Philips
Henk van Houten, CTO Philips
Jun 14, 2021
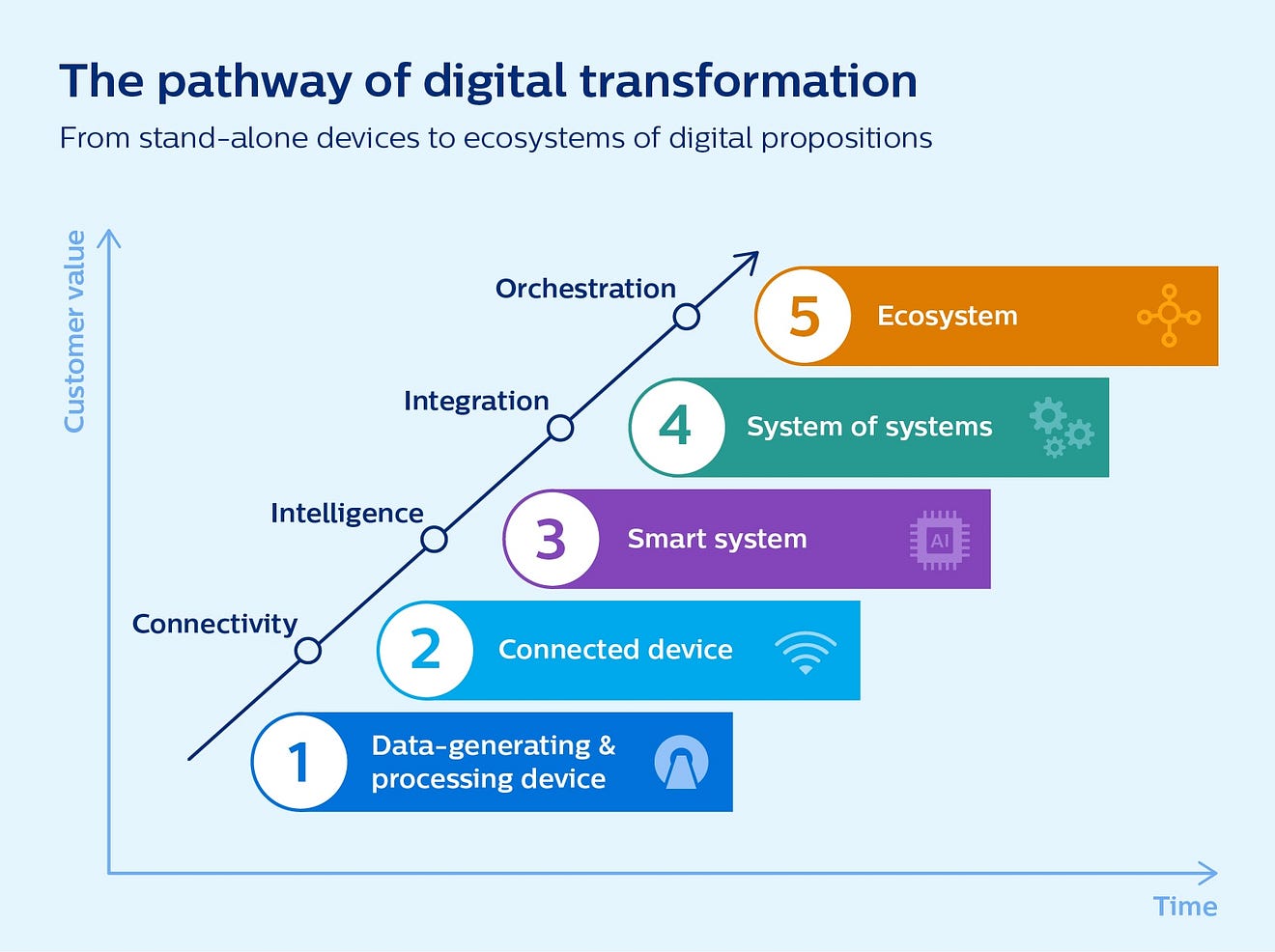
What do a 200-gram smartphone and a 4-ton MR machine have in common? Not much, at face value. But if we trace the past and future evolution of these two very different feats of modern technology, they actually follow surprisingly similar trajectories. Here’s why the comparison matters, and what it reveals for the future of healthcare.
I still remember the initial excitement of being able to talk to friends and family wherever I was. Early cell phones may have been somewhat cumbersome to use compared to today’s smartphones, but they represented a huge shift in how we went about our daily lives. The real breakthrough in smartphone technology, however, only came many years later, through a series of developments that upended the very nature of innovation.
