Led by Duke University and Covid Collaborative
March 2022
Executive Summary
At this pivotal moment, the world’s response to the pandemic must shift from emergency crisis management to a sustainable control strategy.
This strategy should help to build resilient health systems with capabilities to address potential future COVID-19 outbreaks and other public health threats.
Driving the urgent need for an updated strategy are
- important recent developments related to the SARSCoV-2 virus,
- the impact of current vaccines, and
- the world’s response to the pandemic.
The Omicron variant’s high transmissibility and partial immune evasion have changed both the purpose and definition of vaccination.
- The primary purpose of vaccination with current vaccines is now to prevent severe disease, hospitalization, and death, not to prevent transmission or infection.
- There is also growing recognition that full vaccination for many current vaccines requires three doses, plus additional boosters over time.
- Moreover, there is increasing evidence that duration of protection from current vaccines and from infection is limited.
As a result, achieving the WHO goal of 70 percent population coverage with primary vaccination by mid2022 seems no longer the best path to save the most lives with limited resources in most countries.
Rather, countries should prioritize full vaccination and boosters for those at highest risk to minimize severe disease, hospitalization, and deaths — and thus protect health systems so they can meet other critical population health needs as well.
As a result, achieving the WHO goal of 70 percent population coverage with primary vaccination by mid2022 seems no longer the best path to save the most lives with limited resources in most countries.
Rather, countries should prioritize full vaccination and boosters for those at highest risk to minimize severe disease, hospitalization, and deaths — and thus protect health systems so they can meet other critical population health needs as well.
Promisingly, the ability to manage and contain COVID-19 outbreaks is improving.
- Vaccine supply is rising.
- Increased supply and development of effective countermeasures are expanding our arsenal.
- Low-cost rapid diagnostic tests and highly effective oral antiviral therapies can prevent surges in cases from turning into high rates of severe illness and deaths.
- Tests and therapies are playing an increasing role in containing COVID-19 in some high income countries, and much work remains to ensure equitable access to these in most low- and middle income countries.
- Improved access to oxygen and PPE can also help limit the impact of future case surges.
At the same time, two years into the pandemic, attention to other population health priorities can no longer be deferred.
- Many countries have lost substantial ground in providing routine immunizations, preventive services, and chronic disease management.
- Improvements in local manufacturing and distribution of vaccines and drugs, and in primary and community-based care, can help control COVID-19 and strengthen preparedness for the next variant or pandemic.
With thoughtful planning, these steps could also help countries address their other population health priorities.
Unfortunately, the actions of high-income countries and multilateral organizations to address global COVID-19 needs has been far from sufficient to achieve an equitable emergency response.
Now, transitioning to the next phase, the challenges to global equity in COVID-19 containment could worsen.
Unfortunately, the actions of high-income countries and multilateral organizations to address global COVID-19 needs has been far from sufficient to achieve an equitable emergency response.
Now, transitioning to the next phase, the challenges to global equity in COVID-19 containment could worsen.
High-income countries are eager to return to more normal activities, undermining current emergency response efforts.
The worsening military and humanitarian crisis in Ukraine is consuming growing attention and resources, especially in Europe and North America, and threating food security in many countries, further straining the COVID-19 response.
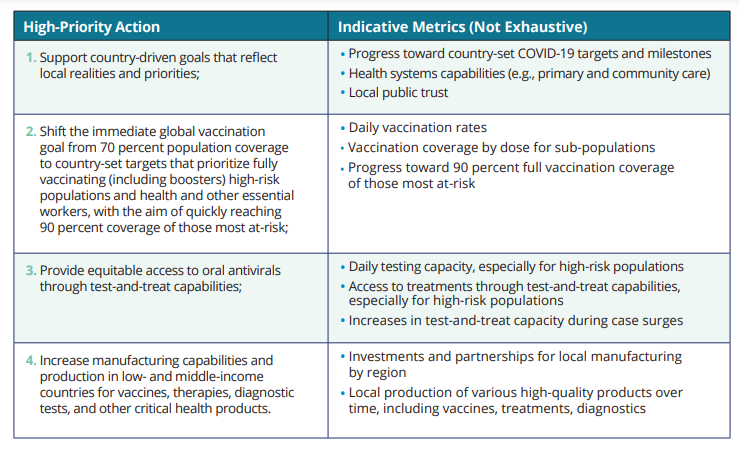
In response to these factors, national leaders, donors, multilateral organizations, and global public health organizations must support the urgently needed shift in global strategy by implementing the following four actions:
- Support country-driven goals that reflect local realities and priorities;
- Shift the immediate global vaccination goal from 70 percent population coverage to country-set targets that prioritize fully vaccinating (including boosters) high-risk populations and health and other essential workers, with the aim of quickly reaching 90 percent coverage of those most at-risk;
- Provide equitable access to oral antivirals through test-and-treat capabilities; and
- Increase manufacturing capabilities and production in low- and middle-income countries for vaccines, therapies, diagnostic tests, and other critical health products.
