Chapter 3 of : “Transforming healthcare with AI”
EIT Health — European Institute of Innovation and Technology
March 3, 2020
This is an excerpt of the report “ Transforming healthcare with AI. Impact on the workforce and organisations”, published in 2020 by EIT Health. Survey of 175 healthcare professionals, health investors and AI start-up founders and executives
Executive Summary
by Joaquim Cardoso MSc.
Chief Editor of “The Health Revolution” Institute
AI Health Unit @ Digital Health Institute
March 25, 2022
Introduction
- Despite the undeniable potential of the various technologies and applications, the jury is still out both on the potential impact of automation and AI as a spectrum of applications on healthcare practitioners and on the likelihood of adoption at scale in a way that could revolutionise healthcare delivery.
- In this early stage of AI evolution, it is hard to predict all the ways in which healthcare delivery will change, and there are multiple possible operational and business models that could emerge.
- To prepare to make the most of the opportunities AI offers to improve patient care, healthcare practitioners would need to start changing their approach to education, lifelong learning, teamwork, patient empowerment and consumerism; and welcome and integrate new categories of professionals, with hybrid “clinical+data” profiles, or entirely new profiles, such as data scientists.
- Automation and AI are often used interchangeably but are not the same thing.
- However, automation solutions increasingly involve an AI component in order to expand their flexibility and effectiveness in addressing the challenges faced by healthcare organisations and by individuals.
How will AI and automation change the activities of healthcare practitioners?
- AI’s impact will be felt across the healthcare workforce. At the heart of any change is the opportunity to refocus on and improve patient
- This improvement could include not only providing better diagnosis and more effective treatments, but also fundamental changes to clinician-patient interactions and reimagining patient-centric care delivery, such as AI-enabled home care and chronic disease management, each with its own effect on the quality of care and clinical outcomes.
- Overall, AI is expected to allow practitioners to operate at the top of their licence, focusing on those activities that add the most value for patients.
- AI is not expected to replace clinicians but rather augment their capabilities to deliver impact for patients and the health systems they serve.[1]
Less admin; more patient care
Administrative tasks
Administrative tasks absorb a tremendous amount of healthcare practitioners’ time, with some studies suggesting they can take up to 70 percent of a physician’s time, while nurses spend only around 40 percent of their time on direct or indirect care.[2]
Much of this administrative burden can be alleviated by well-designed AI solutions, which will not only mean more time spent with patients, but significantly higher job satisfaction.
A software to improve the speed and quality of document completion was implemented in East London’s Homerton NHS Trust, where turnaround time for clinical letters was · reduced from 17 days · to just two [5]
Improve operations primary and community-based care
AI can not only improve operations in hospitals, but also in primary and community-based care, including the out-of-hospital care of elderly and frail patients. For example, predictive scheduling …
Bed management and operating room
Two notable examples of healthcare capacity management are bed management and operating room (theatre) preparation and utilisation management.
Allowing staff to see available beds on digital displays in real time, rather than call other departments to confirm availability, frees up capacity from routine tasks to spend in clinical care.
Over time though, clinical staff can use the data generated to help inform an AI-augmented learning process that reduces system inefficiencies and delays; for instance, identifying the drivers of clinically unnecessary long stays.
Capacity Command Center
In 2016, the Johns Hopkins Hospital in the US launched a Capacity Command Center to better predict and manage patient flow; patients are now assigned a bed 30 percent faster once the decision has been made to admit them.[7]87
These solutions can lead to small, centralised bed management teams who take all that effort away from nurses, physicians and other practitioners.
Operating rooms
Operating rooms are a very different situation but also lend themselves to AI-based solutions. They are highly complex environments. Scheduling is complicated even without unplanned emergencies and disruptions.
Surgery
Overall, there are high expectations for AI in surgery. Using AI-based algorithms could predict time flow better, which could substantially increase efficiency and allow more patients to be cared for on a given day.”
Supporting clinical activities
Apart from supporting routine tasks, AI can also augment a range of clinical activities. It can speed up labour-intensive processes and give practitioners information that can lead to better patient outcomes and higher quality of care.
- Improve the speed and accuracy of diagnostics
- Improve the speed and accuracy of diagnosis and detection
- Identifying patients at risk of deterioration at the hospital — and in the community
- Detecting cardiac arrest during emergency calls
Easier access to more knowledge
- The traditional model of learning and care delivery has relied on physicians, nurses and other practitioners dedicating a lot of time to accessing and then memorising information, whether in early training, or in ongoing efforts to maintain their skills.
- AI could bring an enormous amount of relevant, curated and prioritised knowledge to the practitioner’s fingertips, creating new possibilities for both learning and care delivery.
There is a broad trend in the healthcare sector away from caring for patients in hospitals and towards more community-based care, … and home-based care is also on the rise — where this applications could be leveraged.
New activities and new skills
- New technologies inevitably lead to new types of activities for healthcare practitioners — not least because of changes to the way patients themselves interact with the healthcare system — and entirely new skills to help them navigate this digital world.
A new way of interacting with patients
- Patients already have unprecedented to access medical knowledge.
