the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
September 25, 2023
One page summary
What is the message?
The United Nations’ high-level meeting (HLM) on universal health coverage (UHC) recently adopted a political declaration, committing member states to provide health services for all.
However, this commitment remains an empty promise unless governments invest substantially in primary healthcare.
As of 2021, over half of the world’s population lacked full access to essential health services, with approximately one billion people spending more than 10% of their income on healthcare.
Key Takeaways:
1. The Challenge of Implementation
Dr. Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization (WHO), emphasized that UHC is not just a paper declaration but a political choice that requires real investments. He urged member states to prioritize UHC in their policies and allocate resources to primary healthcare, including supporting healthcare workers.
2. Stalled Progress
Despite a similar declaration in 2019 aimed at ensuring universal access to healthcare, progress towards UHC has faltered, mainly due to the COVID-19 pandemic. As of 2021, over half of the world’s population lacked full access to essential health services, with approximately one billion people spending more than 10% of their income on healthcare.
3. Barriers to Access
Factors such as geography, income, education, gender, and age continue to limit access to basic healthcare for many individuals. Additionally, non-communicable diseases pose a growing threat. Activists also highlighted religious and cultural biases that hinder access to healthcare, with some countries even criminalizing LGBTQ individuals.
4. Calls for Inclusivity
The United States and Norway explicitly called for UHC to include marginalized populations, emphasizing the importance of sexual and reproductive health rights. EU Commissioner Ylva Johansson stressed the need to address health determinants, inequalities, and gender disparities for equitable and sustainable health systems.
5. Financing for UHC
Tunisia’s foreign affairs minister, Nabil Ammar, representing the African group, called for sufficient, predictable, and sustainable financing to support UHC efforts in developing countries. Japan and the European Union (EU) have heavily invested in UHC, with Japan pledging over $7.5 billion, and the EU allocating over €4.4 billion between 2021 and 2027 for health system strengthening.
6. Embracing Technology
To bolster primary healthcare and address health crises, EU Commissioner Johansson emphasized digitalization and technology transfers while respecting international intellectual property rules.
In summary:
While the UN’s recent commitment to universal health coverage is a positive step, it will only become a reality if member states act decisively to invest in primary healthcare, remove barriers to access, and ensure inclusivity for all, especially marginalized populations. Adequate financing and the adoption of technology are key components of this effort.
DEEP DIVE
UN Universal Health Coverage Declaration: Paper Promise or Funded Reality?
Health Policy Watch
Kerry Cullinan
September 21, 2023

NEW YORK – While the United Nations (UN) high-level meeting (HLM) on universal health coverage (UHC) adopted a political declaration on Thursday committing member states to accelerate health for all, this will remain a paper promise unless governments invest in primary healthcare.
This was the challenge issued to member states by World Health Organization (WHO) Director-General Dr Tedros Adhanom Ghebreyesus at the start of the HLM.
“Ultimately, UHC is a political choice. The political declaration you have approved today is a strong signal that you are making that choice, but the choice is not just made on paper,” said Tedros.
“Most of all, it’s made by investing in primary health care, which is the most inclusive, equitable, cost-effective and efficient path to universal health coverage. In particular, investing in primary health care means investing in the people who deliver it: the healthcare workers who are the backbone of every health system.”
Tedros then made three requests of member states: make UHC “the central policy priority for your government”; increase domestic investments in primary health care, health workers and financial protection starting with the most vulnerable; and address the drivers of poor health in “the food people eat, the air they breathe and the conditions in which they live and work”.

Going backwards?
In 2019, the UN adopted a similar political declaration on UHC aimed at ensuring all people have access to health services when and where they need it, irrespective of their financial position.
But progress towards UHC has stalled since then, primarily due to the COVID-19 pandemic. By 2021 over half the world’s population – at least 4.5 billion people – were not fully covered by essential health services. About a billion spent over 10% of their income on health expenses.
Rebecca Akufo-Addo, Ghana’s First Lady and a UHC champion, told the HLM that “geography, income, education, gender and age continue to exclude many from basic health services” while “a further threat is the rise of non-communicable diseases.”
“We cannot continue to push people into poverty because of illness. We must develop insurance schemes that cover our people,” urged Akufo-Addo.