Timely reporting of high-quality data at national and sub-national levels is necessary to assess progress and strengthen accountability.
Robust financing and improved governance are also critical to achieve these recommendations.
G20 nations, multilateral development banks, and private donors should increase non-debt financing for COVID-19 control and future preparedness and link this financing directly to local health systems capabilities and resilience.
Multilateral governance must be reformed to enable more inclusive decision-making and more effective use of resources, including the ability to redirect and reallocate funding across initiatives and organizations.
The US-hosted Global COVID-19 Leaders Summit, likely to be held in April, holds the potential to be the most consequential event since the pandemic began by redirecting the global response onto a more sustainable, effective, and equitable trajectory.
The US-hosted Global COVID-19 Leaders Summit, likely to be held in April, holds the potential to be the most consequential event since the pandemic began by redirecting the global response onto a more sustainable, effective, and equitable trajectory.
Appendix: Data and Accountability (excerpted from the report)
Data and Accountability National leaders should commit to the collection and public reporting of timely, high-quality data at national and sub-national levels across the four actions noted above, in order to analyze evolving needs and gaps, provide the right resources and support to address them, assess overall progress toward country-set targets, and strengthen accountability.
Key measures of access and outcomes for different subgroups, such as by age, gender, geography, and important risk factors, will strengthen efforts to design and implement equitable programs to increase access to immunization, test-and-treat, oxygen, and other tools for pandemic response. Dynamic “country dashboards” that track progress toward country-led targets and milestones would provide valuable information to guide national, regional, and global policy-making and resource-allocation decisions as well as accountability for timely progress.
These efforts should also enable the identification and sharing of best practices to address various challenges, enabling a robust peer learning network among public and private sector organizations that improves the effectiveness and efficiency of response and preparedness.
The following table includes indicative metrics that could be tracked in order to assess progress towards each of the four priority actions noted above. COVID GAP will continue to capture and analyze data on important aspects of pandemic response, preparedness, and health systems resilience over the coming months, and will regularly publish Accountability Reports providing key insights and recommendations to strengthen actions and outcomes at all levels.
About the authors
Krishna Udayakumar is director of the
Duke Global Health Innovation Center.
Gary Edson is president of the
COVID Collaborative and former US deputy national security advisor and
deputy national economic advisor.
Michael Merson is a
Duke University professor and
former director of the World Health Organization Global Program on AIDS.
Mark McClellan directs the
Duke-Margolis Center for Health Policy, and is a former US FDA commissioner
and CMS administrator.
About Covid Gap
The COVID Global Accountability Platform (COVID GAP), led by Duke University and COVID Collaborative, aims to improve and accelerate global pandemic response by serving as an independent source of insights and actionable recommendations, convening key stakeholders to galvanize actions and collaborations, and strengthening transparency and accountability. Find out more: https://covid19gap.org/.
Disclosures
This report and related COVID Global Accountability Platform (COVID GAP) activities are supported by funding from the Bill & Melinda Gates Foundation and The Rockefeller Foundation.
The content and recommendations in this report is an independent effort by COVID GAP, without approval by any external parties. It does not necessarily reflect the viewpoints of funders or any person who contributed to discussions with the COVID GAP team that helped inform this report.
Originally published at https://www.rockefellerfoundation.orghttps://joaquimcardoso.blog/media/0f5edd046e803efd771d3067c57282b9