- The introduction of AI solutions, especially e-triage or self-diagnostic tools, may exacerbate the trend for patients to attend a consultation with a preformed view on likely diagnosis and treatments.
- But the quality of information patients has can also be significantly better.
AI-enabled solutions are also increasingly available for care delivery, including for patients to administer care themselves, and there have been increasing efforts to allow for the prescription and reimbursement of “digital medicine”. In Germany, as of 2020, patients can be prescribed digital apps, including digital diaries for diabetes, … among others.
Boosting digital skills in the broader healthcare workforce
- Healthcare staff have been working on their digital literacy for the past 15 years but it is still listed as a major priority in The Topol Review.[19]100
- Practitioners need not only to be able to use AI solutions, but assess when they are appropriate for patients and those on the front line need to explain them to those patients.
- This requires a mixture of digital literacy and critical thinking skills rather than specific qualifications in statistics — and these skills are needed across all healthcare staff.
- Healthcare practitioners will undeniably need stronger technological skills in order to understand how AI works at a certain level of detail, while the data scientists and engineers will need some basic medical knowledge and strong communication skills to help them translate clinical requirements into technology solutions. All staff will need both digital and genomics literacy.
- In the healthcare sector in Europe, the highest growth in skills demand by 2030 will be for basic digital skills
Introducing new professionals in healthcare
- Multiple roles will emerge at the intersection of medical and data-science expertise.
- These will be required to develop algorithms and turn them into products, implement those products in clinical workflows, apply new approaches at scale and establish the conditions to facilitate the application of AI. Designers, … Data architects … are some of the news roles.
- In other data-rich areas, such as genomics, new professionals will include ‘hybrid’ roles, such as clinical bioinformaticians, specialists in genomic medicine and genomic counsellors.
Last, although the ability to develop new approaches will be important to centres of excellence, being able to implement these approaches at scale will be essential if the benefits are to reach the majority of patients.
- Many new roles will be populated by science, mathematics and computer graduates, fulfilling roles in computational genomics, data science, public-health informatics and bioinformatics.
- The Topol Review suggests there is an urgent need for health systems to attract and retain such scarce and valuable talent, for example, by developing flexible and exciting career paths and clear routes to healthcare leadership roles.
LONG VERSION (excerpt of Chapter 3, from sections 3.2 to 3.4)

Introduction
Despite the undeniable potential of the various technologies and applications reviewed in Chapter 2, the jury is still out both on the potential impact of automation and AI as a spectrum of applications on healthcare practitioners and on the likelihood of adoption at scale in a way that could revolutionise healthcare delivery.
In this early stage of AI evolution, it is hard to predict all the ways in which healthcare delivery will change, and there are multiple possible operational and business models that could emerge.
To prepare to make the most of the opportunities AI offers to improve patient care, healthcare practitioners would need to start changing their approach to education, lifelong learning, teamwork, patient empowerment and consumerism; and welcome and integrate new categories of professionals, with hybrid “clinical+data” profiles, or entirely new profiles, such as data scientists.
Automation and AI are often used interchangeably but are not the same thing.
However, as described in Chapter 2, automation solutions increasingly involve an AI component in order to expand their flexibility and effectiveness in addressing the challenges faced by healthcare organisations and by individuals.
Given that AI represents a subset of solutions referred to broadly as automation, in this report we draw on the MGI work on the impact of automation and AI across industries to explore the possible impact of AI on healthcare practitioners in Europe.
We complement this view with an activity-based perspective on the areas where AI can transform the lives of practitioners and a review of some of the new profiles that might be needed, to highlight the major changes organisations will have to address
3.2 How will AI and automation change the activities of healthcare practitioners?
Having considered the impact on the sector overall, we now turn our attention to how healthcare practitioners’ daily activities could change as AI and automation are introduced or scaled.
Given the spectrum of AI applications described in Chapter 2 (including varying levels of automation), it is not always possible to separate how much of the automation impact in healthcare we described in section 3.1 can be attributed solely to AI.
Many interviewees and survey respondents agree that AI’s impact will be felt across the healthcare workforce. They also agree that at the heart of any change is the opportunity to refocus on and improve patient care, especially for nursing.
As nurse Rebecca Love puts it, “Intelligent scheduling and staffing optimisation through AI would be a game changer for nurses.”
“Intelligent scheduling and staffing optimisation through AI would be a game changer for nurses.”
This improvement could include not only providing better diagnosis and more effective treatments, but also fundamental changes to clinician-patient interactions and reimagining patient-centric care delivery, such as AI-enabled home care and chronic disease management, each with its own effect on the quality of care and clinical outcomes.
“In the future, AI will not replace clinicians.
Clinicians who use AI will replace clinicians who do not use AI.”
Dr. Eyal Zimlichman, Sheba Medical Center
In this section, we discuss how the activities of practitioners will likely change as AI becomes more prevalent in the sector.
Overall, AI is expected to allow practitioners to operate at the top of their licence, focusing on those activities that add the most value for patients.
