The regimen is equally safe and effective — giving access to much more people
This is an excerpt of the paper below, with the topic above, highlighting the topic in question.
Cost containment analysis and access to treatment associated with adopting hypofractionated radiation therapy — from the Brazilian perspective
The Lancet — Regional Health, Americas
Prince Taylor; Marcus Simões Castilho; Gustavo Nader Marta 1
June 09, 2022
Executive Summary by
Joaquim Cardoso MSc
Health Transformation Institute
continuous transformation
for better health, care, costs, and universal health
July 3, 2022 (rogelcancer)
What is the background?
- While postoperative radiation therapy (RT) is commonly used to reduce recurrence and mortality, research has shown that moderately hypofractionated radiation therapy (HFRT) and 5-fraction HFRT are equally safe and effective and can reduce treatment costs.
What is the scope of the study?
- This study aimed to compare the cost of conventional RT (50Gy/25), moderately HFRT (40.05Gy/15), and 5-fraction HFRT (26Gy/5) for breast cancer patients in Brazil.
What are the results of the study?
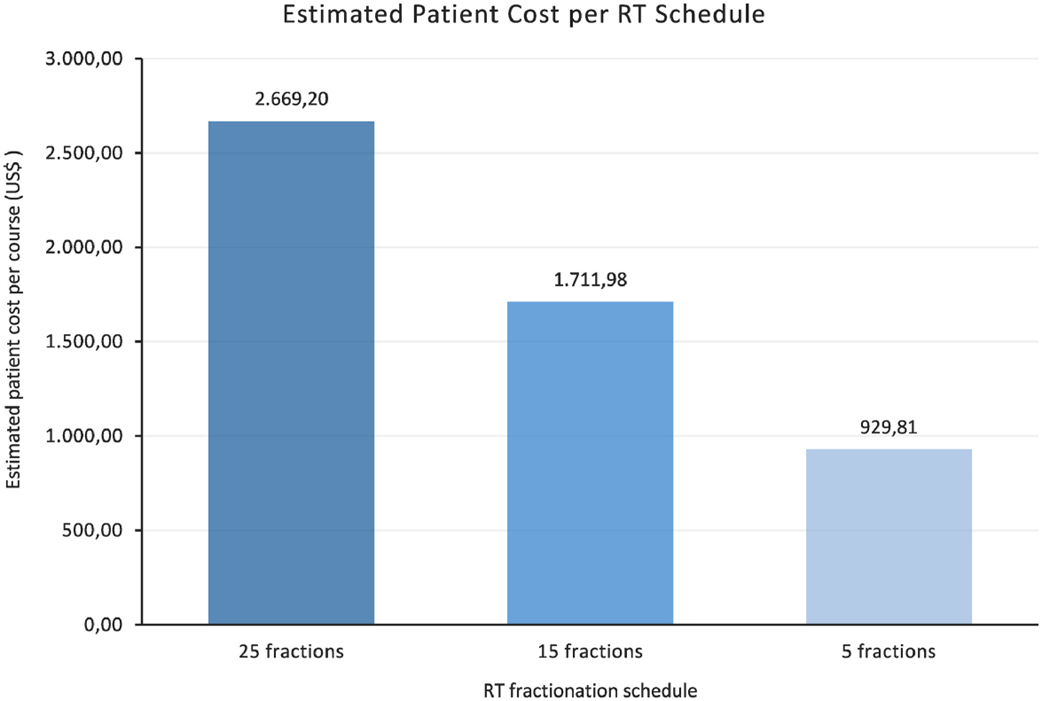
- As shown in Figure 1, the average cost per patient for a 25 fraction CFRT regimen is $2,669.20.
- The average cost per patient for a 15-fraction moderately HFRT regimen is $1,711.98, representing a reduction of 35.9% compared to the cost of the CFRT regimen.
- Lastly, for a 5-fraction ultra HFRT schedule, the average cost per patient is $929.81, representing a reduction of 65.1% compared to the cost of the CFRT regimen.
Figure 1 — Estimated average patient costs associated with CFRT (25 fractions), moderately HFRT (15 fractions), and ultra HFRT (5 fractions).
- While CFRT takes, on average, 5 weeks to complete treatment, moderately HFRT can complete this in only 3 weeks, and ultra HFRT can do so in only 1 week.
- As such, with significantly shorter treatment times, radiation oncology clinics can treat a significantly increased number of patients, as demonstrated by the findings of this paper.
