This is an excerpt of the publication above, focusing on the overview of the project.
IDB and Healthcare Israel
Amir Gilboa and Luis Tejerina
2022
Edited by
Joaquim Cardoso MSc.
Institute for Health Transformation
Research Institute for “Better Health and Care for All, at a lower cost”
June 15, 2022
Structure of the publication
- Preface
- Executive Summary
- Background
- Introduction
- The Need for the HIE, and the Challenges it Addresses
- The Israeli National HIE Solution
- The Israeli National HIE Implementation
- Evaluation of Results
- Reflections and Recommendations

5. THE ISRAELI NATIONAL HIE IMPLEMENTATION
5.1. Implementation Methodology
The implementation of the Israeli HIE involved health organizations right from the beginning.
This increased organizational buy-in, helped overcome objections, and made each organization an important part of the process rather than a recipient of government mandates.
The MOH’s first implementation step of the national platform was a kickoff meeting with executive managers in each health organization before the implementation got underway.
In this meeting, the MOH’s team presented the project, its vision and purpose, and the responsibility of each partner (MOH, health organization, software provider).
The MOH started the implementation with the early-adopter organizations while encouraging others to join them.
After the kickoff, while the implementation process was getting underway, the health organizations were responsible for the following functions:
· Agreement — Signing an agreement to formalize the organization’s participation containing the commitments made by all parties to the implementation process
· Infrastructure — Supporting the technical team with the installation of local servers and paving a line of communications to the MOH datacenter
· Development — Developing an interface between the local EMR and the local HIE (together with the local EMR provider)
Throughout the process, the MOH team worked closely with each organization’s team to define timelines and provide help with any questions or challenges in the implementation process.
5.2. Key Takeaways of the HIE Implementations
A key takeaway from Israel’s Ofek and Eitan implementations is the need for transparency and sharing of all information on the hospital’s implementation planning during the implementation process.
When all stakeholders felt they were part of the decision-making team, and that they played important roles with real influence, the implementation process moved forward smoothly.
Another takeaway is the importance of listening to employees to understand their needs.
Doing so helped the employees adapt to the new system and quickly resolve their concerns. For instance, when Ofek was first implemented in most health organizations, the physicians saw it as a critical system like EMRs, even though the MOH’s original plan did not classify it as such.
The organizations and the ministry had to reconsider their classification upon receiving the many complaints filed by the physicians on the essentiality of the HIE for their daily routines, especially in emergency situations.
A third takeaway, from the Eitan implementation, is the importance of a friendly user interface (see figures 5, 6, and 7).
The Eitan system is more complex than its predecessor and adds important functionality, which also increases the need to simplify and improve the user interface.
5.3. Incentives
The implementation of a new core system can be a challenge for any organization, but especially for health organizations, which are usually very conservative.
The Ofek implementation was remarkably smooth because the organizations clearly understood how its benefits met their needs, so they were eager to move forward with implementation.
The Eitan implementation was more complex. Health organizations had to upgrade their infrastructures (servers, interfaces, and more), so several organizations delayed implementing the new version — partly because Ofek was already better than anything that had preceded it and partly because of the costs (time and financial) of upgrading or changing the infrastructure. (The implementation timeline is shown in Figure 2, and the process is detailed in section 4.1.)
To address the financial issue, the MOH decided to provide a grant to health organizations to cover the cost of infrastructure upgrades and connection to the new HIE.
Grants were given based on the speed of the Eitan implementation: 100 percent funding for organizations that implemented in the first three months after kickoff, 75 percent for organizations that implemented in four to six months, 50 percent for implementation in seven to nine months, 25 percent for implementation in 10 to 12 months, and 0 percent for organizations that delayed implementation past one year.[1]
To address the financial issue, the MOH decided to provide a grant to health organizations to cover the cost of infrastructure upgrades and connection to the new HIE.
This incentive model succeeded in motivating several organizations to focus their efforts, build their infrastructures, and implement in a timely manner.
Approximately 25 percent of organizations received the full grant amount.
Some organizations have not yet chosen to join the new system, so work continues to help more organizations enjoy the added benefits of the upgraded HIE network.

6. EVALUATION OF RESULTS
To measure and evaluate the results and value of the Ofek HIE, the MOH studied the results between an experimental group of users and a control group.
The study shows that the implementation improved clinical as well as administrative results by reducing unnecessary tests and hospitalizations.
In the first case it is important to balance the clinical need vs the patient safety and patient satisfaction.
While it is necessary to take a blood tests and imaging for a better diagnostic and care, if there are tests and imaging data already available to the physicians, patients do not have to suffer from unnecessary tests or unnecessary exposure to radioactivity.
Also, unnecessary hospitalizations can expose patients to infections and decrease their satisfaction.
Administrative effects can be measured as cost savings since unnecessary tests or hospitalization days generate unnecessary costs for the payers and the insurers.
The main results of the study are shown in Table 3 (Nirel et al., 2010)[2].
TABLE 3: Results of the experimental study of Ofek
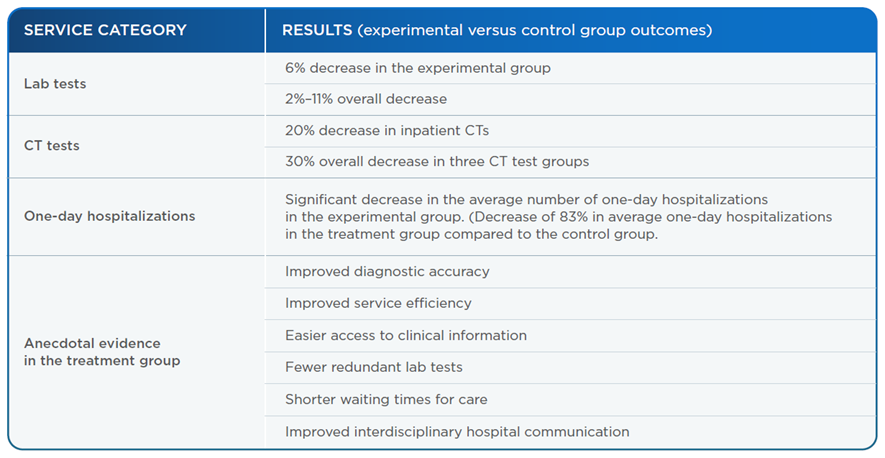
Source: Nirel et al., 2010[3].

