A summary of data reported to the National Healthcare Safety Network
Infection Control & Hospital Epidemiology | Cambridge Core
Lindsey M. Weiner-Lastinger MPH1 , Vaishnavi Pattabiraman MSc, MS, MPH1,2 , Rebecca Y. Konnor MPH1,3 , Prachi R. Patel MPH1,3 , Emily Wong MPH1,2 , Sunny Y. Xu MPH1,3 , Brittany Smith MPH1,4 , Jonathan R. Edwards MStat1 and Margaret A. Dudeck MPH1
Cambridge University Press: 03 September 2021
ABSTRACT
Objectives:
To determine the impact of the coronavirus disease 2019 (COVID-19) pandemic on healthcare-associated infection (HAI) incidence in US hospitals, national- and state-level standardized infection ratios (SIRs) were calculated for each quarter in 2020 and compared to those from 2019.
Methods:
Central–line–associated bloodstream infections (CLABSIs), catheter-associated urinary tract infections (CAUTIs), ventilator-associated events (VAEs), select surgical site infections, and Clostridioides difficile and methicillin-resistant Staphylococcus aureus (MRSA) bacteremia laboratory-identified events reported to the National Healthcare Safety Network for 2019 and 2020 by acute-care hospitals were analyzed. SIRs were calculated for each HAI and quarter by dividing the number of reported infections by the number of predicted infections, calculated using 2015 national baseline data. Percentage changes between 2019 and 2020 SIRs were calculated. Supporting analyses, such as an assessment of device utilization in 2020 compared to 2019, were also performed.
Results:
Significant increases in the national SIRs for CLABSI, CAUTI, VAE, and MRSA bacteremia were observed in 2020.
Changes in the SIR varied by quarter and state.
The largest increase was observed for CLABSI, and significant increases in VAE incidence and ventilator utilization were seen across all 4 quarters of 2020.
Conclusions:
This report provides a national view of the increases in HAI incidence in 2020.
These data highlight the need to return to conventional infection prevention and control practices and build resiliency in these programs to withstand future pandemics.
Significant increases in the national SIRs for CLABSI, CAUTI, VAE, and MRSA bacteremia were observed in 2020.
Changes in the SIR varied by quarter and state.
The largest increase was observed for CLABSI, and significant increases in VAE incidence and ventilator utilization were seen across all 4 quarters of 2020.
These data highlight the need to return to conventional infection prevention and control practices and build resiliency in these programs to withstand future pandemics.

As the coronavirus disease 2019 (COVID-19) pandemic swept through the United States, regions experienced peak cases and hospitalizations at various times in 2020.Reference Sapiano, Dudeck and Soe1
The pandemic response placed burden on acute-care hospitals (ACHs), which may have altered staffing practices, increased critical care capacity, and modified use of personal protective equipment (PPE).Reference Rebmann, Alvino and Holdsworth2,Reference Weiner-Lastinger, Dudeck and Allen-Bridson3
In the early stages of the pandemic, little was known about how COVID-19 hospitalizations would affect the incidence of healthcare-associated infections (HAIs).
Single-site studies observed early signs of increases in select HAIs during the spring of 2020.Reference Fakih, Bufalino and Sturm4–Reference LeRose, Sandhu and Polistico6
Others have studied the occurrence of secondary infections in COVID-19 patients.Reference Kumar, Adams and Hererra7–Reference Smith, Karaba and Amoah9
Additionally, a report from the National Healthcare Safety Network (NHSN) found significant increases in central-line-associated bloodstream infections (CLABSIs) during the early months of the pandemic.Reference Patel, Weiner-Lastinger and Dudeck10
The NHSN is the nation’s largest HAI surveillance system and is used by nearly all US hospitals to fulfill local, state, or federal HAI reporting requirements.
NHSN data are used to measure progress toward prevention goals; this progress is assessed using an observed-to-predicted ratio called the standardized infection ratio (SIR).
Nationally, from 2015 to 2019, there have been consistent, significant reductions in the SIRs for CLABSIs, catheter-associated urinary tract infections (CAUTIs), and Clostridioides difficile infection (CDI) laboratory-identified (LabID) events.12–Reference Nkwata, Soe, Li, Godfrey-Johnson, Edwards and Dudeck14
Some significant year-to-year decreases have also been observed in methicillin-resistant Staphylococcus aureus (MRSA) bacteremia LabID events since 2010.
Conversely, there has been minimal change in the occurrence of ventilator-associated events (VAEs).
Given the potential for COVID-19 response activities to impact HAI prevention and surveillance, the NHSN team analyzed national and state SIRs to identify potential changes in HAI incidence between 2019 and 2020.
Methods
See the original publication
Results
See the original publication

Discussion
This report is the first to present national and select state-level quarterly SIRs for each HAI type in 2020, along with a comparison to 2019 SIRs.
Due to reporting requirements for the CMS HACRP, NHSN data are representative of largely all ACHs in the country and provide a national picture of how patient safety, in particular HAI incidence, may have been affected by the COVID-19 pandemic.
Prior to the pandemic, widespread decrease in HAI incidence had been observed across US hospitals.