- An important consideration, however, is that not all patients would be eligible for ultra HFRT, since it is generally only used in early-breast cancer patients and caution is still needed for patients who have breast implants.
- As such, the authors created a realistic model based on the Brazilian data regarding the prevalence of breast cancer stages, … considering treating 30% of patients with ultra HFRT and 70% of patients with moderately HFRT
Discussion
- While the cost analysis reveals promising cost savings for patients and the healthcare system, there are some concerns regarding the adoption of HFRT given current reimbursement models, which would reduce the lead to a revenue loss for oncology departments. 26
- Marta et al. 26 found that 77% of the countries investigated would experience a revenue loss through per-patient income ranging from 5%-40%.
- However, the adoption of HFRT is not only an evidence-based and international guideline-supported treatment but also holds the potential to drastically improve access to treatment, which is critical in emerging economies and resource-poor settings that are unable to meet their RT demand.
- Given these large-scale benefits, withholding evidence-based treatments such as HFRT, due to a potential loss of income for healthcare providers, would be highly unethical.
In conclusion
- In conclusion, the adoption of HFRT is associated with significant reductions in cost and treatment time, leading to a significant increase in RT access and treatment capacity.
- In combination with the previously established clinical safety and efficacy of HFRT for breast cancer patients, the positive cost and access implications suggest that the adoption of HFRT presents a promising solution to improve Brazilian breast cancer treatment capacity.
ORIGINAL PUBLICATION [excerpt]
Cost containment analysis and access to treatment associated with adopting hypofractionated radiation therapy — from the Brazilian perspective
The Lancet — Regional Health, Americas
Prince Taylor; Marcus Simões Castilho; Gustavo Nader Marta 1
June 09, 2022
SUMMARY
Background
Estimates show that breast cancer, the leading cause of cancer death in females worldwide, will continue to increase in incidence, highlighting the need for increased treatment capacity. While postoperative radiation therapy (RT) is commonly used to reduce recurrence and mortality, research has shown that moderately hypofractionated radiation therapy (HFRT) and 5-fraction HFRT are equally safe and effective and can reduce treatment costs. This study aimed to compare the cost of conventional RT (50Gy/25), moderately HFRT (40.05Gy/15), and 5-fraction HFRT (26Gy/5) for breast cancer patients in Brazil.
Methods and additional information
See the original publication
Results
As shown in Figure 1, the average cost per patient for a 25 fraction CFRT regimen is $2,669.20.
The average cost per patient for a 15-fraction moderately HFRT regimen is $1,711.98, representing a reduction of 35.9% compared to the cost of the CFRT regimen.
Lastly, for a 5-fraction ultra HFRT schedule, the average cost per patient is $929.81, representing a reduction of 65.1% compared to the cost of the CFRT regimen.
Table 1 details a cost breakdown of the estimated annual operating costs, capital costs, annual departmental costs, and average cost per patient, associated with each RT regimen.
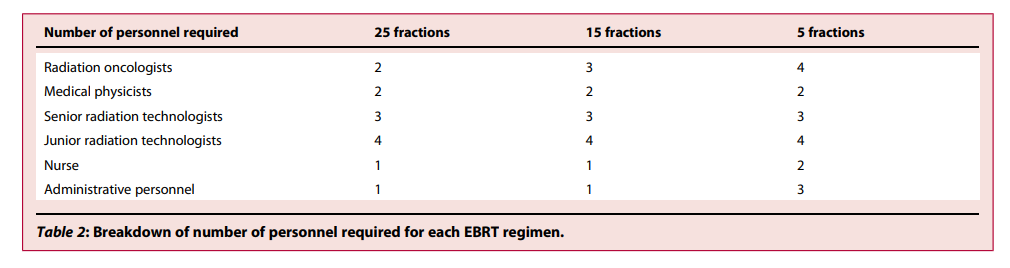
Table 2 lists the number of personnel required for each RT regimen, which led to changes in the annual operating costs associated with each EBRT regimen.
Figure 1 — Estimated average patient costs associated with CFRT (25 fractions), moderately HFRT (15 fractions), and ultra HFRT (5 fractions).