7. REFLECTIONS AND RECOMMENDATIONS
7.1. Recommendations
· Stakeholder management — Each country and region may have different stakeholders, preconditions, and policy considerations that must be considered when implementing a digital health solution like an HIE. A key lesson from Israel’s HIE implementation is that the first step should be to understand the healthcare ecosystem, especially in three main areas:
o Health system structure (including the regulation, policy, and billing models)
o Existing IT systems in health organizations (including EMRs, terminologies, and interoperability options)
o Security and privacy requirements and regulations
After key information is gathered and the next steps can be planned, it is important to involve stakeholder representatives to increase buy-in, which facilitates the implementation, and provide feedback on ways to improve the system.
· Main components of the HIE solution — Another key finding from the Israeli case is that the planning process must consider all the aspects of the HIE solution and be able to divide it into three main components: terminology solutions, regulation and instructions adjustments, and technology and integration solutions.
· Architecture — The solution architecture has to serve all or most of the stakeholders’ interests. As became clear in Israel, the architecture is what persuaded health organizations to join the national HIE. The decision to avoid a central database, for instance, helped the organizations feel more confident that their data would stay on-site and not be copied or amended by others.
· Security and privacy — It is very important to combine the security and privacy components at the design stage of the new HIE. The security and privacy design has to support and secure the data but not disturb the functionality or effectiveness of the solution. For instance, as seen in Israel, the decision to use an opt-out model, even though it is sometimes better to use an opt-in model for privacy protection, made the platform very effective from day one.
· Terminology — Terminology issues can be a significant barrier to implementing an HIE. The more EMR systems are in use, the more terminology becomes a major issue. Using a terminology mapping and conversion mechanism from the beginning of the HIE project can help more organizations join HIE initiatives and help simplify and smote the implementation.
· Implementation partners — Choosing the right implementation partners can be critical to the success of implementing a national HIE. Once the plan for a national HIE is in place — and stakeholders have been involved from the beginning — the next recommended step is to identify and choose implementation partners who will be the early adopters, meaning those who will begin their implementation quickly and be able to showcase the system’s benefits.
· Incentives for health organizations — To ensure that health organizations’ successes and commitments are sustainable, it is recommended that health organizations taking part in the implementation sign an agreement committing the organization to the implementation process. To further aid organizations and ease the implementation, we recommend using incentive models to attract early adopters and maintain interest throughout the implementation.
In summary, the end goal of the implementation process is to create a win-win-win situation — for frontline healthcare providers, healthcare systems and organizations, and — especially — patients.
This is happening today in Israel, as demonstrated by the Israeli HIE case that shows it is possible to implement a national HIE solution while improving services and achieving the support of medical teams.
7.2. The Future of the HIE in Israel
The HIE implementation in Israel enables the MOH to use this infrastructure and continue developing more advanced services.
When Israel started to plan the national HIE program, it had a road map of the advanced services and capabilities that used the HIE as a national platform.
The following are some of the features that were planned. Currently, the MOH is considering the right way to implement these features or adjust them:
· HIE everywhere — To provide a mobile version of the EMR agent that allows medical staff to access medical information anytime, anywhere
· Care communication platform — To allow direct communication between caregivers from different hospitals or community doctors and the hospital, which is vital to continuity of care
· Personal health records at the palm of your hand — To allow patients to access their complete medical data anytime, anywhere using the HMO’s portal, the HMO’s mobile application, or a dedicated flash drive
· Decision support system interoperability at the point of care — To allow seamless integration and full interoperability of third-party decision support systems at the point of care
· IoT repository — To handle information generated by medical devices and the IoT
· IoT visualization and analytics — To allow visualization and analytics of continuous data from medical devices at the point of care.

References
See the original publication
About the authors
Written by: Amir Gilboa.
Technical edition: Luis Tejerina.
The author wishes to thank the following people for their contributions and remarks:
• Hagai Dror — Managing Director, Healthcare Israel
• Dr. Izhak Zaidise — Chief Medical Officer, Healthcare Israel
• Mrs. Mali Shapira — HIE Division Manager, IT Department, Israeli MOH
• Tziel Ohayon — Sr. Sales Engineer, PH Solutions Architects, DB Motion — All Scripts
Originally published at https://publications.iadb.org