Financial Times
Andy Haines
OCTOBER 11 2021
A Covid ward in a California hospital. Healthcare’s contribution to plastic pollution has increased during the pandemic © Mario Tama/Getty Images
The warning could not be starker. “The science is unequivocal,” wrote the editors of over 200 international health journals in a simultaneously published call to action last month.
“A global increase of 1.5°C above the pre-industrial average and the continued loss of biodiversity risk catastrophic harm to health that will be impossible to reverse.”
“A global increase of 1.5°C above the pre-industrial average and the continued loss of biodiversity risk catastrophic harm to health that will be impossible to reverse.”
Preventing such a calamity is a task not only for the politicians who will soon gather in Glasgow for the UN’s COP26 climate change conference, but also for the world’s healthcare providers.
It is they who are already having to deal with the immediate effects of climate change on human bodies and minds.
But they must also recognise that they, too, have contributed to the problem — because healthcare systems are significant carbon emitters.
Preventing such a calamity is a task not only for the politicians … but also for the world’s healthcare providers.
But they must also recognise that they, too, have contributed to the problem — because healthcare systems are significant carbon emitters.
Climate change threatens health along multiple fronts. Heat is the most obvious danger: a recent study estimates that over one-third of heat-related deaths between 1991 and 2018 can be attributed to climate change.
By the second half of this century, 1bn people could be living in locations where physical labour is hazardous, even in the shade.
Wildfires are increasing in frequency and intensity in some regions, exposing large populations to toxic smoke.
… estimates are that … over one-third of heat-related deaths between 1991 and 2018 can be attributed to climate change.
Other risks are less direct. Crop yields could decline on average by 10 per cent or more from the 2050s, threatening food security, while greater concentrations of carbon dioxide could reduce the micronutrient content in crops.
Meanwhile, higher temperatures and a greater incidence of flooding will encourage the spread of food- and waterborne infections, and of mosquito-borne diseases, such as dengue and West Nile virus.
Other risks are less direct. Crop yields could decline on average by 10 per cent or more from the 2050s, threatening food security …
Meanwhile, higher temperatures and a greater incidence of flooding … and its consequences.

The World Bank estimates that, in the absence of effective climate action, more than 100m people could be forced back into poverty by 2030.
Hunger could spur migration and conflict. And the toll will not only be physical: research published last year indicates that common mental disorders may persist for long periods following droughts, floods and wildfires.
… in the absence of effective climate action, more than 100m people could be forced back into poverty by 2030.
… common mental disorders may persist for long periods following droughts, floods and wildfires.
Adaptation strategies offer some hope.
- The heat warning systems that some countries have adopted save lives while,
- in the Caribbean, climate-informed epidemic forecasting promises to protect people from dengue.
But health policymakers should beware of unintended consequences:
increased use of air conditioning, for example, could
- overload electricity grids and
- add to greenhouse gas emissions and other forms of pollution.
What is needed?
What is needed, above all, is greater effort to meet the Paris climate accord target of keeping the global average temperature increase to well below 2°C — and preferably less than 1.5°C — above pre-industrial levels.
Current progress is seriously inadequate, yet the value of the health benefits alone could substantially offset the costs of mitigation.
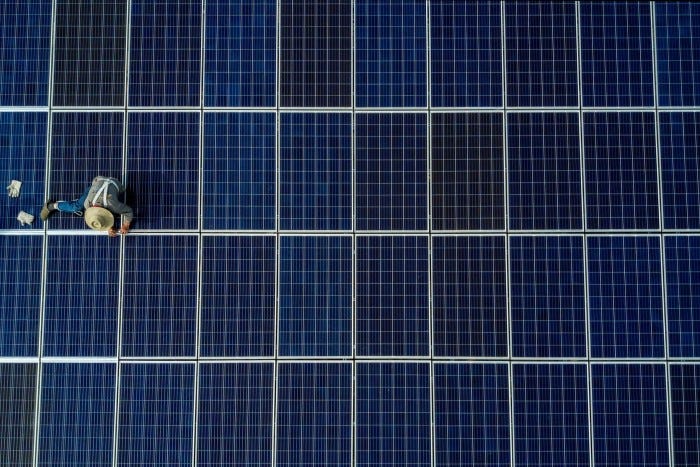
More rapid replacement of fossil fuels by clean renewable energy, for example, could prevent 3.6m premature deaths annually caused by outdoor air pollution.
More rapid replacement of fossil fuels by clean renewable energy, for example, could prevent 3.6m premature deaths annually caused by outdoor air pollution.
Or consider the food system, which currently contributes about 30 per cent of the world’s greenhouse gas emissions.
The health and climate benefits of reducing red meat production and increasing the consumption of fruit and vegetables are clear.
The EAT-Lancet Commission, a group of scientists whose report on sustainable eating came out in 2019, suggested that 10–11m premature deaths a year could be prevented by mid-century with a switch to a predominantly plant-based “planetary health” diet.
… 10–11m premature deaths a year could be prevented by mid-century with a switch to a predominantly plant-based “planetary health” diet.
Retrofitting houses with better insulation, draught-proofing and, where necessary, improved ventilation to reduce the build-up of household air pollutants could also reduce emissions and improve health.
Promoting public transport, walking and cycling can yield significant benefits through increased physical activity. Greater provision of green spaces in cities benefits physical and mental health.
Health professionals are already lobbying for progress in these areas: last year over 350 health organisations worldwide wrote to leaders of the G20 nations to urge them to put the environment at the centre of efforts to recover from the coronavirus pandemic.
Yet they also need to get their own houses in order.
- Research published by pressure group Health Care Without Harm in 2019 showed that the sector accounts for about 4.4 per cent of global greenhouse gas emissions — which, if it were a country, would make it the world’s fifth-biggest emitter.
- Healthcare also inflicts other types of environmental damage, such as plastic pollution, a problem exacerbated by the pandemic.
NHS England has committed to net zero direct carbon emissions by 2040 — through measures such as electrifying its fleet of vehicles — and by 2045 for indirect emissions.
It is already starting to work with suppliers to incentivise decarbonisation of their products.
All sorts of interventions can make a difference.
- Doctors can prescribe powder inhalers for asthma rather than those containing climate-active propellants, and avoid anaesthetic agents with big climate footprints such as desflurane.
- The Aga Khan Development Network has been building energy-efficient health facilities in low- and middle-income countries.
Even before Covid lockdowns necessitated consultations via Zoom, research showed that telemedicine could cut carbon emissions from patient transport.
Amid the horse-trading over emissions reduction targets and financial obligations that will take place at COP26, it may be easy to lose sight of climate change’s growing toll on human wellbeing.
The fact is that the health of the planet and of its human population are intimately entwined. In the fight against climate change, health workers are on the front line.
… the health of the planet and of its human population are intimately entwined. In the fight against climate change, health workers are on the front line.
About the author
Andy Haines, is professor of environmental change and public health at the London School of Hygiene and Tropical Medicine.
He co-chairs the Academy of Medical Sciences/Royal Society working group on health and decarbonisation, whose was published on October 14
Originally published at https://www.ft.com on October 11, 2021.












