollars.
- Yet, two dozen Pittsburgh hospitals have succeeded in cutting the incidence of central-line infections by more than 50%; some, in fact, have reduced them by more than 90%.
- Rolled out throughout the U.S., these improvements alone would save thousands of lives and billions of dollars.
- Other hospitals have dramatically lowered the incidence of infections arising from surgery and of pneumonia associated with ventilators.
- Still others have improved primary care, nursing care, medication administration, and a host of other clinical and nonclinical processes.
All of these improvements have a direct impact on the safety, quality, efficiency, reliability, and timeliness of health care.
Were the methods these organizations employ used more broadly, the results would be extraordinary.
Other examples and results
In less than three years, using techniques adapted from the Toyota Production System, the Pittsburgh Regional Healthcare Initiative
- slashed the number of reported central line-associated bloodstream (CLAB) infections by more than 50%.
- The rate per 1,000 line days (the measure the hospitals use) plummeted from 4.2 to 1.9.
At Allegheny General Hospital alone
- the number of patients suffering from central-line infections declined from 37 in one year to six in the following year, and
- associated deaths fell from 19 to one.
In their quest to eliminate central line-associated bloodstream (CLAB) infections, the hospitals in the Pittsburgh Regional Healthcare Initiative instituted a plethora of small process enhancements that together added up to dramatic improvement.
Life Care Hospitals
- 87% reduction in CLAB infections even as the number of lines placed rose by 9.75%.
Monongahela Valley Hospital
- Since 2002, zero infections in medical intensive care unit (MICU), 1 in cardiac care unit (CCU). (National average is 5 infections per 1,000 line days.)
- Zero urinary tract infections and zero ventilator-associated pneumo-nias in MICU and CCU for 6 months.
UPMC Health System
- One MICU went without a CLAB infection for several months. System wide rate cut to 1.2 infections per 1,000 line days.
Allegheny General Hospital
- Infections down from 37 in 2003 to 6 in 2004; deaths down from 19 to 1 in the same period.
- Direct cost reduction of $1.4 million.
The Health Care Opportunity
- What if the improvements to medical care described in this article were adopted by every hospital in the United States?
- This approach to operations can work wonders in health care, as the case studies show.
- But the potential savings in lives alone-never mind the improved quality and increased access to health care that the dollar savings will make possible-are surely ample justification for attempting the voyage.
The case of the pharmacy at the University of Pittsburgh Medical Center (UPMC) is a good example of that (see the long version).
- The pharmacy did manage to process batches of medication once every two hours instead of once every 24 hours.
- As a result, the incidence of missing medications in the wards dropped 88%.
- The savings in terms of pharmacy time and medication management were equally impressive.
– Time spent searching for medication fell by 60% and
– stock-outs fell by 85%-with no investment in technology.
- What’s more, a patient’s condition often changed before the IV was to be administered, so more than 30% of IV medications were returned to the pharmacy.
Institutionalizing Change
If one asks the question, Can the Toyota Production System be applied in health care? the quick answer is yes. The experiments just described all demonstrate that possibility.
- But to realize the full potential of TPS, senior health care leaders-hospital CEOs, presidents, chiefs of staff, vice presidents for patient care, medical directors, unit directors, and the like-will need to do more than provide support for pilot projects.
- They will need to embrace and embody TPS in their own work.
An example from the Virginia Mason Medical Center (VMMC) illustrates what it means for managers to try to master this new approach.
This commitment to process improvement has indeed increased quality and reduced costs.
- In 2002, for instance, 34 patients contracted pneumonia in the hospital while on a ventilator, and five of them died.
- But in 2004, only four such patients became ill, and just one died. Associated costs dropped from $500,000 in 2002 to $60,000 in 2004.
- And the overall number of professional liability claims plummeted from 363 in 2002 to 47 in 2004.
Improved efficiencies in labor, space, and equipment allowed VMMC to
- avoid adding a new hyperbaric chamber (saving $1 million) and
- even as it increased the number of patients its oncology unit treated from 120 to 188.* * *
Conclusion
- More to the point, the health care system is populated by bright, dedicated, well-intentioned people.
- They have already demonstrated a capacity to experiment and learn in order to master the knowledge and skills within their disciplines.
- One can imagine few people better qualified to master the skills and knowledge needed to improve processes that span the boundaries of their disciplines.

ORIGINAL PUBLICATION (full version)
Fixing Health Care from the Inside, Today
Harvard Business Review
by Steven Spear
From the Magazine (September 2005)
Last year on Christmas day, a 32-year-old Belgian woman celebrated the birth of a healthy daughter. Nothing remarkable about that, you might say, except that seven years prior, this same woman had been diagnosed with Hodgkin’s lymphoma. Because doctors feared that chemotherapy would leave her infertile, they surgically removed, froze, and stored her ovaries. Once her treatment was concluded, with her cancer sufficiently in remission, they thawed the tissue and returned it to her abdomen, after which she was able to conceive and deliver.
Such medical miracles-improvements in fertility treatment, cancer cures, cardiac care, and AIDS management among them-are becoming so commonplace that we take them for granted.
Yet, in the United States, the health care system often fails to deliver on the promise of the science it employs. Care is denied to many people, and what’s provided can be worse than the disease.
As many as 98,000 people die each year in U.S. hospitals from medical error, according to studies reviewed by the Institute of Medicine.
Other studies indicate that nearly as many succumb to hospital-acquired infections.1 The Centers for Disease Control and Prevention (CDC) estimates that for each person who dies from an error or infection, five to ten others suffer a nonfatal infection.
As many as 98,000 people die each year in U.S. hospitals from medical error, according to studies reviewed by the Institute of Medicine.
Other studies indicate that nearly as many succumb to hospital-acquired infections.
… for each person who dies from an error or infection, five to ten others suffer a nonfatal infection.
With approximately 33.6 million hospitalizations in the United States each year, that means as many as 88 people out of every 1,000 will suffer injury or illness as a consequence of treatment, and perhaps six of them will die as a result.
In other words, in the 15 to 20 minutes it might take you to read this article, five to seven patients will die owing to medical errors and infections acquired in U.S. hospitals and 85 to 113 will be hurt.
With approximately 33.6 million hospitalizations in the United States each year, that means as many as 88 people out of every 1,000 will suffer injury or illness as a consequence of treatment, and perhaps six of them will die as a result.
Health care safety expert Lucian Leape compares the risk of entering an American hospital to that of parachuting off a building or a bridge.
Health care safety expert Lucian Leape compares the risk of entering an American hospital to that of parachuting off a building or a bridge.
How can this be in the country that leads the world in medical science?
It’s not that caregivers don’t care. Quite the contrary: Health care professionals are typically intelligent, well-trained people who have chosen careers expressly to cure and comfort.
For that reason, perhaps, many policy makers and management scholars believe that the problems with American health care are rooted in regulatory and market failures.
