BCG – Boston Consulting Group
By Ben Horner, Wouter van Leeuwen, Maggie Larkin, Julia Baker, and Stefan Larsson
SEPTEMBER 03, 2019
This is an excerpt from the report “Paying for Value in Health Care” published in September 2019, based on the introduction of the report. (VBHC: Value Based Health Care), edited by Joaquim Cardoso.
Introduction
As health systems around the world strive to improve health care value, one of the biggest obstacles they face is the way that individual clinicians and provider organizations are paid for the care they deliver.
Value in health care is generated by delivering better health outcomes for the same, or a lower, cost.
Yet, providers have typically been paid for the activities they perform-irrespective of whether those activities deliver value to patients.
In many countries, most physicians are still paid according to the traditional fee-for-service model.
And even where clinicians are salaried, their employers are reimbursed for the tests and procedures that their salaried clinicians collectively perform, regardless of the outcomes those activities produce.
The problem is not only that activity-based payment models lack incentives for improving health care value but also that they create powerful disincentives for doing so.
To cite one dramatic example, an analysis of more than 34,000 in-patient surgical procedures at a major US hospital system found that privately insured surgical patients with one or more complications provided the hospitals with a profit margin that was 330% higher — an additional $39,000 per patient, on average — than the margin from similarly insured patients who had no complications.[1]
In other words, the reimbursement system made it economically irrational to improve health care value by minimizing complications.
New value based payment models
To address these disincentives, health systems around the world are experimenting with new value-based payment models.
- They are paying performance bonuses to reward providers for meeting predefined thresholds for quality care.
- They are designing bundled payments that reimburse providers for all the activities associated with discrete episodes of care (for example, joint replacement), both to encourage more innovative and cost-effective treatments for the full cycle of care and to hold providers accountable for the ultimate health outcomes delivered to patients.
- And in some cases, they are paying lump sums that cover all of the expected costs to serve certain patient populations, creating incentives for providers to invest in prevention, early diagnosis, and proactive treatment in order to minimize total costs to the system.
The amount of experimentation and innovation in designing new value-based payment models is impressive. To give just one example, in a recent survey of US health care executives and clinical leaders, respondents reported that,
- on average, value-based payments constitute about a quarter of their organization’s revenues, and
- 42% said they believe that value-based payment will eventually become the primary revenue model in US health care. [2]
But it’s fair to say that the results of all this innovation have, so far, been decidedly mixed.
Not all value-based payment initiatives have resulted in improvements in health care value, and it is unclear why some programs have worked while others have not.
Meanwhile, much of the discussion about value-based payment focuses on the relative merits of various payment models.[3]
But the high degree of definitional inconsistency makes it difficult to compare payment models and draw conclusions about their relative efficacy.
The implementation challenge, at the level of an entire health system
When it comes to value-based payment, perhaps the greatest challenge that health systems face today is how to implement value-based payment models at the level of an entire health system.
Even when individual payment initiatives demonstrate improved health care value, it is not immediately obvious how to knit them together into a comprehensive and coherent system-wide payment regime.
For example, what is the best way to organize payment for a patient with comorbidities who may use multiple parts of the health system-primary and acute care, or elective and emergency procedures-often concurrently?
So far, the global health care sector lacks clear, actionable strategies for health systems that want to implement value-based payment models at regional or national levels.
That system-wide level is the focus of this report.
