Bertalan Meskó, MD, PhD
April 8, 2022
According to a series of studies published in the Lancet, the wealthiest American women live approximately 10 years longer than their poorest counterparts, and this gap widens to a shocking 14,5 years for men.
With these figures, the USA is the most unequal country in terms of health outcome among the OECD countries. And the outlook is not great either. Researchers warn us that this difference we now see between the top and bottom 1% is only going to grow. Without intervention, the difference in life expectancy between the richest and poorest 20% will expand to 10 years in a generation’s time.
According to a series of studies published in the Lancet, the wealthiest American women live approximately 10 years longer than their poorest counterparts, and this gap widens to a shocking 14,5 years for men.
There are differences between the developed world in how much inequity you face when accessing healthcare. Some countries manage the issue better.
While 39% of Americans with below-average income reported not seeing a doctor for a medical problem because of its cost, this compares to a 7% figure of low-income Canadians and 1% of those in the UK.
While 39% of Americans with below-average income reported not seeing a doctor for a medical problem because of its cost, this compares to a 7% figure of low-income Canadians and 1% of those in the UK.
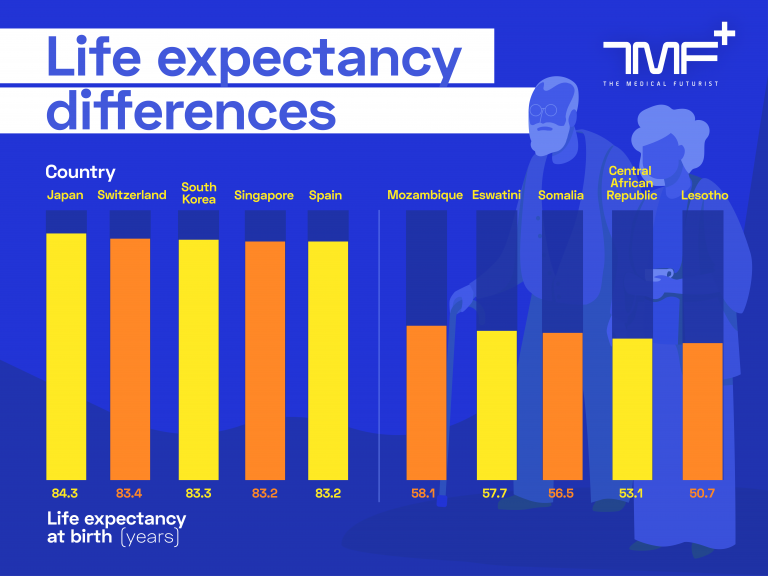
The real health gap: life expectancy at birth according to WHO. On the left the 5 countries with the highest figures. On the right the 5 countries with the lowest figures.
But of course, this is not just an OECD problem. Inequities are even more prevalent between rich and poor countries.
Based on the WHO’s figures, a Japanese newborn is expected to live 84,2 years, while a baby born on the same day in Lesotho will be dead before celebrating the 51st birthday.
This highlights the fact that the health gap is significantly wider between countries than within countries, even if US figures seem shocking at first.
Based on the WHO’s figures, a Japanese newborn is expected to live 84,2 years, while a baby born on the same day in Lesotho will be dead before celebrating the 51st birthday.
Money, money, and health literacy
The reasons for the existing and ever-widening health gap are quite easy to grasp. There are the well-known facts.
Lower income statistically means a higher prevalence of unhealthy habits, poorer diet, fewer medical visits, less money to afford healthcare services.
Lower income statistically means a higher prevalence of unhealthy habits, poorer diet, fewer medical visits, less money to afford healthcare services.
But there is another, often overlooked aspect: the difference between health literacy.
The CDC defines health literacy as: “the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others”.
But there is another, often overlooked aspect: the difference between health literacy.
A 2013 WHO report revealed that health literacy is a stronger predictor of the formation of the state of health than income, education or belonging to various ethnic groups.
And we are not talking just about individuals, as there is a definition for ‘Organisational health literacy’ as well.
That is “the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others”.
And we are not talking just about individuals, as there is a definition for ‘Organisational health literacy’ as well.