They argue that institutions and processes mandated by law and custom are preventing demand for health care from matching efficiently to those most capable of providing it. In this view, the best treatment for what ails the U.S. health care system is strengthening market mechanisms-rewarding doctors according to patient outcomes rather than the number of patients they treat, for instance; increasing access to information about health care providers’ effectiveness to employers, individuals, and insurers; expanding consumer choice.
I won’t dispute the benefits of these reforms. The efficiency of health care markets may indeed be gravely compromised by poor regulation, and economic incentives should reinforce health care providers’ commitment to their patients. But I fear that the exclusive pursuit of market-based solutions will cause professionals and policy makers to ignore huge opportunities for improving health care’s quality, increasing its availability, and reducing its cost.
What I’m talking about here are opportunities that will not require any legislation or market reconfiguration, that will need little or no capital investment in most cases, and-perhaps most important-that can be started today and realized in the near term by the nurses, doctors, administrators, and technicians who are already at work.
What I’m talking about here are opportunities that will not require any legislation or market reconfiguration, that will need little or no capital investment in most cases,
and-perhaps most important-that can be started today and realized in the near term by the nurses, doctors, administrators, and technicians who are already at work.
The scale of the potential opportunities can be seen in the results of a number of projects I’ve been following over the past five years at various hospitals and clinics in Boston; Pittsburgh; Appleton, Wisconsin; Salt Lake City; Seattle; and elsewhere.
- Consider just one example. The CDC cites estimates indicating that bloodstream infections arising from the insertion of a central line (an intravenous catheter) affect up to 250,000 patients a year in the United States, killing some 15% or more.
The CDC puts the cost of additional care per infection in the tens of thousands of dollars.
… bloodstream infections arising from the insertion of a central line (an intravenous catheter) affect up to 250,000 patients a year in the United States, killing some 15% or more.
Yet, two dozen Pittsburgh hospitals have succeeded in cutting the incidence of central-line infections by more than 50%; some, in fact, have reduced them by more than 90%.
Rolled out throughout the U.S., these improvements alone would save thousands of lives and billions of dollars.
Yet, two dozen Pittsburgh hospitals have succeeded in cutting the incidence of central-line infections by more than 50%; some, in fact, have reduced them by more than 90%.
Rolled out throughout the U.S., these improvements alone would save thousands of lives and billions of dollars.
- Other hospitals have dramatically lowered the incidence of infections arising from surgery and of pneumonia associated with ventilators.
- Still others have improved primary care, nursing care, medication administration, and a host of other clinical and nonclinical processes.
All of these improvements have a direct impact on the safety, quality, efficiency, reliability, and timeliness of health care.
Were the methods these organizations employ used more broadly, the results would be extraordinary.
In fact, you could read an entire issue of HBR, even several, and during that time the number of fatalities would be close to zero. (See the exhibit “The Health Care Opportunity.”)
The Health Care Opportunity
What if the improvements to medical care described in this article were adopted by every hospital in the United States?
The following calculations estimate how many lives and how much money could be saved if actual rates (drawn from a number of conservative empirical studies) were cut in half — and if they were slashed by 90%.
To understand how the improvements were achieved, it is necessary to appreciate why such a gap exists between the U.S. health care system’s performance and the skills and intentions of the people who work in it.
The problem stems partly from the system’s complexity, which creates many opportunities for ambiguity in terms of how an individual’s work should be performed and how the work of many individuals should be successfully coordinated into an integrated whole.
The problem stems partly from the system’s complexity, which creates many opportunities for ambiguity in terms of how an individual’s work should be performed and how the work of many individuals should be successfully coordinated into an integrated whole.
The Belgian woman’s treatment, for instance, required a large number of oncologists, surgeons, obstetricians, pharmacists, and nurses both to perform well in their individual roles and to coordinate successfully with one another. Unless everyone is completely clear about the tasks that must be done, exactly who should be doing them, and just how they should be performed, the potential for error will always be high.
The problem also stems from the way health care workers react to ambiguities when they encounter them.
Like people in many other industries, they tend to work around problems, meeting patients’ immediate needs but not resolving the ambiguities themselves.
As a result, people confront “the same problem, every day, for years” (as one nurse framed it for me) regularly manifested as inefficiencies and irritations-and, occasionally, as catastrophes.
The problem also stems from the way health care workers react to ambiguities when they encounter them.
Like people in many other industries, they tend to work around problems, meeting patients’ immediate needs but not resolving the ambiguities themselves.
As a result, people confront “the same problem, every day, for years” (as one nurse framed it for me) regularly manifested as inefficiencies and irritations-and, occasionally, as catastrophes.
The Characteristics of High Velocity Organizations
But as industry leaders such as Toyota, Alcoa, Southwest Airlines, and Vanguard have demonstrated, it is possible to manage the contributions of dozens, hundreds, and even thousands of specialists in such a way that their collective effort not only is capable and reliable in the short term but also improves steadily in the longer term.
But as industry leaders such as Toyota, Alcoa, Southwest Airlines, and Vanguard have demonstrated,
it is possible to manage the contributions of dozens, hundreds, and even thousands of specialists in such a way that their collective effort not only is capable and reliable in the short term but also improves steadily in the longer term.
These companies create and deliver far more value than their competitors, even though they serve the same customers, employ similar technologies, and use the same suppliers.
Operating in vastly different industries, they have all achieved their superior positions by applying, consciously or not, a common approach to operations design and management.
As I have argued in previous articles in Harvard Business Review, what sets the operations of such companies apart is the way they tightly couple the process of doing work with the process of learning to do it better as it’s being done.
what sets the operations of such companies apart is the way they tightly couple the process of doing work with the process of learning to do it better as it’s being done.
Operations are expressly designed to reveal problems as they occur. When they arise, no matter how trivial they are, they are addressed quickly.
If the solution to a particular problem generates new insights, these are deployed systemically.
And managers constantly develop and encourage their subordinates’ ability to design, improve, and deploy such improvements. (See the sidebar “Delivering Operational Excellence.”)
Delivery Operational Excellence
Four basic organizational capabilities, if properly developed and nurtured, deliver the kind of operational excellence exhibited at Toyota and companies like it:
- Work is designed as a series of ongoing experiments that immediately reveal problems.
- Problems are addressed immediately through rapid experimentation.
- Solutions are disseminated adaptively through collaborative experimentation.
- People at all levels of the organization are taught to become experimentalists.
Four basic organizational capabilities, if properly developed and nurtured, deliver the kind of operational excellence exhibited at Toyota and companies like it:
1.Work is designed as a series of ongoing experiments that immediately reveal problems.
In order to drive out any ambiguity, employees in industry-leading companies spell out how work is expected to proceed in extraordinary detail, especially for highly complex and idiosyncratic processes. This increases the chance that the employees will succeed because it forces them to make their best understanding of a process explicit. If they don’t succeed, spelling out what is expected increases the chance that problems will be detected earlier rather than later, since people will be surprised by the unexpected outcome. Such companies go even further by embedding tests into the work that show when what is actually happening is contrary to what was expected.