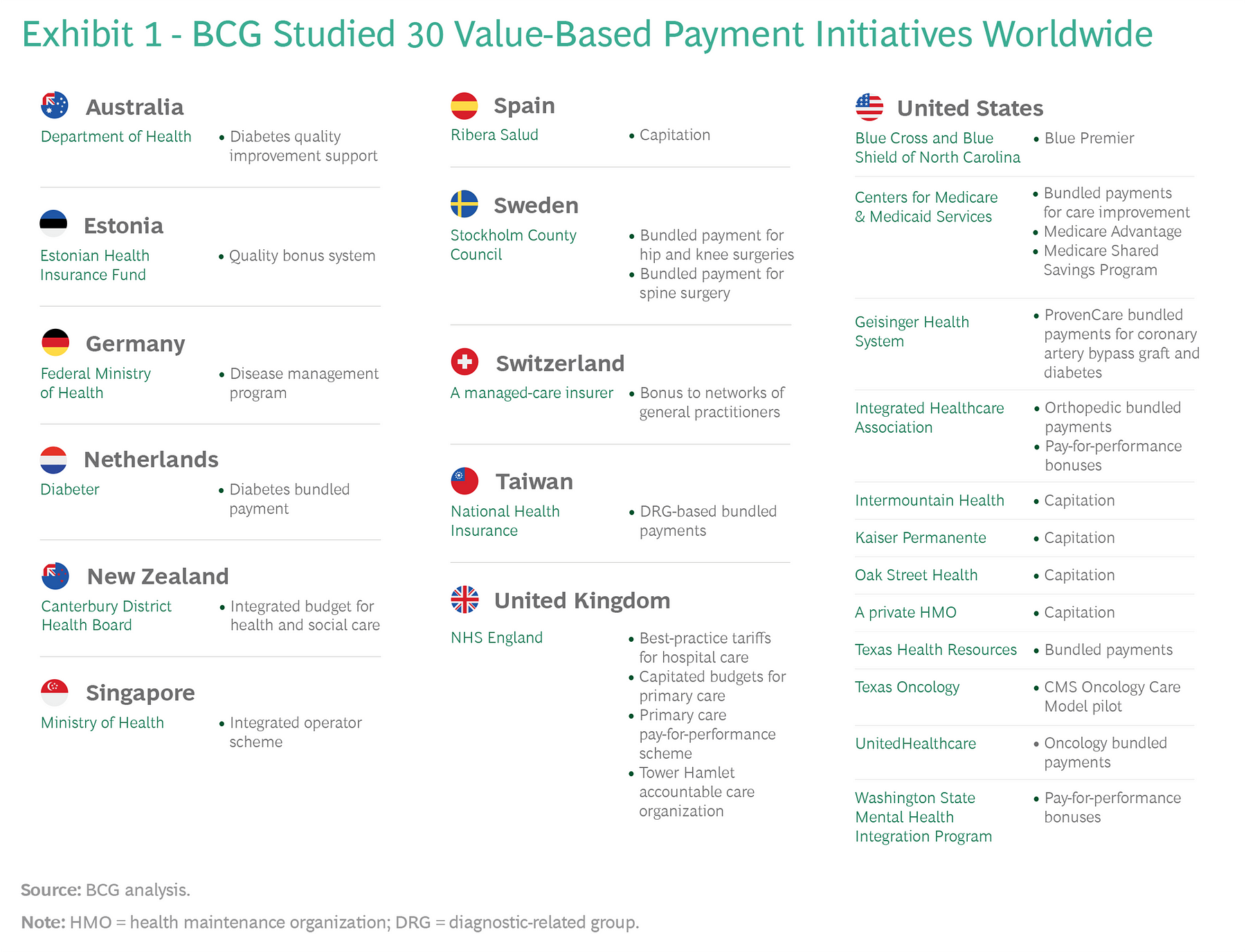
During the past year, BCG studied 30 value-based payment initiatives worldwide and reviewed the growing scientific literature about payment models.
We looked at programs initiated by public and private payers covering single provider organizations and multiple organizations, and by governments that are leaders in value-based health care as well as others that are just beginning to focus on value. (For a list of initiatives studied, see Exhibit 1.)
In addition to creating a clear and consistent taxonomy of value-based payment models, we identified best practices both within and across models and analyzed how various models can be linked together into a coherent system-wide design.
Our research led to three high-level conclusions:
- 1.Value-based payment isn’t an end in and of itself but, rather, a means to an end: creating a new organizational context in which improving health care value becomes a rational behavior for all stakeholders.
- 2.When it comes to changing behavior, financial incentives matter-but so do organizational cultures, norms, practices, and data and analytics.
Therefore, it is critical not to conceive of value-based payment in isolation but, instead, to see it as just one element in a broad system transformation that will require considerable investment and long-term institutional commitment. If initiatives are conceived narrowly as a way to achieve immediate short-term cost-savings, they are likely to fail.
- 3. No single value-based payment model is appropriate for all situations or all patient groups; rather, the challenge is to choose the right type of model for a given situation or patient group and to link different models together into a comprehensive value-based payment system.
In this report, we review the existing value-based payment models and discuss the advantages and disadvantages of each.
We then identify seven characteristics of successful value-based payment initiatives. We also propose three pragmatic interventions that leaders can use today to build coherent value-based payment systems-regardless of their organizations’ starting points or existing capabilities.
Finally, we discuss some common system challenges that leaders will encounter.
Originally published at https://www.bcg.com on January 8, 2021.
To download the PDF open the URL below:
http://image-src.bcg.com/Images/BCG-Paying-for-Value-in-Health-Care-September-2019_tcm9-227552.pdf