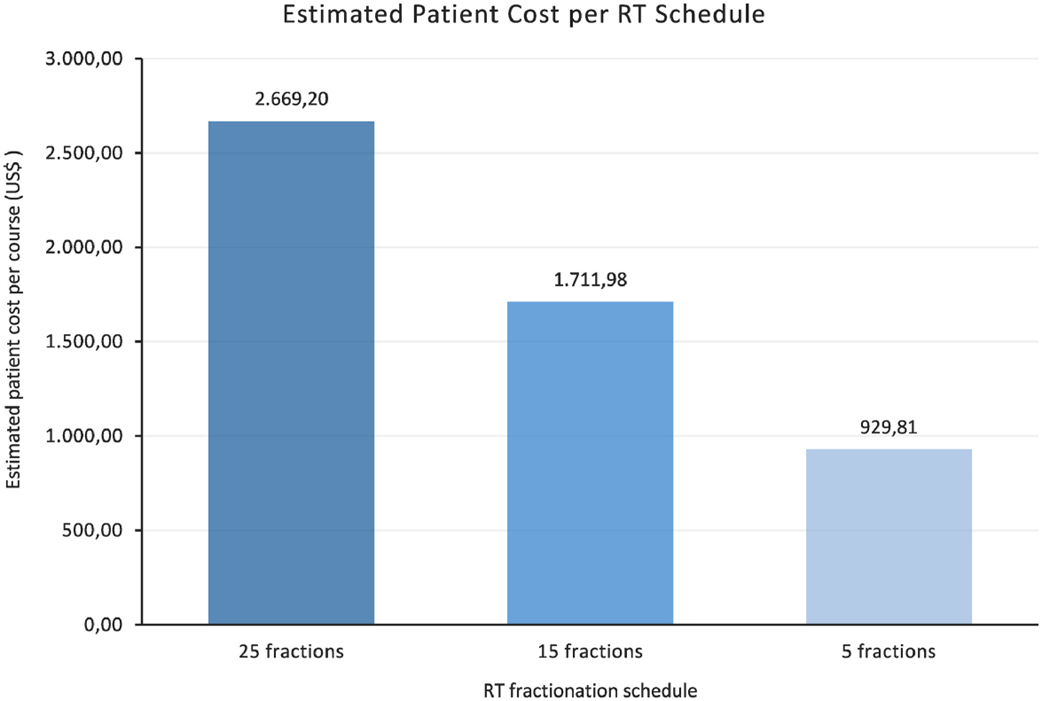
Table 1 — Cost breakdown of estimated annual operating costs, capital costs, annual department costs, and average patient cost associated with each EBRT regimen.
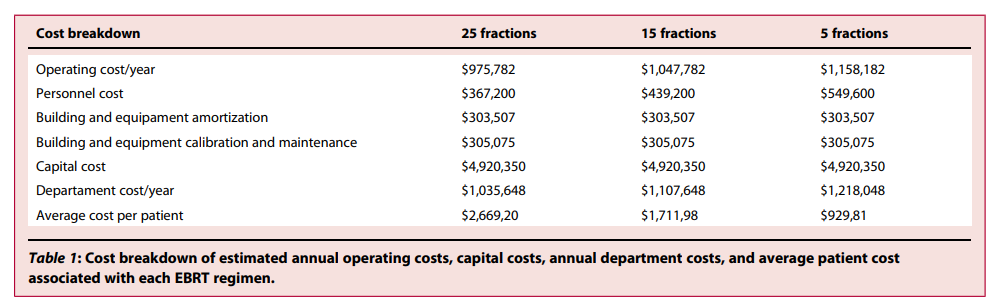
Table 2 Breakdown of number of personnel required for each EBRT regimen.
When these estimated patient costs are applied to all 61,178 patients, we can see a clear decrease in the annual estimated cost associated with switching from CFRT to moderate HFRT and a further decrease associated with switching to ultra HFRT.
The estimated cost of treating all patients with CFRT is $163,296,318, while the cost of treating all patients with moderately HFRT and ultra HFRT is $104,735,512 and $56,883,916.20, respectively.
An important consideration, however, is that not all patients would be eligible for ultra HFRT, since it is generally only used in early-breast cancer patients and caution is still needed for patients who have breast implants.
An important consideration, however, is that not all patients would be eligible for ultra HFRT, since it is generally only used in early-breast cancer patients and caution is still needed for patients who have breast implants.
As such, we created a realistic model based on the Brazilian data regarding the prevalence of breast cancer stages.
According to this model, the cost of treating 30% of patients with ultra HFRT and 70% of patients with moderately HFRT is $90,387,002.60.
Based on these estimated annual costs, the cost savings associated with switching from CFRT to moderately HFRT is $58,560,805.20, the cost savings associated with switching from moderately HFRT to ultra HFRT is $47,851,596.30, …
… the cost savings associated with switching from CFRT to ultra HFRT is $106,412,401, …
… the cost savings associated with switching from CFRT to the realistic model is $72,929,315.40, …
… and lastly, the cost savings associated with switching from moderately HFRT to the realistic model is $14,368,509.40.