Except for VAE, the national 2020-Q1 SIR for each HAI was below 1 and significantly lower than that from 2019-Q1, indicating a continual decline in HAI incidence at the beginning of 2020.
As hospitals began to respond to the COVID-19 pandemic in 2020-Q2, increases in national SIRs became apparent.
Initial increases in the SIRs were observed early in the year for CLABSI and MRSA bacteremia (starting in 2020-Q2) and for VAE (starting in 2020-Q1).
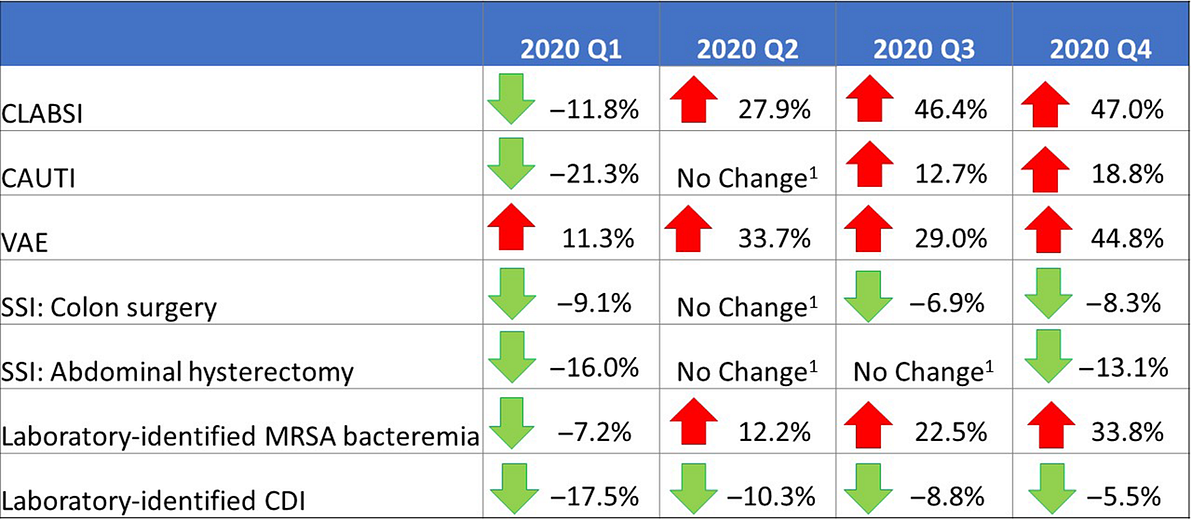
However, compared to 2019, 2020-Q3 and 2020-Q4 saw large and significant increases in the CLABSI, CAUTI, VAE, and MRSA bacteremia SIRs (Fig. 1).
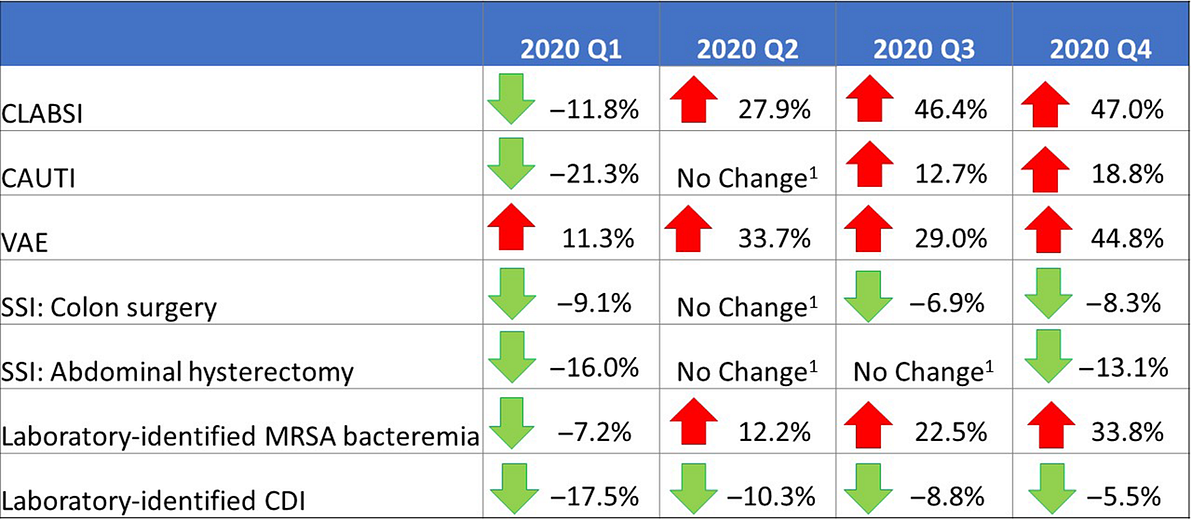
Fig. 1.Changes in the 2020 national healthcare-associated infection (HAI) standardized infection ratios (SIRs) for acute-care hospitals, compared to respective 2019 quarters.