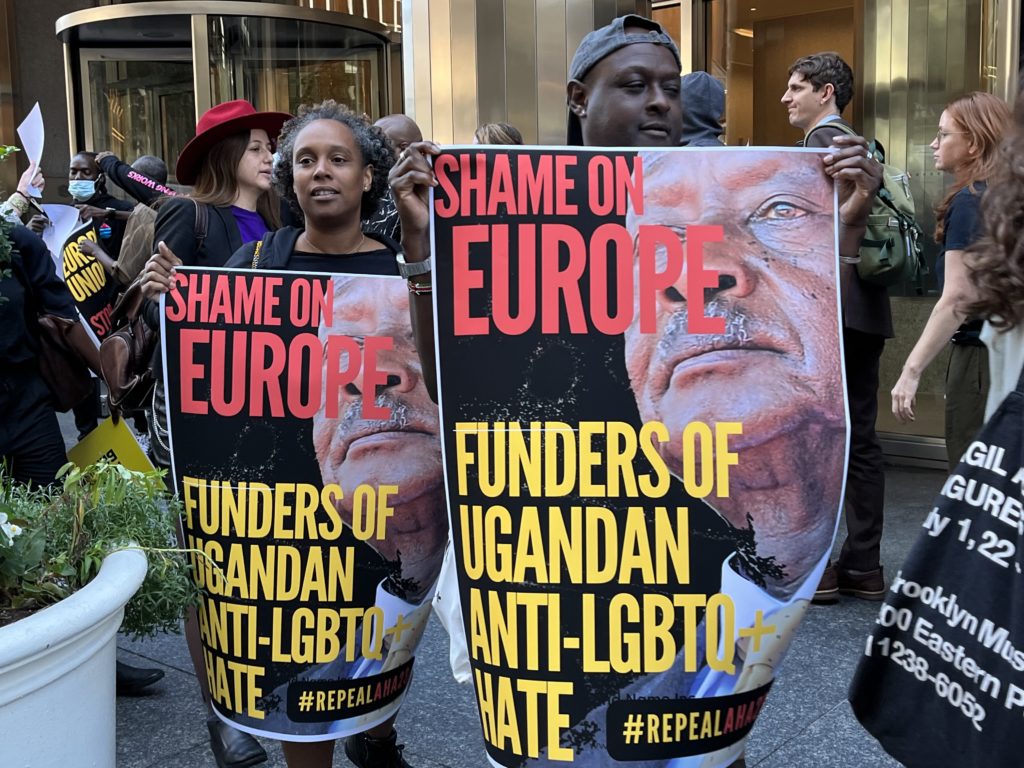
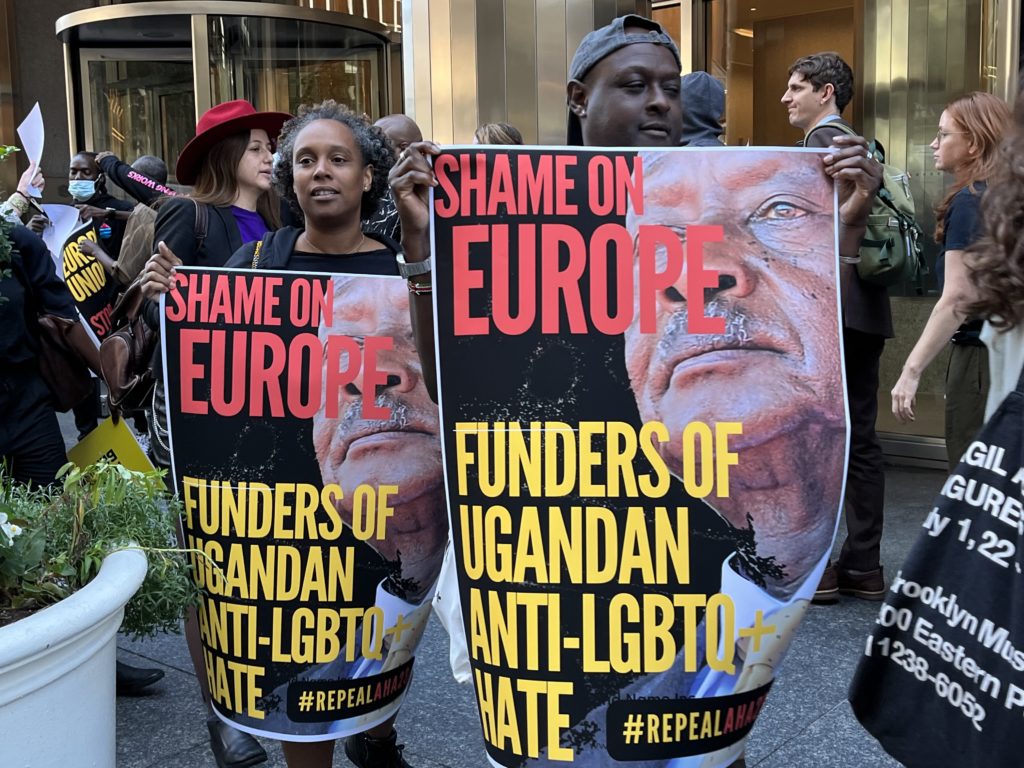
Expanding access to healthcare is also constrained by religious and cultural bias. The EU has not halted aid to Uganda despite that country passing an Anti-Homosexuality Act in May that criminalises LGBTQ people, even compelling health workers to report “suspected” LGBTQ people to the police. Kenya, Tanzania and Ghana are considering similar legislation.