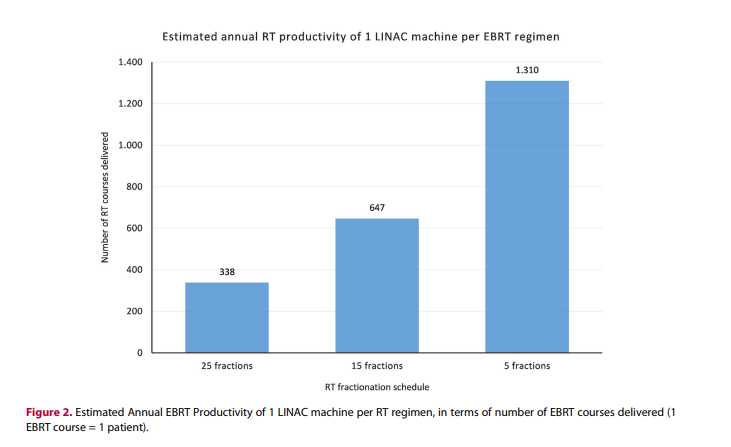
Regarding access to treatment, Figure 2 depicts the estimated annual productivity of 1 LINAC machine.
This graph demonstrates a significant increase in the numbers of patients that can be treated with the adoption of HFRT, with annual LINAC productivity of 388 patients for CFRT, 647 patients for moderately HFRT, and 1,310 patients for ultra HFRT.
Figure 2 — Estimated Annual EBRT Productivity of 1 LINAC machine per RT regimen, in terms of number of EBRT courses delivered (1 EBRT course = 1 patient).

Discussion
The present cost analysis found that HFRT is associated with reduced average estimated costs per patient, and a significantly increased access to treatment associated with HFRT, even after accounting for inefficiencies, such as increased first counselling sessions and scheduling issues, and additional time needed for image-guided RT.
Although we considered an increase in patient output for hypofractionated regiments, it is questionable if radiation departments in Brazil can deal with logistic issues regarding this increased patient turnover.
It is important to have adequate numbers of personnel, adequate transportation services, and an adequate referral structure in order to make it possible. 25 , 26
The estimated costs determined in this cost analysis are supported by a 2021 study conducted by Yaremko et al. 27 , which found similar estimated per-patient costs of CA$851.77 for the ultra HFRT FAST-Forward 1 regimen and $1,339.75 for the moderately HFRT regimen.
However, many of the patient costs reported in other studies are significantly higher.
This is primarily because many of these studies conducted their investigations using data from the US, which has higher patient costs, as compared to other upper-middle-income countries, and significantly higher patient costs compared to low-income countries and lower-middle-income countries.
For example, a US-Based Time-Driven Activity-Based Costing analysis conducted by Dziemianowicz et al. 25 found that accelerated whole breast irradiation, a form of HFRT which delivers 42.5 Gy in 16 fractions + a boost of 10 Gy in 4 fractions, costs a total of US$6,965, compared to $9,267 for CFRT. Unsurprisingly, the investigators found that a majority (86%) of the difference in cost between HFRT and CFRT was due to the lower cost of fewer daily fractions.
When we compare countries with different levels of development, the personnel salaries also play a more important role in differences in costs. Overall, while the estimated costs of each regimen vary significantly depending on the country of interest, the overall trend of significantly lower costs associated with HFRT, as compared to CFRT, is consistent among the literature.
In respect to the reviewed literature relating to cost considerations, a majority of the publications reported that HFRT was associated with significantly reduced patient and/or healthcare costs, supporting the findings of this present cost analysis. 28 , 29 , 30
However, while the cost analysis reveals promising cost savings for patients and the healthcare system, there are some concerns regarding the adoption of HFRT given current reimbursement models, which would reduce the lead to a revenue loss for oncology departments. 26
Marta et al. 26 found that 77% of the countries investigated would experience a revenue loss through per-patient income ranging from 5%-40%.
However, the adoption of HFRT is not only an evidence-based and international guideline-supported treatment but also holds the potential to drastically improve access to treatment, which is critical in emerging economies and resource-poor settings that are unable to meet their RT demand.
Given these large-scale benefits, withholding evidence-based treatments such as HFRT, due to a potential loss of income for healthcare providers, would be highly unethical.