2.Problems are addressed immediately through rapid experimentation.
When something does not go as expected, the problem is not worked around. Instead, it is addressed by those most affected by it. Its ramifications are contained and prevented from propagating and corrupting someone else’s work. Causes are quickly investigated and countermeasures rapidly tested to prevent the problem from recurring. When those who first address a problem are flummoxed, the problem is quickly escalated up the hierarchy so that broader perspectives and additional resources are brought to its resolution.
3.Solutions are disseminated adaptively through collaborative experimentation.
When an effective countermeasure is developed, its use is not limited to where it has been discovered. But that doesn’t mean the countermeasure is simply rolled out as a cookie-cutter solution. Rather, people build on local insights into reducing defects, improving safety, enhancing responsiveness, and increasing efficiency by solving problems with colleagues from other disciplines and areas so that the countermeasure, and the process by which it was developed, is made explicit, can be emulated, and can be critiqued.
4.People at all levels of the organization are taught to become experimentalists.
Finally, managers at companies like Toyota don’t pretend that the ability to design work carefully, improve processes, and transfer knowledge about those improvements develops automatically or easily. Coaching, mentoring, training, and assisting activities constantly cascade down to ever more junior workers, thereby building exceptionally adaptive and self-renewing organizations.
This approach to operations can work wonders in health care, as the case studies in this article will show.
We will see examples of how health care managers and professionals have designed their operations to reveal ambiguities and to couple the execution of their work with its improvement, thus breaking free of the work-around culture.
We will also see how health care managers have transformed themselves from rescuers arriving with ready-made solutions into problem solvers helping colleagues learn the experimental method.
I won’t claim that moving to the new environment will be easy, given the complexities of the health care workplace.
It will probably take some time, as well, because changes will have to be introduced gradually through pilot projects so as not to disrupt patient care.
These changes will require serious commitment from health care managers and professionals at the highest levels.
But the potential savings in lives alone-never mind the improved quality and increased access to health care that the dollar savings will make possible-are surely ample justification for attempting the voyage.
This approach to operations can work wonders in health care, as the case studies in this article will show.
But the potential savings in lives alone-never mind the improved quality and increased access to health care that the dollar savings will make possible-are surely ample justification for attempting the voyage.
Let’s begin by taking a closer look at what lies behind the health care tragedies we so often hear about.
Ambiguity and the Work-Around Culture
Typically, care in a hospital is organized around functions. Issuing medication is the responsibility of a pharmacist, administering anesthesia of an anesthetist, and so on.
The trouble is, that system often lacks reliable mechanisms for integrating the individual elements into the coherent whole required for safe, effective care.
The result is ambiguity over exactly who is responsible for exactly what, when, and how.
Eventually a breakdown occurs-the wrong drug is delivered or a patient is left unattended.
Then, doctors and nurses improvise. They rush orders through for the right drugs, urge colleagues to find available room for patients, or hunt down critical test results.
Unfortunately, once the immediate symptom is addressed, everyone moves on without analyzing and fixing what went wrong in the first place. Inevitably, the problem recurs, too often with fatal consequences.
The trouble is, that system often lacks reliable mechanisms for integrating the individual elements into the coherent whole required for safe, effective care.
Consider the story of Mrs. Grant, which comes to us from a 2002 article by David W. Bates in the Annals of Internal Medicine.
A 68-year-old woman Bates called Mrs. Grant (all individuals’ names in this article are likewise pseudonyms) had been recovering well from elective cardiac surgery when, all of a sudden, she began to suffer seizures.
Her blood was drawn for testing, and she was rushed for a CT scan, which revealed no hemorrhage, mass, or other obvious cause.
When she was returned to her room, caregivers saw from her blood test results that she was suffering from acute hypoglycemia, and they tried unsuccessfully to raise her blood sugar level.
She quickly fell into a coma, and after seven weeks her family withdrew life support.
How could that have happened?
A subsequent investigation revealed that at 6:45 on the morning of the incident, a nurse had responded to an alarm indicating that an arterial line had been blocked by a blood clot, and he had meant to flush the line with an anticoagulant, heparin.
There was, however, no evidence that any heparin had been administered.
What investigators did find was a used vial of insulin on the medication cart outside Mrs. Grant’s room, even though she had no condition for which insulin would be needed.
Investigators concluded that the nurse had administered insulin instead of heparin and that this error had killed the patient.
In retrospect, the mistake was understandable. Insulin and heparin (both colorless fluids) were stored in vials of similar size and shape, with labels that were hard to read, and they were located next to each other on the cart.
Mrs. Grant’s tragedy illustrates both the ambiguity that typifies many health care environments and the drawbacks of a work-around culture.
The drugs were packaged, labeled, and stored the way they were because the people responsible for doing so did not understand how their decisions about such specifics might cause problems for the nurses administering the drugs.
As a consequence, safety depended heavily on nursing staff vigilance.
Given how fragmented and hurried nursing work is, that was asking a lot at the best of times.
In Mrs. Grant’s case, the timing of the mistake may have increased its likelihood, as the insulin was administered early in the morning, when the nurse might not have been fully alert, in a room that may have been dimly lit.
Mrs. Grant’s nurse was certainly not the first in this hospital to have confused insulin with heparin.
In fact, Bates (et al.) in a 1995 study found that for every death due to medication error there were ten injuries that weren’t fatal and 100 instances where harm was averted.
In other words, most of the time people make a mistake, they prevent it from harming the patient, mainly by catching themselves in time and replacing the wrong drug with the right one.
Because they usually correct themselves quickly, almost reflexively, they seldom draw attention to the error.
It is only after a patient dies or suffers a serious injury that the type of mistake and the factors contributing to it are subject to serious scrutiny.
It is only after a patient dies or suffers a serious injury that the type of mistake and the factors contributing to it are subject to serious scrutiny.
Not all medical errors are the result of individuals failing in the face of challenges presented by confusing situations.
Take the case, investigated by the Centers for Medicare & Medicaid Services, of a five-year-old boy who had electrical sensors surgically implanted in his brain to treat his epilepsy.
Six hours after the operation, seizures began to rack the boy’s entire body; anticonvulsant medication needed to be administered immediately.
Yet even though several neurosurgeons, neurologists, and staff members from the medical intensive care unit (MICU) were either in the room, on call nearby, or at the end of a telephone, too little medication was administered too late.
The boy suffered a heart attack 90 minutes into the seizures and died two days later.
When the investigators asked the doctors and nurses involved how the boy could have died surrounded by so many skilled professionals, they all explained that they had assumed at the time that someone else was responsible for administering the drugs.
The MICU staff thought that the neurologists were in charge.
The neurosurgery staff thought the MICU and neurologists were responsible.
The neurologists thought the other two services had the lead.
Those on the phone deferred to those at the patient’s bedside.