That is “the degree to which organizations equitably enable individuals

Brigding the gap with digital health tools
Let me start with yet another definition, and I promise, this will be the last one.
So, what is digital health? In this paper published by The Medical Futurist Institute it is summarised like this:
“The cultural transformation of how disruptive technologies that provide digital and objective data accessible to both caregivers and patients leads to an equal level doctor-patient relationship with shared decision-making and the democratisation of care”
The only thing we have a realistic chance to democratise is access to care. The goal is to come up with a system that provides healthcare to everyone, regardless of their financial situation, nationality or the language they speak.
The only thing we have a realistic chance to democratise is access to care.
This is not an easy feat though.
Currently, around 5 million healthcare workers are missing from the system according to the most optimistic estimate, and this figure is only expected to grow.
Thinking about accessing healthcare along the usual lines — I have a problem, I go to see the doctor — will obviously not work.
The gap between patients without healthcare access and the number of trained doctors is only going to widen. And can only be bridged with digital health tools.
The gap between patients without healthcare access and the number of trained doctors is only going to widen. And can only be bridged with digital health tools.
These solutions might lend a hand here. We are not able to involve a huge number of patients in the traditional way.
We can, however, involve them with remote health tools and A. I. chatbots, taking over the first line of contact.
We can, however, involve them with remote health tools and A. I. chatbots, taking over the first line of contact.
Building an arsenal to reach everyone
This opens up an avenue to globalised healthcare, an accessible, affordable arsenal built by digital health tools.
This opens up an avenue to globalised healthcare, an accessible, affordable arsenal built by digital health tools.
By now a vast number of tools, apps and solutions are available. Here are a few examples:
- Sensors and wearables generating data that were previously only accessible to hospitals, doctors or nurses. (Examples: blood glucose and EKG monitors, smart and fitness watches collecting data 24/7, pulse oximeters)
- Smart and connected devices for home use generating data valuable for the medical professionals. (Including medication management tools, contact sensors for the medical cabinet, movement sensors, sleep sensors)
- Remote solutions. (Including telehealth applications, remote consultation, A. I. chatbots, drone delivered services and solutions)
- Online and/or device-driven support for personal health management. (Including support for breaking nicotine addiction, managing epilepsy, overviewing dietary habits, training and exercise)
This is not the same as going to your doctor? Sure. But this is the next best thing we can come up with for millions and billions of people with currently zero access to health services if we can bridge the gap between the data and the user.
We have seen some good examples of that.
A company, Mucca Design re-invented blood test results in a way that they changed the basic list of results to a colourful and easily digestible infographic.
Text4Wellness and Mobilize4Fitness are mobile services that provide texts with health and wellness tips, reminders to exercise, inspirational quotes and information about health and wellness activities geared toward African-American women in the United States. It uses a convenient communication method and familiar language.
The Maxillofacial Department at Radboud University in the Netherlands invited patients to help design new care facilities which improve patient satisfaction.
As good as the weakest link
But let’s circle back to the question of health literacy and health gap. Studies also pinpoint that apps and wearables actually only benefit the rich. Why?
Studies also pinpoint that apps and wearables actually only benefit the rich.
The European health literacy survey (HLS-EU) found that every second person possesses limited health literacy.
Also, patients with lower health literacy rates are less likely to use the possibilities of eHealth.
The technological boom makes it unambiguous that digital health literacy has a wider aspect than the notion of classic health literacy.
The technological boom makes it unambiguous that digital health literacy has a wider aspect than the notion of classic health literacy.
“Digital health adds the requirement to be technically literate about computers and media. We are standing before an enormous challenge. Will technological transformation improve health literacy levels, or the contrary: will digital health deepen the already existing digital divide?”
The answer might lie in design thinking to improve health literacy, which most likely will have to happen un-digitally.
The answer might lie in design thinking to improve health literacy, which most likely will have to happen un-digitally.
Originally published at https://www.linkedin.com.
TAGS: Health Inequalities; Life Expectancy; Digital Health; Digital Health Tools; Health Strategies; Health Issues; Digital Divide; Access to Digital Health, Smart Home Devices; Health Literacy; Digital Health Literacy; Design Thinking