The CLABSI SIR experienced the greatest increase among all HAI types; the heightened CLABSI incidence during the pandemic and the likely impacts of hospital COVID-19 prevention activities on central-line insertion and maintenance practices have been previously documented. Reference Fakih, Bufalino and Sturm4–Reference LeRose, Sandhu and Polistico6,Reference Patel, Weiner-Lastinger and Dudeck10CAUTIs and VAEs were also reported more frequently in 2020 than 2019.
A longer patient length-of-stay, additional comorbidities and higher patient acuity levels, and a longer duration of device use in 2020 could have contributed to an overall increased risk of a device-associated infection during the pandemic.
In addition, some studies identified an increased risk of ventilator-associated conditions in critically ill COVID-19 patients. Reference McMullen, Smith and Rebmann5,Reference Maes, Higginson and Pereira-Dias 20
The characteristic worsening of respiratory status in some patients with COVID-19 resulted in an increase in the number of hospitalized patients in 2020 that required ventilation, and an increase in patients’ average duration of ventilation, both of which could have contributed to an increased risk of VAE.
Almost all states previously identified by CDC with a high COVID-19 hospital admission burden observed increases in their 2020-Q2 CLABSI and VAE SIRs compared to 2019, most of which were statistically significant.Reference Sapiano, Dudeck and Soe1
Preliminary data for 2020-Q4 showed a large increase of 34% in the national MRSA bacteremia SIR compared to 2019-Q4.
There were 2,715 MRSA bacteremia events reported for 2020-Q4, which is 41% higher than the number of events reported by the same set of hospitals in 2019-Q4.
Further investigation is needed to identify the source of these additional events.
A previous study found that device-associated infections, particularly those related to central-lines, are a common source of MRSA bacteremia; thus, the increase in MRSA bacteremia in 2020 is possibly a result of inadequate central-line insertion and maintenance practices.Reference Fakih, Bufalino and Sturm4,Reference LeRose, Sandhu and Polistico6,Reference Ham, See and Novosad21
However, preliminary NHSN data show no substantial changes in 2020, compared to 2019, in the proportion of CLABSIs caused by S. aureus, or in the proportion of S. aureus CLABSIs that are resistant to methicillin (data not shown).
S. aureus has been identified as a common cause of secondary bacterial infection in COVID-19 patients.Reference Kumar, Adams and Hererra7,Reference Smith, Karaba and Amoah9
One meta-study found that >25% of all coinfections in COVID-19 patients were related to S. aureus, more than half of which were MRSA.Reference Adeiza, Shuaibu and Shuaibu22
Whether some of the MRSA bacteremia events reported to NHSN in 2020 occurred as secondary infections in patients with COVID-19 remains unknown.
The increased focus on hand hygiene, environmental cleaning, patient isolation, and use of PPE during 2020, combined with continued inpatient antimicrobial stewardship programs and a marked decline in outpatient antibiotic prescribing, may have resulted in decreases in the CDI SIRs during 2020 compared to 2019.Reference McMullen, Smith and Rebmann5,23
The increased focus on hand hygiene, environmental cleaning, patient isolation, and use of PPE during 2020, combined with continued inpatient antimicrobial stewardship programs and a marked decline in outpatient antibiotic prescribing, may have resulted in decreases in the CDI SIRs during 2020 compared to 2019.
This analysis has several limitations.
The 2020-Q4 data were analyzed prior to the CMS HACRP reporting deadline of May 17, 2021, and therefore may be incomplete. This analysis was restricted to hospitals that reported data for both 2019 and 2020; new hospitals and units that opened in 2020 were not included. Thus, this paper does not reflect all HAIs that occurred in the United States. Information on the voluntarily reported COVID-19 status of patients with HAIs was not explored. In addition, we focused solely on ACHs for this analysis, and did not address HAI incidence in other settings that may have cared for COVID-19 patients, such as critical access and long-term ACHs.
This is the first comprehensive look at the impact of COVID-19 on HAI incidence at the national and state levels.
Substantial increases in CLABSIs, CAUTIs, VAEs, and MRSA bacteremia were observed.
The year 2020 marked an unprecedented time for hospitals, many of which were faced with extraordinary circumstances of increased patient caseload, staffing challenges, and other operational changes that limited the implementation and effectiveness of standard infection prevention practices.
A regular review of HAI surveillance data is critical for hospitals to identify gaps in prevention and address any observed increases in HAIs.
Infection prevention staff should continue to reinforce infection prevention practices in their facilities, and consider the importance of building resiliency in their programs to withstand future public health emergencies.
Originally published at https://www.cambridge.org.
About the authors & affiliations
Lindsey M. Weiner-Lastinger MPH1 , Vaishnavi Pattabiraman MSc, MS, MPH1,2 , Rebecca Y. Konnor MPH1,3 , Prachi R. Patel MPH1,3 , Emily Wong MPH1,2 , Sunny Y. Xu MPH1,3 , Brittany Smith MPH1,4 , Jonathan R. Edwards MStat1 and Margaret A. Dudeck MPH1
1 Division of Healthcare Quality Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia,
2 Leidos, Atlanta, Georgia,
3 CACI, Atlanta, Georgia and
4 Oak Ridge Institute of Science and Education, Oak Ridge, Tennessee