Shortly before the HLM began, activists held a protest outside the EU Mission in New York to protest its ongoing aid to Uganda, holding posters calling for UHC to apply to everyone.
Addressing the HLM, the US and Norway explicitly called for UHC to be inclusive of all marginalised people.
“We must take bold action to include historically marginalised populations and ensure sexual and reproductive health and rights for all,” said Xavier Becerra, US Secretary of Health and Human Services.
“We must include the voices of women, the underrepresented, and LGBTQIA+ populations in our decision-making, and we must meaningfully include all people in all their diversity and reject policies that hinder their access to care because of bias, discrimination, or stigma.”
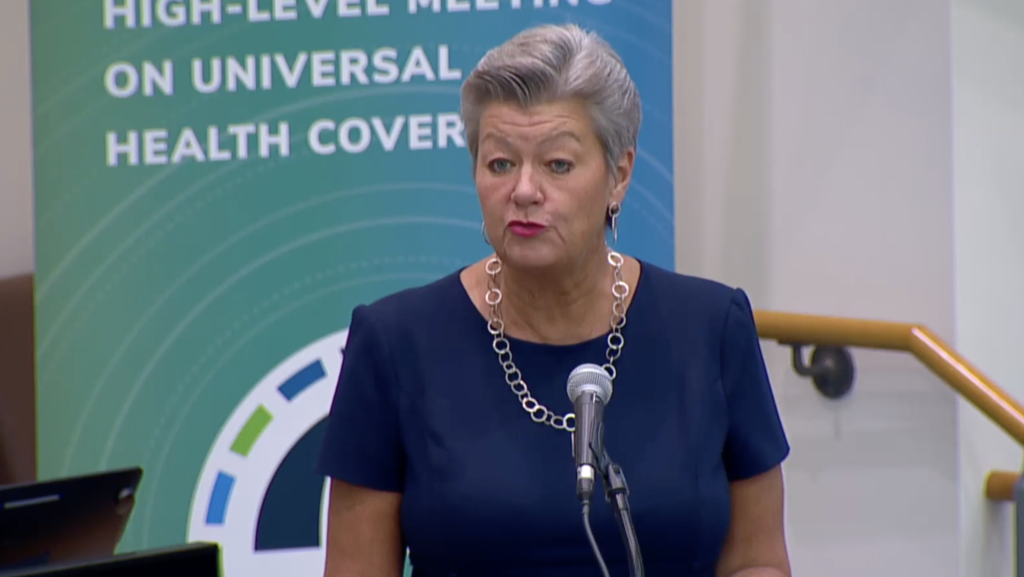
EU Commissioner Ylva Johansson said that governments “need to address the determinants of health as well as inequality and gender equality, including sexual and reproductive health, as a prerequisite for equitable, sustainable health systems and UHC”.
Sexual and reproductive health services are dismal in many parts of the world. At an event earlier in the week, philanthropist Melinda French Gates said that almost half of women in sub-Saharan Africa who wanted contraception could not get it. Meanwhile, access to abortion – even when a woman’s health is in danger – is getting far more difficult in many parts of the world, including the US.
Africa’s ask, EU and Japan’s response
Tunisia’s foreign minister, Nabil Ammar, speaking for the Africa group, called for “sufficient, predictable and sustainable financing to support national efforts by developing countries [to achieve UHC] through bilateral and multilateral financing, including innovative financing mechanisms and concessional financing”.
He also called for international financing to support the local and regional manufacturing of medical countermeasures to ensure Africans are protected during health emergencies and pandemics.”
Both Japan and the European Union have invested heavily in UHC. Japanese Prime Minister Fumio Kishida said that his country had made contributions totalling more than $7.5 billion dollars to assist with this.
He also said that G7 leaders had also endorsed the Impact Investment Initiative for global health to pursue expansion of private investment in UHC.
EU Commissioner Johansson said that between 2021 and 2027, EU institutions alone will contribute over €4.4 billion to health system strengthening in countries that most need UHC.
She emphasized strengthening primary health care “as the first line to protect people’s health and defend against infectious disease outbreaks”.
“We must foster digitalization as a fundamental enabler and exploit the potential of voluntary technology transfers based on mutually agreed terms fully in line with international intellectual property rules,” she said.
Originally published at https://healthpolicy-watch.news.