AI is not expected to replace clinicians but rather augment their capabilities to deliver impact for patients and the health systems they serve.[1]81
3.2.1 Less admin; more patient care
Administrative tasks
Administrative tasks absorb a tremendous amount of healthcare practitioners’ time, with some studies suggesting they can take up to 70 percent of a physician’s time, while nurses spend only around 40 percent of their time on direct or indirect care.[2] 82 ]
Much of this administrative burden can be alleviated by well-designed AI solutions, which will not only mean more time spent with patients, but significantly higher job satisfaction.
And, of course, making life easier for clinical staff increases the likelihood that they adopt and champion these solutions within the organisation.
As Robert Freeman from Mount Sinai Hospital says, “AI is going to help to bring back more joy to our nursing team. No one wants to spend half their day on data entry.”
“The best AI will be invisible to the workflow.”
David E. Albert, AliveCor
We have already seen some of the applications than can assume administrative tasks, such as clinical note takers using NLP abilities.
Speech recognition has been introduced in several clinical settings to address the vast amount of clinical documentation and here we focus on the potential impact in terms of actual resources needed in care.
For example, the South Tees Hospital NHS Foundation Trust Accident & Emergency (A&E) department, which provides healthcare services to around 1.5 million people in the UK, partnered with a private-sector provider to improve the speed and quality of document completion.[3]83
This dramatically changed activities across the A&E department:
· previously, 95 percent of staff were writing notes by hand or typing them;
· now 69 percent use speech recognition to complete clinical notes,
· saving on average 3½ minutes per patient in the main A&E unit — the equivalent of two full-time A&E clinicians a year.
Considering that an additional 2,200 A&E consultants are needed to fully address the staffing needs of all A&E departments across the UK, freeing up consultant time could have significant impact on the delivery of safe and timely care and on improving patient experience.[4]84
Similar software was implemented in East London’s Homerton NHS Trust, where turnaround time for clinical letters was
· reduced from 17 days
· to just two.[5]85
The Topol Review estimates that saving just one minute per clinical consultation would be the equivalent of the time worked by 230 A&E doctors, 600 outpatient hospital clinicians and 3,200 GPs.[6]86
Improve operations primary and community-based care
AI can not only improve operations in hospitals, but also in primary and community-based care, including the out-of-hospital care of elderly and frail patients.
For example, predictive scheduling — intelligently predicting which appointments are likely to overrun in a GP surgery and adapting appointment planning accordingly — and capacity management tools can help reduce waiting times for patients, improve patient experience and outcomes, and free up resources in elderly care.
This is especially important where delays in access to treatment could compromise clinical outcomes, such as in specific types of cancer diagnoses.
Bed management and operating room
Two notable examples of healthcare capacity management are bed management and operating room (theatre) preparation and utilisation management.
These logistical challenges involve matching available resources against expected demand or a planned schedule, taking into account patient context, frailty and comorbidities, demographics, seasonality, reduced capacity in neighbouring facilities etc., but also the specific hospital context such as the operating surgeon and surgical team, clinical protocols, levels of experience, peri-operative processes, protocols around anaesthesia and recovery, and so forth.
Not unlike airline operations, where matching an aircraft to a scheduled flight often needs to be revised to respond to disruption, AI solutions could allow hospitals to run operations more smoothly.
At one level, bed management is a digitisation effort that involves constantly monitoring admissions, discharges and patients moving within the hospital, to understand which beds are available.
Allowing staff to see available beds on digital displays in real time, rather than call other departments to confirm availability, frees up capacity from routine tasks to spend in clinical care.
Over time though, clinical staff can use the data generated to help inform an AI-augmented learning process that reduces system inefficiencies and delays; for instance, identifying the drivers of clinically unnecessary long stays.
Capacity Command Center
In 2016, the Johns Hopkins Hospital in the US launched a Capacity Command Center to better predict and manage patient flow; patients are now assigned a bed 30 percent faster once the decision has been made to admit them.[7]87
Singapore’s Tan Tock Seng Hospital, one of the country’s largest multidisciplinary hospitals, uses a similar system to replace a process where healthcare staff had to go through more than 300 rules during admission to correctly prioritise assigning beds.[8]88
These solutions can lead to small, centralised bed management teams who take all that effort away from nurses, physicians and other practitioners.
Operating rooms
Operating rooms are a very different situation but also lend themselves to AI-based solutions. They are highly complex environments. Scheduling is complicated even without unplanned emergencies and disruptions.
Determining how much time each patient will require, and exactly what resources they need is challenging.
Procedures often run longer than planned, leading to cancellations for procedures booked later in the day, or booking processes allow for significant gaps, leaving operating rooms underused. AI could free up valuable time for surgeons and other staff (e.g., anaesthetists, nurses), forecasting the likely time a procedure for a specific patient could take.
The Frederick Memorial Hospital in Maryland uses just such a tool and similar applications are being developed and implemented by hospitals and the private sector.
Surgery
Overall, there are high expectations for AI in surgery. As Todd Ponsky, Professor of Surgery at Cincinnati Children’s Hospital Medical Center, says, “The flow of patients through a busy operating room could be ‘smarter’.
Using AI-based algorithms could predict time flow better, which could substantially increase efficiency and allow more patients to be cared for on a given day.”