Each of the professionals had probably been involved in hundreds of similarly ambiguous transfers of care.
In those cases, however, either the patient didn’t suffer an unexpected crisis or one of the parties involved stepped in and took a decisive lead.
Unfortunately, the success of those sometimes heroic work-arounds concealed the ambiguity that made them necessary in the first place.
When the investigators asked the doctors and nurses involved how the boy could have died surrounded by so many skilled professionals, they all explained that they had assumed at the time that someone else was responsible for administering the drugs.
Nailing the Ambiguities
What can hospitals and clinics do to prevent such tragedies?
The experience of the pre surgery nursing unit at Western Pennsylvania Hospital (“West Penn”) in Pittsburgh shows how organizations can make the transition from an ambiguous environment filled with work-arounds to one in which problems become immediately apparent and are dealt with as they occur.
The experience of the pre surgery nursing unit at Western Pennsylvania Hospital (“West Penn”) in Pittsburgh shows how organizations can make the transition from an ambiguous environment filled with work-arounds to one in which problems become immediately apparent and are dealt with as they occur.
On a typical day, the hospital’s pre surgical nursing unit prepared some 42 patients for scheduled surgery.
On arrival, a patient registered with a unit secretary, who entered the person into the system. Then a nurse took the patient’s medical history and conducted a physical examination.
A critical part of this prepping job was drawing blood for testing, which provided essential information for the surgical team.
Sometimes, the examining nurse drew the blood; other times, she asked a technician to do it; still other times, if something intruded on the nurse’s attention, no one would do it.
The result of this catch-as-catch-can procedure was that, on average, the blood work for one in six patients failed to be completed before the patient was ready to go to the operating room.
This was costly in a number of ways. A delay in getting a patient to the OR meant idling OR staff, at an estimated cost of $300 per minute.
It also meant delaying care-even canceling it, in some instances-for a patient who had been fasting and was anxious about the procedure.
When the unit reviewed the steps used in drawing blood, it uncovered, and then eliminated, a series of ambiguities in the process in a systematic way.
First, though it was clear that blood needed to be drawn for every patient, it was often not clear to the nursing staff whether the procedure had already been done.
To eliminate this confusion, the unit introduced visual indicators to identify which patients still needed the procedure and which did not.
These indicators included stickers on charts and signs on the ends of beds, both of which could be deployed easily during the presurgical preparation.
But even when it was clear which patients needed blood drawn, it was not clear who should do it. The nurse? A technician?
To deal with this second ambiguity, the unit designated a particular staff member, whom we’ll call Mary, to be the sole person to draw blood from every patient.
Mary’s appointment had positive results: The number of prepped patients missing blood test results fell sharply.
Nonetheless, some patients were still ready for surgery before their tests were complete.
It turned out that even if Mary knew which patients needed their blood drawn, she didn’t always know soon enough to get results back in time for their surgery.
To give the lab the most time to process the sample, nurses agreed that blood should be drawn as soon as a patient was registered.
This improvement also reduced, but did not eliminate, the problem.
In investigating further incidents, the nursing staff found yet another degree of ambiguity. Although Mary now knew she was responsible for drawing blood once the patients were registered, she didn’t always know when the registration had been completed. There was no clear signal that Mary should begin her work.
To resolve this, Mary and the unit’s registration secretary specified a simple, reliable, and unambiguous visual signal-a card would be placed on a rack. If no cards were on the rack, no samples needed to be taken. If one card was on the rack, a patient had been registered and was ready to have a sample taken.
Two or more cards beginning to pile up on the rack was a clear sign that Mary was taking samples at a rate slower than patients were arriving.
Despite all these improvements, a few patients were still turning up for the OR without their blood work.
Mary and her colleagues took another look at their process. It was clear which patients needed to have blood drawn, who was responsible for drawing the blood, and when Mary needed to draw it.
What still wasn’t clear was where the procedure should take place. To eliminate this final ambiguity, the unit converted a small closet into a room for drawing blood.
Stored items were removed, the walls were painted, lighting was installed, supplies were stocked, and a comfortable chair was provided for patients. With this final change, the number of patients ready for the OR without blood work declined to-and stayed at-zero.
In addition to the blood-drawing initiative, Mary’s unit conducted a number of similar projects to improve the reliability of work through high-speed, iterative trials.
One such effort was targeted at improving patient comfort and dignity. In the past, the unit had moved patients as far along in presurgical preparation as possible to ensure that surgeons were never kept waiting.
This included getting patients to change into those uncomfortable, overly revealing hospital gowns well ahead of time, which meant that they had to wait around in public for an average of 25 minutes before being given a bed.
A team in the unit spent half a day piloting a number of innovations to allow patients to delay changing until a bed was free.
Team members tested out and then established signals to indicate which bed was to be available for whom, when. A changing area was created, equipped with various signs and directions designed to ensure that patients wouldn’t get lost or misplace their personal effects. Before choosing the area, the team tested different rooms and screen configurations to see how well they provided privacy and made it easy to change clothes. The changes made a considerable difference. The number of patients waiting in public in their gowns at any one time fell from as many as seven to zero. Now they could wait in their street clothes with family members until beds were ready.
West Penn’s improvements didn’t happen because frontline workers all of a sudden started avoiding work-arounds and instead paused to construct reliable countermeasures.
Much of the credit for the successes can be attributed to the problem-solving support provided by the unit’s clinical coordinator, Karen, whose role was redefined in the course of the projects.
West Penn’s improvements didn’t happen because frontline workers all of a sudden started avoiding work-arounds and instead paused to construct reliable countermeasures.
Much of the credit for the successes can be attributed to the problem-solving support provided by the unit’s clinical coordinator, Karen, whose role was redefined in the course of the projects.
Previously, she had been the person of last resort when unit staffers couldn’t construct their own work-arounds.
If they couldn’t get some needed paperwork, she got it; if lab tests were missing, she chased them down. Karen’s new responsibilities were very different. Staffers brought all problems, including those they could work around themselves, to her attention one by one, as they occurred, rather than after the fact (if at all) in a group. Once alerted to a problem, Karen worked with whoever had raised it to investigate the causes, develop a solution, and test and validate the changes. These were not ad hoc solutions-like putting pressure on the pharmacy to rush a particular order-but rather basic changes in the design of work that were meant to entirely prevent the problem from recurring.
In the highest-performing organizations, all workers-not just those on the front line-need to be coached …
…to learn how to reduce ambiguity systematically and how to continually improve processes through quick, iterative experiments.
Thus, to help find her way into the new approach, Karen had a mentor-Alex-who worked with her several days a week. A former hospital administrator, Alex had been trained in the principles of the Toyota Production System. Alex’s role was not to teach Karen how to apply to the hospital environment the widely used tools of TPS, such as andon cords or kanban cards, but rather to teach her how to develop analogous problem-solving techniques and tools that took into account the idiosyncrasies of her unit.