First, there was the introduction of high-speed internet connectivity. This put the world at our fingertips, allowing us to find a nearby restaurant or to check when it’s going to rain while we’re on the go. From a technological perspective, connectivity also brought about another fundamental shift: it allowed for features of the smartphone to exist outside of the physical device itself — in the cloud. This enabled manufacturers to update and upgrade features over the air, and to introduce new ones over time, adding ever more value to their customers.
It’s hard to overstate how fundamental a change this was. What was once a static product, a device that offered the same fixed features until you replaced it with a new one, could now delight you with new services every time you picked it up.
Manufacturers then opened their platforms to others, introducing the first app stores. That’s when the pace of change accelerated exponentially. Third-party developers jumped on the opportunity to make a slew of new apps available. Digital ecosystem innovation was born, disrupting entire industries — from banking to music and photography. Today, there’s an app for everything. And thanks to AI, those apps keep getting smarter every day as they learn from ever-growing masses of data.
Our daily lives have changed profoundly as a result. What was once time-consuming and complex, is now fast and easy. Split and pay the bill after a night out with friends? Done with one press of the button. Looking to blur the background in your family snapshots? No need to be an experienced photographer. An app will do the trick for you.
More than ever, it makes me wonder: what would healthcare — an industry riddled with complexity — look like if we embraced the same digital best practices?
- How much more pleasant and frictionless could we make patient and staff experiences if we designed medical devices and systems with the same level of smartness and connectivity?
- How much more value could those systems and devices offer over their lifetime if we were able to update and upgrade them just as easily as our smartphones?
- And how much faster would we be able to innovate if we adopted the same ecosystem approach that has taken other industries by storm?
How much more pleasant and frictionless could we make patient and staff experiences if we designed medical devices and systems with the same level of smartness and connectivity as smartphones?
That’s where past and future innovations in magnetic resonance imaging (MRI) can serve as a telling example — because as far removed as an imaging exam room may seem from the world of smartphones, on closer inspection, a similar pattern of digital transformation is beginning to emerge.
Bringing MR into the connected world
Ever since the first commercial MR systems were launched in the early 1980s, millions of patients have benefited from the detailed images of the body these machines provide to help physicians diagnose everything from cancers, heart damage and spine injuries to brain abnormalities.
Yet initially, like early cell phones, MR systems were essentially designed as static, stand-alone products — revolutionary in what they made possible, but with limited connectivity or services beyond basic break-fix maintenance.
That began to change with the introduction of remote connectivity, which I like to think of as a first step in digital transformation. For example, we can now monitor and analyze over 500 parameters on an MR machine remotely, 24/7, using predictive analytics to identify when certain hardware parts may need maintenance or replacement. As a result, 30% of service cases can be resolved before downtime is caused — preventing avoidable interruptions to clinical practice and unnecessary patient delays.
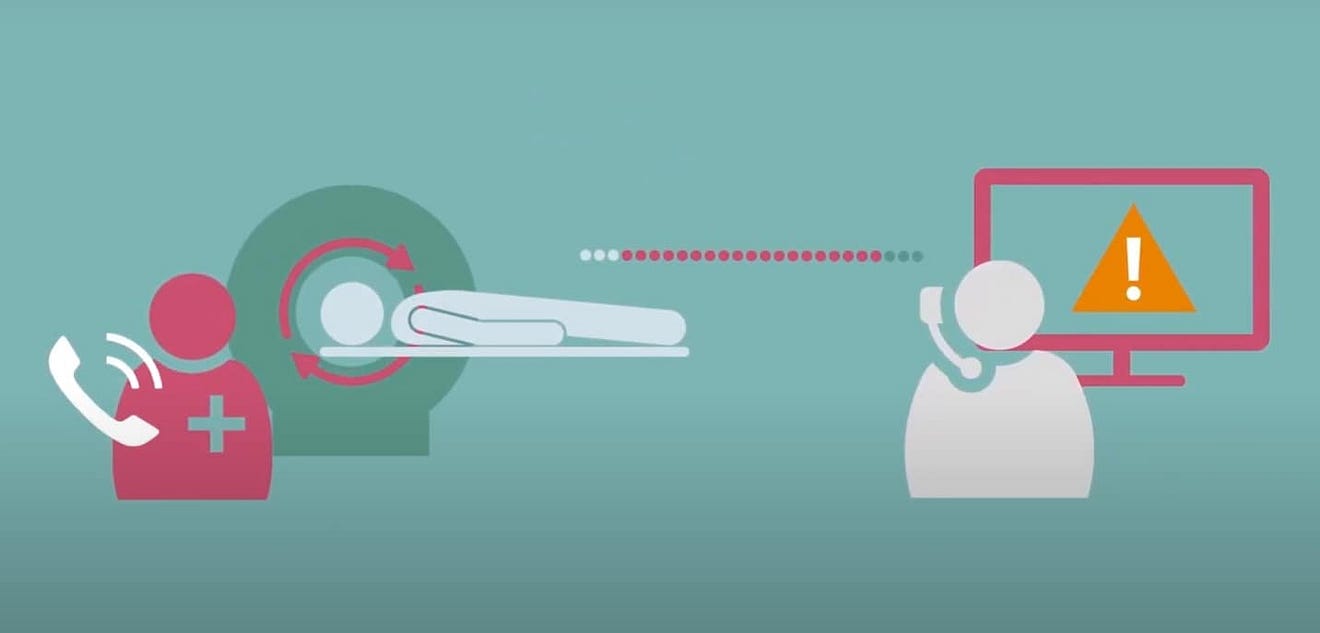
Remote connectivity allows for proactive monitoring and maintenance of medical equipment like MR scanners, which can help to prevent unnecessary downtime and patient delays
That’s just one way in which remote connectivity can add value to MR. On top of that, we started adding smartness to reduce the inherent complexity in MR — a second step forward in its digital evolution.