From just these two examples, it is clear that AI enabled solutions can take repetitive automatable tasks away from practitioners and can deliver operational efficiencies that allow physicians, nurses, and other clinical staff more time to spend on direct patient care.
There should be few impediments to adoption. A recurring theme from our interviews was that a reduction of administrative work is not just less controversial, it is top of most people’s wish list.
3.2.2 Supporting clinical activities
Apart from supporting routine tasks, AI can also augment a range of clinical activities.
It can speed up labour-intensive processes and give practitioners information that can lead to better patient outcomes and higher quality of care.
We have already looked at some examples in Chapter 2. Here, we will consider the implications for the daily lives of practitioners in more detail.
· Improve the speed and accuracy of diagnostics
· Improve the speed and accuracy of diagnosis and detection
· Identifying patients at risk of deterioration at the hospital — and in the community
· Detecting cardiac arrest during emergency calls
Improve the speed and accuracy of diagnostics
Radiology, pathology and ophthalmology are clinical disciplines already being reshaped by AI. In recent years, AI algorithms, and deep learning in particular, have made remarkable progress in image-recognition tasks.
They have thus propelled the field of medical-image analysis forward. These specialties involve large numbers of images delivered across different care settings, through interoperable systems.
The evidence basis for these technologies keeps expanding and specific technologies have been shown to perform as well as experts in medical-image analysis in selected trials and industry-led applications.[9]90
In radiology, trained physicians visually assess medical images to detect, characterise and monitor diseases.
But AI can automatically recognise complex patterns in imaging data and provide quantitative, rather than qualitative, assessments of radiographic characteristics.
It can be used in multiple stages of the workflow, helping with many of the steps required to improve patient safety, diagnostic accuracy and time-efficiency.
In these early stages, AI can help the physician determine the most appropriate imaging procedure and define personalised radiation doses during the imaging process, reducing patient exposure to radiation based on specific risk factors using machine-learning processes based on population data.[10] 91
During image capture, AI can analyse images as they are acquired, saving the physician time by performing relatively simple steps, from image rotation to real-time quality checks of the field to be acquired.
These AI-generated, physician-validated images can, in turn, be used to improve the underlying algorithms.
As Egil Samset from GE Healthcare Cardiology Solutions says, “The goal is to have fully AI-augmented workflows connected to treatment guidelines; allowing the physician to focus on care delivery.”
Automated segmentation, i.e., annotating the medical-imaging data, is another time-consuming step for physicians that can be supported using AI. Conservative estimates suggest that radiologists spend 60 percent of their time reviewing images.
AI can help the radiologist spot areas of interest and suggest the most likely diagnosis.[11]92
The Topol Review suggests that extrapolating results from breast-cancer-detection algorithms alone could reduce the time radiologists review images by 20 percent.
AI can also save physicians’ time by providing structured reporting, generating the bulk of the final report, linking words, images and quantitative data.
Adopting reporting standards could make the data more interoperable too, and feed into radiology case collections to teach both clinicians and algorithms.[12]93
Radiology today often employs “double reading” to reduce diagnostic errors, ensuring images are reviewed by two different radiologists.
Recent research suggests that if an AI system participates in the double-reading process (as happens in some UK hospitals), the AI performance is comparable to the double-reading results and could reduce the workload of the second radiologist by up to 88 percent.[13]94
Such advances will be necessary to allow physicians to cope with the sheer amount of healthcare data now being generated. “Twenty years ago, you would see maybe 100 X-rays per shift,” explains Dr. med. Dominik Pförringer, orthopaedic and trauma surgeon at TUM Hospital, “Through modern tomography, you will have a large multiple of this number.”
Once images are captured, they need to be triaged to decide which cases are more urgent and whether a patient requires more comprehensive imaging, such as an MRI. Dr. med. Pförringer compares AI to a hunting dog: “It has a better nose. An AI-enhanced CT scanner that tells me ‘in pictures 840–880 I saw some irregularities’ would be incredibly helpful. It could even identify detectable conditions that I am not looking for at that time.”
This ability to identify potential risks of disease onset, even when not specifically looking for them, could save lives, as radiologists often focus on a specific question while handling increasing amounts of imaging data. AI could be complementary to the radiologist’s diagnostic effort, always bearing in mind that, as radiologist Antanas Montvila says, “We are still going to be the ones signing the report.” Radiology today sees increasing applications of AI, from oncology (e.g., breast-cancer or prostate-cancer detection), to interpretation of chest radiographs and liver-lesion analysis.[14]95
Last, as discussed in Chapter 2, new solutions in Sheba Medical Centre, Israel, explore how AI based image reconstruction could help reduce the radiation exposure of a patient to 4 percent of a conventional CT, one of the highest volume diagnostics in Europe.
Improve the speed and accuracy of diagnosis and detection
There are many examples of how AI could help healthcare practitioners make decisions and supplement the diagnosis and detection process, from identifying hospital patients at risk of deterioration to detecting cardiac arrest during emergency calls.
Identifying patients at risk of deterioration at the hospital — and in the community
During a hospital stay some patients are, or can become, vulnerable to adverse outcomes caused by malnutrition, septic shock or acute respiratory failure.