In the year after Karen’s role was redefined, her unit identified and tackled 54 separate problems-about one a week.
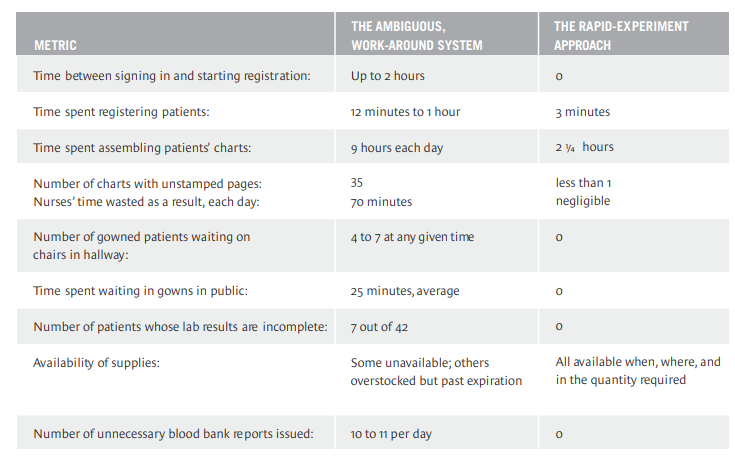
These varied in scope, impact, and time involved, but each followed the approach I’ve just described. As the table “Eliminating Ambiguity and Work-Arounds” shows, a systematic approach to eliminating problems need not take any more time than a temporary work-around.
But see how much time was saved-and how much patient care improved-when people at Western Pennsylvania Hospital stopped working around problems, and ambiguities in work processes were systematically eliminated through a series of rapid experiments facilitated by a manager.
Eliminating Ambiguity and Work-Arounds
In the moment, it may seem that when you are faced with a problem, the most effective thing to do is work around it as quickly as possible particularly when lives are in the balance.
But see how much time was saved — and how much patient care improved — when people at Western Pennsylvania Hospital stopped working around problems, and ambiguities in work processes were systematically eliminated through a series of rapid experiments facilitated by a manager.
Big Gains Through Small Changes
The changes I’ve described at West Penn were individually small, but taken together they led to marked improvement in the presurgical unit’s performance.
That’s also characteristic of change at Toyota: People don’t typically go in for big, dramatic cure-alls.
Instead, they break big problems into smaller, tractable pieces and generate a steady rush of iterative changes that collectively deliver spectacular results. This determination to sweat the small stuff underlies the remarkable reduction in central line-associated bloodstream (CLAB) infections achieved by the hospitals participating in the Pittsburgh Regional Healthcare Initiative (PRHI).
Used to speed the delivery of medication, central lines are intravenous catheters placed in the blood vessels leading to the heart. Infections arising from this procedure exact a terrible cost.
The figures that I cited at the top of this article-250,000 patients suffering central-line infection in U.S. hospitals, with some 15% or more deaths-are only averages.
The mortality rate (for central line infections) at just one PRHI member, LifeCare Hospitals of Pittsburgh, was a staggering 40%, and the cost for each case was anywhere between $25,000 and $80,000.
The mortality rate (for central line infections) at just one PRHI member, LifeCare Hospitals of Pittsburgh, was a staggering 40%, and the cost for each case was anywhere between $25,000 and $80,000.
The CDC has developed guidelines for the placement and maintenance of central lines. But as the PRHI professionals realized, the guidelines are generic to all hospitals and do not take into account the idiosyncratic factors of patient, place, and worker that are the root causes of individual infections. To improve their central-line processes, therefore, the PRHI hospitals decided to identify all the potential sources of central-line infection and all the local variations. As a result, the countermeasures these hospitals generated were tailored to the caseload, staffing, and special requirements of individual institutions and units. Nevertheless, the hospitals developed their countermeasures in the same way that Mary, Karen, and their colleagues did at West Penn. They responded swiftly to individual problems, testing a variety of possible solutions quickly, and those more senior took on the responsibility of enabling those more junior to succeed in the design and improvement of the work.
At Monongahela Valley Hospital, for example, a team of infection control experts documented every line placement to identify all variations and their shortcomings.
They carefully monitored all line insertions, dressing changes, medication administrations through the line, and blood draws for even the minutest breaks in technique and sterility. Each time the team observed a problem with the process, it would immediately develop and test some kind of countermeasure.
Like the innovations developed at West Penn, the countermeasures these hospitals developed were all aimed at removing ambiguity and increasing specificity in the same way-specifically, at four levels of system design: system output, responsibility, connection, and method. As they did at West Penn, the changes at the PRHI hospitals were designed to make crystal clear
For instance, several hospitals required that the central lines in all new admissions be replaced, since the histories of those lines were not known, thus simplifying output. To ensure that lines were properly placed, some units assigned responsibility only to those who had been specifically trained in each hospital’s most up-to-date techniques (while expanding the size of that group through additional training).
In terms of connections, visual signals, such as stickers, were added to patients’ charts and beds to trigger the removal of catheters sooner rather than later. Other such signals were used to indicate when a catheter should be moved from a place on the body known to have a high risk of infection to a lower-risk area and to otherwise clarify when lines had to be maintained or replaced. Transparent dressings were used to make it easier to tell whether a wound site was healthy or not.
As for methods, changes were made in disinfectant materials and techniques, and the kits in which line maintenance supplies came were repeatedly modified. (One alteration was to pack gloves on the top of the kit so that people would not contaminate other components in getting at the gloves.) Tests were made of various sized surgical drapes to determine which were not so small as to be ineffective or so big that they were knocked out of place when patients moved.
The results of the initiative were impressive. At Allegheny General Hospital alone, the number of patients suffering from central-line infections declined from 37 in one year to six in the following year, and associated deaths fell from 19 to one. (To see the cumulative effect, see the exhibit “Combining Countermeasures Has a Big Effect.”)
In their quest to eliminate central line-associated bloodstream (CLAB) infections, the hospitals in the Pittsburgh Regional Healthcare Initiative instituted a plethora of small process enhancements that together added up to dramatic improvement.
Combining Countermeasures Has a Big Effect
In their quest to eliminate central line-associated bloodstream (CLAB) infections, the hospitals in the Pittsburgh Regional Healthcare Initiative instituted a plethora of small process enhancements that together added up to dramatic improvement.
Life Care Hospitals
Countermeasure
- Avoid femoral lines because of increased infection risk.
- Change type of disinfectant.
- Use transparent dressings to improve visibility of wound to caregivers and reduce the need for physical manipulation as part of inspection.
- Call out every hand-washing lapse.
- Have nurses ask doctors each day if catheters can be removed or placed in lower-risk sites.
- Change lines for all new admissions, since history of current line is not known.
- Report every infection to the CEO every day, and investigate each one immediately.
Result
- 87% reduction in CLAB infections even as the number of lines placed rose by 9.75%.