Adding smartness to make the complex simple
As any MR technologist or operator will tell you, performing an MR exam is not easy. Every patient has a different anatomy. There is a wide range of different protocols to choose from. And an MR exam is also time-consuming, taking anywhere from 15 to 60 minutes depending on the complexity of the case. For patients, spending such a long time in a restricted space can be stressful — especially because they need to hold still during the exam. Patient motion requires a redo in nearly one in five cases [1]. With ever-rising numbers of exams and a scarcity of qualified technologists in many parts of the world, that puts a huge pressure on staff — contributing to high levels of stress and burnout [2].
Can we make MR faster and easier for the operator, and more comfortable for the patient?
Thanks to AI and smart algorithms, we now can.
One of my favorite examples is a camera-based patient sensing technology that lets the MR technologist monitor a patient’s breathing without having to set up an old-fashioned respiratory belt. The technology can analyze over a hundred body locations in parallel to extract signs of breathing — allowing the setups of routine MR exams to occur in less than a minute, even for less experienced operators, while helping them keep a caring eye on the patient [3].
By offering automated workflow support we can further boost operator confidence, allowing them to focus more on patients and less on technology. And with the help of smart algorithms, we can also drastically accelerate image acquisition, shortening MR exams by up to 50% [4].
While these are fantastic first steps, it’s exciting to think how we could make MR systems even simpler to operate. For example, through wider use of camera-based sensing technology that supports with patient positioning. Or through image reconstruction algorithms that compensate for patient motion.
Imaging a patient’s anatomy may never become as straightforward as taking a family snapshot with your smartphone. But I’m convinced that advanced imaging like MR will keep getting more accessible and less time-consuming. The same goes for post-processing, segmentation, and interpretation of MR images, which can all benefit from smart applications that help technologists and radiologists make sense of ever-growing amounts of images.
Yet as helpful as these individual innovations are at different moments in the radiology workflow, we need to zoom out and look at the bigger picture as well.
Connecting the dots for patient-centered care
In today’s digital, networked, and increasingly virtual world, asking ourselves how we can make individual MR or other diagnostic systems smarter is not enough. We need to recognize that they are all part of a larger, interconnected “system of systems” — a distributed network in which patient data needs to flow across different systems, different locations, and different care professionals.
Just like our smartphones can now seamlessly connect to a smart thermostat or a smart car, the next step in healthcare’s digital transformation will be all about integration.
In the context of radiology, that means we need to look for ways to connect and optimize the entire workflow — all the way from patient scheduling to planning the scan, interpreting it, creating a report, and bringing multiple types of patient information together for clinical decision-making (as my colleague Kees Wesdorp has detailed here).