Patients are typically evaluated against standardised clinical-risk scores and monitored routinely for deterioration.
AI-based warning systems can more accurately identify patients at risk.[15]96
For example, patients admitted to hospital with malnutrition have longer hospital stays, higher rates of 30-day readmission and an increased risk of infections.
Identifying patients at risk and treating the underlying causes early therefore improves patient outcomes and reduces strain on the hospital.
At the Mount Sinai Health System’s hospitals, algorithms are changing how dieticians work.
Previously, dieticians would move between wards trying to identify and prioritise patients based on preset criteria such as age or condition.
AI-based solutions are now integrated into patients’ EHRs and when a dietician logs in to the system for his or her morning round, a dashboard highlights the patients most likely to be malnourished and thus who should be seen first.
The algorithm ranks and colour-codes patients, but also allows sorting and filtering so dieticians themselves can quickly identify priority patients in their unit.
AI, yet again, is not a replacement for practitioners’ clinical judgement, but a tool that takes basic tasks out of the hand of clinicians so they can spend less time screening patients and more time caring for them.
IBM Research similarly highlights the potential of AI to change how hospital teams work when caring for epileptic patients, by preemptively detecting the likely onset of epileptic seizures.
An intensive-care unit can have an average of almost 700 alarms per patient per day and can process approximately 10 gigabytes of data per day.
Such data can be used in epilepsy research to observe conditions that exist before seizures, or to define correlations between the disease and nonadherence.
They can help clinical teams recognise seizures rapidly, while reducing the labour-intensive need for continuous in-person monitoring.
Outside the hospital, mobile technology and remote sensor-generated data and machine learning can allow care teams to deliver personalised seizure forecasting and seizure detection, reducing the time taken to administer medication when a seizure occurs.
Such approaches can be used to support at-home monitoring or, more broadly, the continuous monitoring of patients in resource-poor environments, and can reduce patient self-reporting, increasing the efficiency of clinical trials in this field.[16]97
Detecting cardiac arrest during emergency calls
Emergency services dispatchers have a variety of duties such as keeping callers calm, obtaining essential information, providing first-aid instruction and, vitally, determining what the caller requires in order to triage them correctly and advise on the correct first-aid procedure — all while handling vast volumes of calls and running the risk of not prioritising the most critical cases, which could have an impact in terms of lives saved or lost.
In Copenhagen, Corti, a startup, has used AI to analyse emergency calls in real-time and identify signs of cardiac arrest.
According to Corti, dispatchers recognise cardiac arrest over the phone in 73 percent of cases, while the algorithm, focusing on verbal and nonverbal patterns of communication such as the caller’s tone of voice, reportedly identifies it correctly in more than 93 percent of cases.
It also does so faster (which is critical, as each minute of delay reduces chances of recovery by 7–10 percent). The algorithm acts as a virtual assistant, prompting the dispatcher to ask certain questions and making a recommendation on whether the person concerned is suffering cardiac arrest.
Similar solutions could be developed to identify other critical conditions, such as a stroke or even heart attacks in women, who often present differently to men suffering heart attacks and are less likely to be spotted.[17]98
While such algorithms could revolutionise emergency care, the stakes are also high if an error is made.
For now, such solutions offer only guidance, which means the dispatcher needs a good understanding of the algorithm and its strengths and limitations in order to take the final decision.
3.2.3 Easier access to more knowledge
The traditional model of learning and care delivery has relied on physicians, nurses and other practitioners dedicating a lot of time to accessing and then memorising information, whether in early training, or in ongoing efforts to maintain their skills.
The volume of information has always been high, but recent advances in data and research output are making the effort almost insurmountable. Despite their best efforts and determination to deliver the best care possible, many clinicians feel they cannot keep up.
AI could bring an enormous amount of relevant, curated and prioritised knowledge to the practitioner’s fingertips, creating new possibilities for both learning and care delivery.
During early education, it could mean that examinations are less about memorising knowledge and more about delivering insights through learning, augmented by AI support, while honing clinical counselling skills — a trend already observed in some medical schools.
During practice, it could also give practitioners easy access to the latest advances in innovation so they can give their patients high quality personalised care.
Practitioners can focus more on the human component of their job, ensuring not only that they have the right diagnosis and treatment but that they have the time to coach, counsel and empower patients to self-care where appropriate, and take ownership of their health and wellbeing.
AI solutions would also allow practitioners to work more deeply with multidisciplinary teams to deliver truly integrated care across care settings (e.g., from hospital ward to primary care and home), shifting the healthcare system culture towards more collaboration, integration and joint ownership of clinical outcomes.
This potential of AI is now increasingly welcomed by clinicians. Anthony Chang, founder of AIMed, says, “As we try to create an ecosystem and a community of AI and clinical professionals, we now see a profound shift on both sides, but particularly among clinicians.”
3.2.4 Patient empowerment, self-care and remote monitoring
There is a broad trend in the healthcare sector away from caring for patients in hospitals and towards more community-based care, built on patient empowerment, self-care, and the technical possibilities of remote care and home monitoring. In addition, more emphasis is being placed on prevention and population-health management.