Monongahela Valley Hospital
Countermeasure
• Require that kits always be complete so that practitioners can always don full protective garb.
• Require the lab to call the moment a positive culture is identified; initiate a root cause analysis immediately.
• Avoid femoral lines.
Result
- Since 2002, zero infections in medical intensive care unit (MICU), 1 in cardiac care unit (CCU). (National average is 5 infections per 1,000 line days.)
- Zero urinary tract infections and zero ventilator-associated pneumo-nias in MICU and CCU for 6 months.
UPMC Health System
Countermeasure
• Ensure hand-washing compliance.
- Improve barrier kits and use them in a consistent manner.
- Allow medical residents to place lines only with supervision until they all are formally trained.
Result
One MICU went without a CLAB infection for several months. System wide rate cut to 1.2 infections per 1,000 line days.
Allegheny General Hospital
Countermeasure
• Investigate each infection as it’s discovered.
• Remove all femoral lines within 24 hours.
• Prohibit rewiring of dysfunctional lines.
• Remove all catheters for transferred patients.
• Use biopatch dressings for lines that are expected to be in place for two weeks or more.
Result
Infections down from 37 in 2003 to 6 in 2004; deaths down from 19 to 1 in the same period.
Direct cost reduction of $1.4 million.
Simulation and Experiment
On any given day, Toyota employees engaged in design and production will be conducting some kind of simulation or experiment with workers and managers, repeatedly figuring out how to test ideas as quickly and inexpensively as possible.
People bolt what they would otherwise weld, tape what they would otherwise bolt, and just hold in place what they would otherwise tape. The objective is to compress the time between when an idea is formulated and when it is tested.
The pharmacy at the University of Pittsburgh Medical Center (UPMC) case!
The pharmacy at the University of Pittsburgh Medical Center (UPMC) South Side hospital used this approach in identifying and solving problems with its medication delivery process.
The pharmacy was supposed to make timely deliveries of medication throughout the hospital so that nurses could administer drugs to their patients according to the appropriate schedule. But when nurses went to get the medications, they often found that what they needed was missing. This triggered work-arounds. Nurses would interrupt their work to call the pharmacy, requiring pharmacy staff to stop what they were doing to track down orders: Had they been received? Had they been entered? Had they been prepared? Had they been delivered? Where was the missing medication? How quickly could it be rushed to the person needing it? Tracking down a missing medication, with all the attendant interruptions, could consume hours of nurse, pharmacist, and technician time.
The problem, the pharmacy realized, was that medication administration was done in batches. Physicians would make rounds early in the morning-before office hours or surgery-and follow up throughout the day. As patients’ conditions changed, doctors would write further orders for medication, which would be collected and delivered periodically to the pharmacy. There, pharmacists would enter the orders into the computer system, their expertise allowing them to identify potential problems with dosage, interactions, allergies, and the like. Orders would accumulate in the computer system throughout the day and then be printed out for all patients in the late afternoon. The next day, the pharmacy staff would begin filling these orders, assembling the proper mix and volume for each patient. This work would be completed in the early afternoon, at which point, a delivery technician would bring the completed orders to the nursing units. In view of the 12 to 24 hours that elapsed between the writing and the filling of an order, it was quite likely that medication needs would change, triggering work-arounds to get patients the right medicines, as well as a lot of unnecessary work restocking the old orders and making sure that patients were not billed for drugs they no longer needed.
The temptation in these situations is to brainstorm your way to an answer, with everyone proposing solutions drawn from his or her personal experience. But this was not the approach chosen here. As a first step in determining how to fix the medication preparation process, the pharmacy staff sat down as a group to determine what demands the nursing units were actually placing on the pharmacy. They counted out the previous day’s orders, divided that by the number of hours the pharmacy operated, and concluded that if the pharmacy were operating at the pace at which medication was being consumed, it would have to produce and deliver one order every three minutes. This gave them a concrete goal-instead of asking what changes they needed to make the process “better,” they asked what specifics prevented them from performing perfectly.
To answer that question, they set up a simulation. One pharmacist and one technician were lined up in the pharmacy, and every three minutes they were handed one order, which they tried to fill. This being an experiment, the staff used the previous day’s orders, not that day’s, and they delivered the medication into a cardboard box rather than having a delivery technician bring the medication all the way to the nursing unit. A stopwatch was started, a colleague handed the pair the first order, and they filled it. Three minutes later, the pharmacist and technician were handed a second order, which they filled. They were handed a third order, but before they could complete the work of finding the medication in inventory, taking out the right sized dose, labeling it, checking it, and bagging it, the three-minute interval had elapsed, and they were handed the fourth order.
At this point, they halted the experiment and asked themselves: “Why couldn’t we fill the third order?” This question was critical, and semantics mattered. Asking “Why didn’t you do your work?” elicits a very different response, typically a defensive explanation about how hardworking someone is, how he isn’t trying to fail, and so on. Asking why one couldn’t fill the order elicits a specific impediment, such as some ingredient being stored too far away or someone’s handwriting being too hard to read.
In this case, the pair realized that they couldn’t fill the order because the medication they were seeking couldn’t be found, and by the time they were done searching for it, their time was up. That very specific reason was recorded-”medicine X was in an uncertain location”-and the experiment resumed. A new order was handed to the team, and it was filled. Three minutes passed. Another order, another successful delivery to the cardboard box. Three more minutes. Another order-and another problem. When one of them tried to take a label off the printer, it jammed, delaying the process and preventing the team from keeping pace-another specific problem to be solved. The process of trying to fill one order every three minutes continued throughout the morning, and by the lunch break the experimenters had dozens of very specific answers to why the pharmacy couldn’t fill each order in time.
Some of the problems were easy to fix, such as storing drugs according to how frequently they were used rather than alphabetically. Others were more complicated, such as changing the timing at which drugs left the pharmacy, the delivery route technicians took through the hospital, and the way orders were placed with distributors. But simple or complex, the changes had a big cumulative impact. The pharmacy was ultimately never able to process and deliver each order individually, largely because the doctors writing the orders tended to do so in batches as they made their rounds, and delivery techs could not run so many individual orders to their various destinations at the same time. But the pharmacy did manage to process batches of medication once every two hours instead of once every 24 hours. As a result, the incidence of missing medications in the wards dropped 88%.
The savings in terms of pharmacy time and medication management were equally impressive. Time spent searching for medication fell by 60% and stock-outs fell by 85%-with no investment in technology.
Overall medication inventory was reduced, and medication costs dropped because drugs were less likely to be lost, spoiled, or wasted. Under the old system, for instance, IV medications were delivered as much as 48 hours before they were actually needed. That was problematic because many IV medications had to be refrigerated or otherwise kept in a controlled fashion, taking up valuable storage space in nursing units.
What’s more, a patient’s condition often changed before the IV was to be administered, so more than 30% of IV medications were returned to the pharmacy.