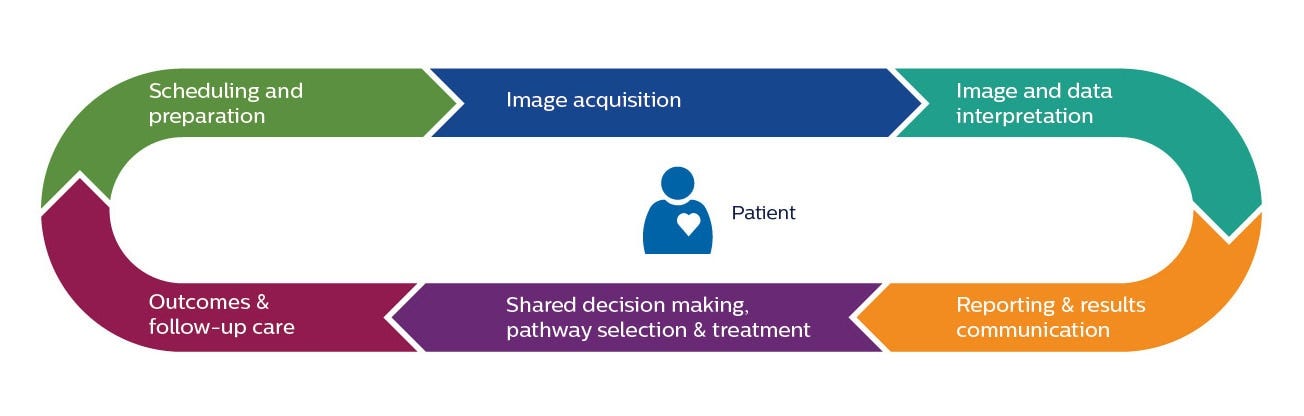
Integration also means bridging the physical and the virtual world to transcend traditional boundaries of care. For example, through a new concept called the Radiology Operations Command Center, we can now connect imaging experts in a central hub with technologists at scan locations across an imaging network, offering them virtual over-the-shoulder support while the patient is in the scanner. Not only does this help to standardize image quality irrespective of operator expertise, it can also make advanced imaging like MR accessible at more locations, closer to where patients live, at more flexible hours.
Combined with (AI-enabled) tele-radiology services for the expert interpretation of images, this could further take the complexity out of MR and make it more widely available. And that’s good news for patients who may lack access to specialized MR services today.
An ongoing journey of digital transformation
Although we have made huge steps forward, the digital evolution of MR — as a building block of wider, integrated solutions — remains very much an ongoing journey.
Especially in terms of connectivity, there is still much to gain. Over the last decade, healthcare has been cautious in moving to the cloud. But in the wake of COVID-19, adoption is gaining momentum. During the pandemic, healthcare providers have experienced firsthand how cloud-based services — backed by robust security standards — allow for rapid implementation of innovations across settings [5].
In the future, I imagine we will be able to update and upgrade MR and other diagnostic systems over the air, just like we are used to updating our smartphone overnight. This means we could make the newest features available much more quickly, and always have MR scanners run at peak performance to serve patients optimally.
During the pandemic, healthcare providers have experienced firsthand how cloud-based services — backed by robust security standards — allow for rapid implementation of innovations across settings.
I expect we will also see increased adoption of cloud-based app stores in healthcare, echoing the revolutionary impact of the smartphone’s app store model. For example, in radiology, this can take the form of curated software marketplaces that allow radiologists to download validated apps from a large number of third-party developers via a common platform — without having to worry about point-to-point integrations for each app individually (which would quickly turn into a nightmare for a hospital CIO). It will then be the role of healthcare solution providers like Philips to ensure that such apps run seamlessly on the consoles and mobile devices used by hospital staff — similar to how the best smartphone manufacturers offer one frictionless experience.
Business models will likely change as a result, with subscription-based software and services becoming more prevalent. And one thing we can be certain of: in this new emerging world of digital ecosystems, innovation will rely even more strongly on collaboration than it does today.

It is often said that we overestimate the impact of innovation in the short term while underestimating its impact in the long term. If you need any proof of that statement, just pause for a moment the next time you pick up your smartphone. Could you have foreseen, 15 years ago, all the benefits it would deliver to you today — as well as to billions of other people around the world?
Now imagine what healthcare could be like if it were just as smart and connected.
References
[1] https://www.healthimaging.com/topics/advanced-visualization/patient-motion-during-mri-proves-be-costly-conundrum
About the author

Henk van Houten
Executive Vice President, Chief Technology Officer, Royal Philips
Henk van Houten joined Philips Research in 1985, where he investigated quantum transport phenomena in semiconductor nanostructures — work awarded with the Royal Dutch Shell prize.
In 2016, he became Chief Technology Officer of Royal Philips.
In this role, he has global responsibility for Research, Innovation Services, the Philips HealthWorks, Philips Innovation Campus Bangalore, Group Technology Start Ups, Technology and R&D Management, and the Idea to Market Excellence Program. He is Vice Chair of the Group Innovation Board.
Originally published at https://www.philips.com