AI-enabled e-triage solutions, such as Ada, Babylon, Mediktor or K Health, could increasingly divert patients to appropriate solutions for their specific symptoms and underlying conditions. This could reduce the clinical workload — especially in primary and emergency care — and free up time for healthcare professionals to address patients with severe and urgent needs.
“It’s time to reduce paternalism in healthcare. Other industries involve the customer as much as possible. Why should medicine be different?”
Adolfo Fernández-Valmayor, Quirónsalud
Patients with chronic conditions will increasingly manage their disease helped by AI-enabled monitoring and decision support.
Diabetic patients have been some of the first to be involved in a degree of automated self-care. Historically, patients have monitored the progression of diabetes with pen and paper and through fortnightly visits to the hospital.
Digital apps now allow healthcare specialists to monitor patients remotely and AI-enabled continuous blood glucose monitors have allowed more accurate tracking of blood glucose levels.
Similarly, solutions such as the closed-loop “artificial pancreas” could allow type 1 diabetes patients to improve self-care and blood glucose control, while practitioners receive and review patient data remotely, reducing the need for regular physical examination.
Home-based care is also on the rise.
Most patients who need to recover from illness or surgery would rather do so at home, and health systems increasingly try to reduce clinically avoidable hospital stays or long lengths of stay.
Advances in monitoring technology and AI-augmented clinical-alert systems, could mean that even some patients with cardiac and blood-pressure complexities could be moved from the intensive-care unit to their homes with centralised monitoring from nurses and physicians.
Hospital-based professionals will need the right skills in order to work closely with AI teams to develop the right calibration, for example on risk-alert thresholds, and to ensure they can use resources most efficiently.
It is true that AI-enabled solutions are already learning and calibrating which alerts physicians perceive as more or less important — a trial in Israel is improving the frequency of alerts in radiology using algorithms based on the action physicians take following specific recommendations.
However, there is no doubt that physicians and other healthcare practitioners will need to be an intrinsic part of the AI development process.

3.3 New activities and new skills
New technologies inevitably lead to new types of activities for healthcare practitioners — not least because of changes to the way patients themselves interact with the healthcare system — and entirely new skills to help them navigate this digital world.
“Our job profile will change over time. AI will be able to do some tasks that take a lot of time. We are happy if we can delegate this and concentrate on diagnostic thinking and talking to patients. I don’t see any threat for radiologists through AI in the next 20 to 30 years.”
Felix Nensa, University Hospital Essen
3.3.1 A new way of interacting with patients
Patients already have unprecedented to access medical knowledge. Their expectations for digitally accessed services are high, carried over from more consumer-focused sectors. Indeed, patients are becoming more like consumers when accessing healthcare, evaluating options in advance and often coming into a consultation with information to discuss with their physician — even if that information is often erroneous.
The introduction of AI solutions, especially e-triage or self-diagnostic tools, may exacerbate the trend for patients to attend a consultation with a preformed view on likely diagnosis and treatments. The quality of this information can vary widely, which may lead to frustration as physicians need to address questions raised by incomplete or at times even erroneous information.
But the quality of information patients has can also be significantly better.
Physicians and other healthcare practitioners will be increasingly asked to give a second opinion — the first having been derived by an algorithm.
This will require the clinician to have a basic understanding of how these applications work, be able to discuss their limitations and whether they have been used appropriately.
But beyond that, it will require an open mind and a willingness to engage with the AIdriven recommendation.
It may even require additional consultation time, which may be alleviated by the increased digital and AI literacy of the wider patient population, potentially reducing the overall numbers of patients seeking frontline care.
“An acquaintance called me for a second opinion having first accessed an AI online triage tool while on holiday. They had been on a surfing vacation and reported a severe headache. AI made a correct diagnosis: a carotid dislocation. The patient took an aspirin and flew home. My work focuses on bones and joints — I would have not immediately thought about the vascular aspect. I was in fact distracted by the fact that the patient accessed the AI online triage tool first. I am now convinced this could be the future of medicine.”
Orthopaedic surgeon
As we have seen, AI-enabled solutions are also increasingly available for care delivery, including for patients to administer care themselves, and there have been increasing efforts to allow for the prescription and reimbursement of “digital medicine”.
In Germany, as of 2020, patients can be prescribed digital apps, including digital diaries for diabetes, apps to support physiotherapy or psychotherapy treatments or to measure blood pressure, which will be reimbursed by Germany’s statutory health insurance.[18]99
For physicians to prescribe such apps, they of course need to be aware of them and understand for whom they are appropriate and under what conditions.
They need to understand the relative advantages and limitations of AI solutions, as well as the ethical implications. If an AI-enabled solution could be an option for a patient, physicians will need to decide not only whether the technology is appropriate for the underlying condition, but also whether the patient will be able to use it correctly.
They will need to spend time introducing patients and caregivers to the technology and advise them on the implications of the clinical data generated.
This will be a world of transparency, collaboration and dynamic interaction between healthcare professional, patient, carer and AI provider, not only to improve outcomes but also to preemptively manage potential risks, including ones of calibration on how and when to use specific solutions.