As such, it is recommended that further cost investigations must be conducted to analyze the integration of HFRT to improve the uptake of HFRT from a financial perspective.
Given these large-scale benefits, withholding evidence-based treatments such as HFRT, due to a potential loss of income for healthcare providers, would be highly unethical.
As such, it is recommended that further cost investigations must be conducted to analyze the integration of HFRT to improve the uptake of HFRT from a financial perspective.
While this paper is important in conducting a cost analysis to compare the cost of various regimes in Brazil, it does have certain limitations.
A limitation regarding the cost analysis is the lack of use of a stringent model, such as a time-driven activity-based costing model or a Markov chain model.
The use of such models has been supported to aid in estimating the total cost of delivering RT based on the cost of various resources, such as personnel, space, equipment, materials, and utilities.
However, this present cost analysis used the IAEA’s EBRT Cost Estimator tool, which is a comprehensive and reliable tool that considers personnel salaries, working arrangements, treatment protocols and building and equipment costs. 23
Thus, the article is interesting in that it raises awareness of the topic and tries to evaluate it in terms of cost.
Nevertheless, these numbers/models, as stated earlier, are crude and may not reflect the reality even though the model works well.
Thus, the article is interesting in that it raises awareness of the topic and tries to evaluate it in terms of cost.
Nevertheless, these numbers/models, as stated earlier, are crude and may not reflect the reality even though the model works well.
Overall, the findings presented in the paper are significant because they indicate that the adoption of HFRT could save significant healthcare costs, which is advantageous for all economies, but especially crucial for emerging economies.
This is especially important in Brazil, whose public health system is currently unable to meet the national RT demand, meaning that the shortage of RT has led to thousands of preventable deaths. 2
Importantly, this present analysis is unique in that it not only compares CFRT and moderately HFRT but also includes the more novel ultra HFRT regimen.
Previous cost analyses, such as the one conducted by Irabor et al. 21 , are limited to consider the cost considerations of adopting moderately HFRT, rather than both moderately HFRT and ultra HFRT.
Additionally, the findings also indicate that the adoption of HFRT can drastically improve access to RT treatment for breast cancer patients, both directly, through shorter treatments, and indirectly through reduced costs.
Additionally, the findings also indicate that the adoption of HFRT can drastically improve access to RT treatment for breast cancer patients, both directly, through shorter treatments, and indirectly through reduced costs.
While CFRT takes, on average, 5 weeks to complete treatment, moderately HFRT can complete this in only 3 weeks, and ultra HFRT can do so in only 1 week.
While CFRT takes, on average, 5 weeks to complete treatment, moderately HFRT can complete this in only 3 weeks, and ultra HFRT can do so in only 1 week.
As such, with significantly shorter treatment times, radiation oncology clinics can treat a significantly increased number of patients, as demonstrated by the findings of this paper.
It is also important to discuss that, from the patient side, this reduces the number of trips to the clinics- which will have a tremendous impact for people needing to travel long distances (sometimes to other states) to access treatment.
Given the results of the analysis, due to the cost and access benefits associated with HFRT, radiation oncology departments should consider adopting the use of this shorter course of treatment for eligible breast cancer patients.
The adoption of HFRT could significantly decrease the number of preventable deaths attributed to the shortage of RT in Brazil.
Additionally, while Brazil was the country of focus in this present study, this cost analysis methodology could be replicated and extrapolated to various countries.
There are many regions of the world which are struggling to meet their national RT demand, and as such, it is recommended that further studies should be conducted to investigate the local implications of adopting HFRT, to facilitate the uptake of evidence-informed treatment strategies that hold the potential to improve healthcare capacity.

In conclusion
In conclusion, the adoption of HFRT is associated with significant reductions in cost and treatment time, leading to a significant increase in RT access and treatment capacity.
In combination with the previously established clinical safety and efficacy of HFRT for breast cancer patients, the positive cost and access implications suggest that the adoption of HFRT presents a promising solution to improve Brazilian breast cancer treatment capacity.
References and additional information
See the original publication https://www.thelancet.com
About the authors & affiliations
Prince Taylor,a,b
Marcus Simoes Castilho, c and
Gustavo Nader Marta d,e *1
a Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
b Department of Global Health, McMaster University, Hamilton, ON, Canada
c Division of Radiotherapy, Radiocare — Hospital Felicio Rocho, Belo Horizonte, MG, Brazil
d Department of Radiation Oncology, Hospital Sírio-Libanes, Sao Paulo, SP, Brazil
e Latin America Cooperative Oncology Group (LACOG), Brazil