Since some medications spoil quickly once mixed with a saline solution, the pharmacy staff was often obliged to throw out the returns. Under the new process, IV medications were prepared and delivered shortly before being needed, significantly reducing both waste and demands on storage in the wards.
The savings in terms of pharmacy time and medication management were equally impressive. Time spent searching for medication fell by 60% and stock-outs fell by 85%-with no investment in technology.
What’s more, a patient’s condition often changed before the IV was to be administered, so more than 30% of IV medications were returned to the pharmacy.
What happened after the UPMC South Side experiment was almost more interesting than the experiment itself. When OR support staffers at UPMC Shadyside hospital learned of the improvements at South Side, they tried to apply the same tools and practices. But they soon discovered that the South Side solutions were inappropriate because of differences in the two organizations’ work. So the Shadyside people visited South Side and walked through the simulation process I’ve just described.
As they did so, they came to see that what they needed to do was master the problem-solving process rather than the problem-specific solutions.
Accordingly, they set up a similar experiment at their own site, uncovered different problems, and found different solutions.
… they came to see that what they needed to do was master the problem-solving process rather than the problem-specific solutions.
The Model Line Approach
When organizations first analyze their problems, they are inevitably tempted to roll out their solutions throughout the organization by installing a common set of tools and procedures broadly and quickly.
But there are a couple of difficulties with that approach.
First, as Shadyside discovered, the solutions from one situation may not apply in another.
Second, the most effective changes-at West Penn, South Side, and elsewhere-are small ones, generated by rapid experiments. Draw too big a group into the initial deployment, and the experiments become unwieldy, requiring too many people to change too much of their work at the same time. After all, even a small nursing unit includes several nurses in each day, evening, and night shift, as well as fill-ins for weekends, vacations, and the like and dozens of doctors who can admit patients to the unit. Finally, what sets companies like Toyota apart is not their portfolio of existing solutions but their ability to generate new ones repeatedly. One way to hone that ability is through the “model line” concept-creating, essentially, a model of the production line, a small incubator within the larger organization in which people can develop and practice the ability to design and improve work through experiments, and managers can rehearse their roles in facilitating this ongoing problem-solving and improvement process.
Shadyside used the model line approach with great success in its efforts to raise several aspects of the quality of its care. Rather than swamp the staff with a large initiative, the hospital began with a few beds within a single nursing unit and at first addressed just one of the many problems affecting nurses’ ability to care for patients.
In less than three years, using techniques adapted from the Toyota Production System, the Pittsburgh Regional Healthcare Initiative slashed the number of reported central line-associated bloodstream (CLAB) infections by more than 50%. The rate per 1,000 line days (the measure the hospitals use) plummeted from 4.2 to 1.9.
In less than three years, using techniques adapted from the Toyota Production System, the Pittsburgh Regional Healthcare Initiative slashed the number of reported central line-associated bloodstream (CLAB) infections by more than 50%.
The rate per 1,000 line days (the measure the hospitals use) plummeted from 4.2 to 1.9.
Tracking down materials, services, and information case!
Like many hospitals, Shadyside found that its nurses spent a disproportionate amount of time nursing not the patients but the system-tracking down materials, services, and information.
One consistent aggravation was with patient-controlled anesthesia (PCA) pumps.
Nurses needed access keys to adjust dosages, but for security reasons the pharmacy had assigned the unit only a few keys, which were often hard to find. So, as a work-around, the nurses would go looking for the most recent user.
Nurses in each shift searched for keys to the narcotics cabinet on average 23 times, wasting 49 minutes a shift and delaying pain relief to patients.
In discussing the problem, the nurses quickly realized that the limited number of keys was the issue. A nurse needing a key would check it out with the unit secretary but often fail to return it when rushing to meet another patient’s needs. The solution piloted was to have a numbered key available for every nurse, which would be signed out at the beginning of the shift and signed back in only when the nurse left the unit or ended his or her shift. In this way, the pharmacy’s need to control drug access was satisfied without inconveniencing the nurses.
The time spent searching for keys was reduced to almost zero, and the practice was subsequently deployed throughout the hospital, saving an estimated 2,900 nurse-hours each year.
The patient fall case
The nurses in the unit then applied their problem-solving approach to another issue: patient falls.
An estimated 2% to 4% of patients fall during their hospitalization in the United States every year (which translates into 670,000 to 1.3 million individuals) and 2% to 6% of those spills (13,000 to 78,000) lead to injury.
At Shadyside, the average was one fall every 12 hours. When the nurses looked into the problem, they realized that they hadn’t made it clear who was at risk of falling. What’s more, patient escorts were not trained in helping patients in and out of beds or on and off gurneys. That meant escorts would leave patients to find a trained nurse. Bit by bit, the unit’s nurses introduced changes, in much the same way the West Penn team did. Whey they first arrived at the unit, patients were rated at risk or not. Escorts were taught how to safely transfer patients so that they wouldn’t have to leave patients unattended. Danger areas were clearly marked (for instance, labels that said, “Don’t leave me alone!” were placed by bedside toilets). Nurses and nurse assistants built into their work the regular inquiry, “Do you need to use the bathroom?” so patients wouldn’t try to get out of bed on their own. Sensors were placed on beds to indicate if a patient was trying to get out of bed unassisted. And patients who needed but arrived without walkers or canes were lent the equipment they needed. After the changes were introduced, the number of falls declined dramatically-at one point, the unit went 95 days without one.
The nurses’ success with PCAs and falls was not lost on the staff from the dietary department serving the same unit. The problem facing the dietitians was that they could not tell how well patients adhered to the dietary regimens appropriate for their medical conditions. Patients on restricted diets would cheat (“I can’t eat this tasteless mess: Honey, can you grab me a burger, fries, and shake from the cafeteria downstairs?”). Even if patients did stick to the regimen in the hospital, they often stopped when they left, potentially compromising their recovery.
After discussing the problem-solving approach with the nurses, the dietitians realized that they could use patient meals as a way to identify precisely which patients would need further education. Rather than restrict choices, they decided to let the patients in the unit pick from the hospital’s entire menu-a counterintuitive approach if your objective is to control what patients eat but not if your objective is to teach patients how to select wisely and discover when your efforts have not succeeded. Allowing patients to choose from the whole menu was coupled with counseling from dietary and nursing staff about what foods should be chosen or avoided. Menu selections were coded-with a “healthy heart” sticker, for example, to indicate low-fat options-to make it clear which choices were appropriate for the various restricted diets. Then, after patients ordered food, dietitians would compare the orders with the instructions in the patients’ charts. Inappropriate picks-say, a cardiac patient ordering a high-cholesterol meal-would be treated as problems, and dietary and nursing staff would visit every problem patient before the meal was even served to provide nutritional instruction. If, after repeated counseling, patients continued to make choices contrary to recommendations, dietary and nursing staff would inform their doctors, who could modify their postdischarge medication orders appropriately, changing, for example, the type or dosage of blood pressure medication for a patient who wouldn’t cut his sodium intake.