3.3.2 Boosting digital skills in the broader healthcare workforce
Healthcare staff have been working on their digital literacy for the past 15 years but it is still listed as a major priority in The Topol Review.[19]100
Practitioners need not only to be able to use AI solutions, but assess when they are appropriate for patients and those on the front line need to explain them to those patients.
This requires a mixture of digital literacy and critical thinking skills rather than specific qualifications in statistics — and these skills are needed across all healthcare staff.
The MGI 2018 discussion paper, Skill shift: Automation and the future of the workforce, analysed these changing requirements, which has informed our discussion on changes needed for the healthcare workforce.
This new report takes an explicitly European perspective, using seven diverse European countries as a starting point.[20]101
Healthcare practitioners will undeniably need stronger technological skills in order to understand how AI works at a certain level of detail, while the data scientists and engineers will need some basic medical knowledge and strong communication skills to help them translate clinical requirements into technology solutions.
All staff will need both digital and genomics literacy. This means practitioners will need ongoing expertise and guidance to evaluate new technologies, based on real-world evidence and their understanding of data validity and accuracy.
“A massive shift needs to happen in education and training. We need to upskill the workforce as a whole — we cannot rely on pockets of specialist knowledge but need to embed the new skills across a range of disciplines. Claire Bloomfield, National Consortium of Intelligent Medical Imaging,”
University of Oxford
Exhibit 3.4 illustrates how much more time healthcare practitioners will need to spend using technology skills. Notably, the time spent using basic digital skills will more than double.
Exhibit 3.4 — In the healthcare sector in Europe, the highest growth in skills demand by 2030 will be for basic digital skills
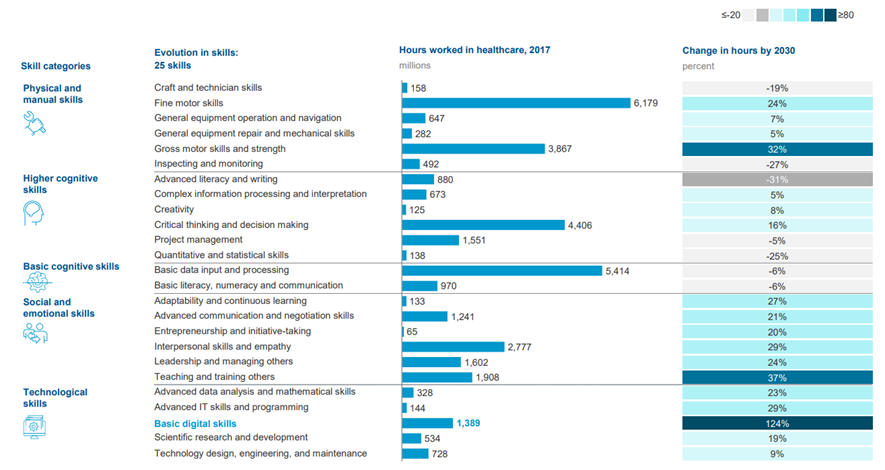
SOURCE: MGI. Selected European countries: France, Germany, Hungary, Italy, Portugal, Sweden, UK
The Topol Review identified specific areas for education and training related to AI and robotics such as health-data provenance, curation, integration and governance, ethics of AI and autonomous systems and tools, and critical appraisal and interpretation of AI and robotics technologies.[21]102
Now, more than ever in healthcare, there will be a professional imperative to stay relevant through a culture of ongoing learning and development, inclusivity and openness to change.
Health systems will need to enable such a shift, developing a structured learning philosophy and programme, as they help practitioners adapt to the scaling up of new technologies.

3.4 Introducing new professionals in healthcare
This report focuses primarily on the relationship between AI and today’s healthcare practitioners, but it is instructive to consider that the projected growth of AI solutions suggests that entirely new roles will need to enter the healthcare workforce.
Multiple roles will emerge at the intersection of medical and data-science expertise.
These will be required to develop algorithms and turn them into products, implement those products in clinical workflows, apply new approaches at scale and establish the conditions to facilitate the application of AI.
For example, medical leaders will have to shape clinically meaningful and explainable AI that contains the insights and information to support decisions and deepen healthcare professionals’ understanding of their patients.
This might include adapting algorithms to highlight those lab results that have the greatest bearing on the likelihood of a diagnosis and share comparable cases, rather than simply providing a risk score.
Clinical engagement will also be required in product leadership in order to determine the contribution of AI-based decision-support systems within broader clinical protocols.
Adapting algorithms into products that are usable and fit into clinical workflows will specifically require product leadership from senior clinicians. These are the people who can define protocols that benefit from the insights of AI but who are also able to use them safely and appropriately. To do this, medical leaders will require a deep understanding of the potential and limitations of the outputs from algorithms.
Designers specialising in human-machine interactions on clinical decision making will help create new workflows that integrate AI.
Data architects will be critical in defining how to record, store and structure clinical data so that algorithms can deliver insights, while leaders in data governance and data ethics will also play vital roles.
In other data-rich areas, such as genomics, new professionals will include ‘hybrid’ roles, such as clinical bioinformaticians, specialists in genomic medicine and genomic counsellors.