Conemaugh Health System in west central Pennsylvania used an interesting variant of the model line approach to reveal problems that spanned the boundaries of individual units and departments. To find out what was falling between the cracks, the hospital tracked the treatment of certain patients all the way from admission to discharge.
One patient had come for a cardiac catheterization following symptoms that included chest discomfort. Testing revealed no blockage, and the patient was scheduled for discharge. From the patient’s perspective, this was a happy outcome, but from the hospital’s perspective, the findings were sobering: The team dealing with the patient documented that fully 27 distinct and potentially dangerous problems had occurred. While none actually compromised the care given to this particular patient, team members didn’t want to leave the ambiguities that caused the problems in place to be worked around again, so they worked with the pharmacy, the lab, and other departments to resolve them.
Institutionalizing Change
If one asks the question, Can the Toyota Production System be applied in health care? the quick answer is yes.
The experiments I’ve just described all demonstrate that possibility. But to realize the full potential of TPS, senior health care leaders-hospital CEOs, presidents, chiefs of staff, vice presidents for patient care, medical directors, unit directors, and the like-will need to do more than provide support for pilot projects. They will need to embrace and embody TPS in their own work.
An example from the Virginia Mason Medical Center (VMMC) illustrates what it means for managers to try to master this new approach.
If one asks the question, Can the Toyota Production System be applied in health care? the quick answer is yes.
An example from the Virginia Mason Medical Center (VMMC) illustrates what it means for managers to try to master this new approach.
VMMC is a 300-bed, Seattle-based teaching hospital with 5,400 employees and 400 physicians who admit some 16,000 patients a year and serve more than a million outpatients at ten sites.
VMMC’s management first became interested in TPS in 2001, after executives from local businesses described the dramatic improvements they had achieved in quality, customer satisfaction, safety, staff satisfaction, and, not least, profitability.
At the time, VMMC was in sorry straits. The hospital was struggling to retain its best people, and issues of quality, safety, and morale were on everyone’s mind.
VMMC started by piloting a few projects along the lines I’ve described in previous sections. But managers didn’t really understand the potential of establishing a continuously self-improving organization until the hospital’s chairman and its president, together with its professional and physician executives, went in 2002 on a two-week visit to Toyota factories, during which they all took part in an improvement project at a Toyota affiliate.
Impressed by the knowledge that it was possible to establish such an organization, VMMC formally adopted TPS as a model for its management system and began to train all of its staffers in its philosophy, principles, and tools. That included a public commitment to retain all full-time employees so that people would not feel that they were expected to improve themselves out of a job.
Since then, VMMC’s leadership has taken a number of steps to reduce tolerance for ambiguity and work-arounds and to make change a regular part of work. To help institutionalize a role for process experts in an organization otherwise filled with experts within disciplines, VMMC created Kaizen Promotion Offices, which support the improvement efforts of its various divisions. To emphasize the idea of quick, constant change, VMMC has conducted several hundred rapid-improvement projects.
To make it easy not to work around problems, VMMC created a patient safety alert process, which allows any employee to immediately halt any process that’s likely to cause harm to a patient. There’s a 24/7 hotline for reporting problems, a “drop and run” commitment from leadership at the department-chief and vice-president levels to immediately respond to the reports and to exhibit a willingness to stop processes until they are fixed. To further bolster the connection between leadership and the “shop floor,” department chiefs and managers conduct safety walkabouts, asking staff to alert them to specific instances in the previous few days of events that prolonged hospitalization, caused a near miss, harmed a patient, or compromised the efforts of people to do their work.
Such alerts rose from three per month in 2002, the year the patient safety alert process started, to ten per month in 2003, to 17 per month in 2004. Despite the increase in the number of alerts, the average time to resolution declined from 18 days in 2002 to 13 in 2004.
This commitment to process improvement has indeed increased quality and reduced costs.
- In 2002, for instance, 34 patients contracted pneumonia in the hospital while on a ventilator, and five of them died.
- But in 2004, only four such patients became ill, and just one died. Associated costs dropped from $500,000 in 2002 to $60,000 in 2004.
- And the overall number of professional liability claims plummeted from 363 in 2002 to 47 in 2004.
Improved efficiencies in labor, space, and equipment allowed VMMC to avoid adding a new hyperbaric chamber (saving $1 million) and avoid moving its endoscopy suites (saving another $1 million to $3 million), even as it increased the number of patients its oncology unit treated from 120 to 188.* * *
So far, no one can point to a single hospital and say, “There is the Toyota of health care.” No organization has fully institutionalized to Toyota’s level the ability to design work as experiments, improve work through experiments, share the resulting knowledge through collaborative experimentation, and develop people as experimentalists. But there’s reason for optimism. Companies in a host of other industries have already successfully followed in Toyota’s footsteps, using common approaches to organizing for continuous learning, improvement, and innovation that transcend their business differences. And these approaches have been successful when piloted in health care.
More to the point, the health care system is populated by bright, dedicated, well-intentioned people. They have already demonstrated a capacity to experiment and learn in order to master the knowledge and skills within their disciplines. One can imagine few people better qualified to master the skills and knowledge needed to improve processes that span the boundaries of their disciplines.
A version of this article appeared in the September 2005 issue of Harvard Business Review.
Originally published at https://hbr.org on September 1, 2005.
About the author
Steven J. Spear is the author of the award-winning and critically acclaimed book, The High Velocity Edge.
He is a senior lecturer at MIT Sloan School of Management and is a Senior Fellow at the Institute for Healthcare Improvement.
He is also a founder of a consulting firm built on the tenets of his book, and of See to Solve Corp., a business process software company.
Expert on the ways that “high-velocity organizations” generate and sustain advantage, even in the most hyper-competitive markets, Spear has worked with clients spanning technology and heavy industry, software and healthcare, and new production design and manufacturing.
Spear’s 1999 Harvard Business Review article, “Decoding the DNA of the Toyota Production System,” is part of today’s lean manufacturing canon. “Fixing Healthcare from the Inside, Today” was an HBR McKinsey Award winner in 2005 and one of his four articles to win a Shingo Research Prize.
Spear helped develop and deploy the Alcoa Business System, which recorded hundreds of millions of dollars in annual operating savings, and he was integral in developing the “Perfecting Patient Care” system for the Pittsburgh Regional Healthcare Initiative.
He has published in the New York Times, the Boston Globe, the Annals of Internal Medicine, and Academic Medicine, and he has spoken to audiences ranging from the Association for Manufacturing Excellence to the Institute of Medicine.
Spear has a doctorate from Harvard Business School, a master’s in engineering and in management from MIT, and a bachelor’s degree in economics from Princeton.
TAGS: Patient Safety Crisis; Patient Safety Improvement; Indicadores da ANS, Continuous Process Improvement; Operations Excellence; Process Excellence; Toyota Production System; Lean Healthcare