Institutions will have to develop teams with expertise in partnering with, procuring and implementing AI products that have been developed or pioneered by other institutions.
Orchestrating the introduction of new specialisations coming from data science and engineering within healthcare delivery will become a critical skill in itself. Experts in the ethics and legalities of data use, intellectual property questions when working with third parties, and best practices on data privacy and data governance, will also become increasingly important.
Last, although the ability to develop new approaches will be important to centres of excellence, being able to implement these approaches at scale will be essential if the benefits are to reach the majority of patients.
In fact, implementing AI approaches at scale is as challenging as their development and to do so successfully will require new roles in training, remodelling workflows and communicating the benefits of AI.
The 2018 AHA report describes the new positions, competencies and skill sets AI could create in healthcare, focusing on individual hospital organisations (Exhibit 3.5).[22]103
Exhibit 3.5 — AHA: new positions, competencies and skills
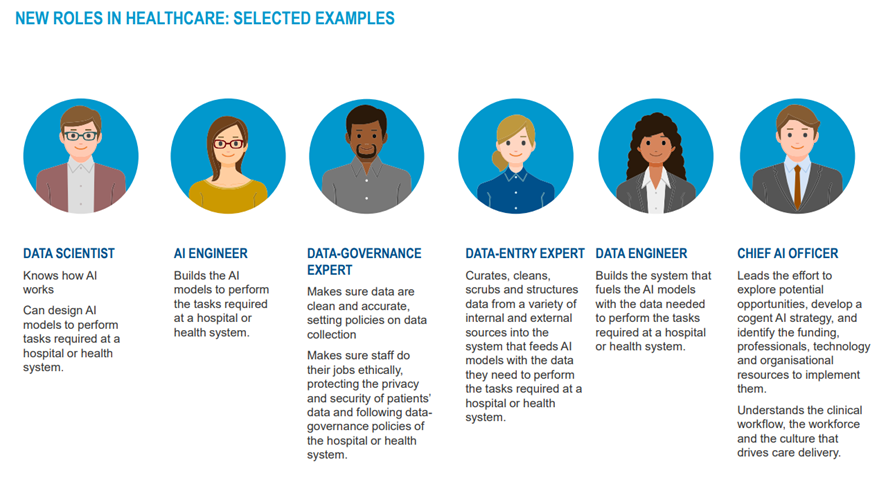
Adapted from AHA, “AI and the Health Care Workforce”, 2019, https://www.aha.org/
Many new roles will be populated by science, mathematics and computer graduates, fulfilling roles in computational genomics, data science, public-health informatics and bioinformatics.
Such professionals will be embedded across medical specialties, through the appointment of consultant-level bioinformaticians, and also across scientific specialties and within primary care environments.
The Topol Review suggests there is an urgent need for health systems to attract and retain such scarce and valuable talent, for example, by developing flexible and exciting career paths and clear routes to healthcare leadership roles.
This is an excerpt of the report “ Transforming healthcare with AI. Impact on the workforce and organisations; EIT Health and McKinsey & Company, (2020). Survey of 175 healthcare professionals, health investors and AI start-up founders and executives
References
[1] See also “Rads who use AI will replace rads who don’t”, Stanford University, November 2017, https://aimi.stanford.edu/ news/rsna-2017-rads-who-use-ai-will-replace-rads-who-don-t.
[2] Woolhandler, S., Himmelstein, D.U., “Administrative work consumes one-sixth of U.S. physicians’ working hours and lowers their career satisfaction”; Int J Health Services 2014; vol. 44; №4; Sinsky, C., et al., “Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties”, Ann Intern Med 2016; vol. 165, p.753–760; Donnelly, Laura, “Junior Doctors ‘spend up to 70 per cent of time on paperwork’”, The Telegraph, 8 December 2015, https:// www.telegraph.co.uk/news/health/news/12037469/Junior-doctors-spend-up-to-70-per-cent-of-time-on-paperwork. html. Westbrook, Johanna I., et al., “How much time do nurses have for patients? a longitudinal study quantifying hospital nurses’ patterns of task time distribution and interactions with health professionals”, BMC health Ser Res, 2011, vol. 11, №319.
[3] “The impact of clinical speech recognition in the Emergency Department at South Tees Hospitals NHS Foundation Trust”, Digital Health, 27 February 2018, https://www.digitalhealth.net/2018/02/impact-clinicalspeech-recognitionemergency-department-south-teeshospitals-nhs-foundation-trust/.
[4] Dr. Taj Hassan, President of the Royal College of Emergency Medicine, quoted in “NHS England urgently needs 2,200 more A&E consultants”, The Guardian, July 19, 2017.
[5] “NHS Trust Saves £150,000 a Year Using Clinical Speech Recognition”, The Journal of mHealth, November 29, 2018, https://thejournalofmhealth.com/nhs-trust-saves-150000-a-year-using-clinical-speech-recognition/.
[6] The Topol Review: Preparing the healthcare workforce to deliver the digital future, NHS, February 2019.
[7] “The Johns Hopkins Hospital Launches Capacity Command Center to Enhance Hospital Operations“, Johns Hopkins Medicine, October 26, 2016, https://www.hopkinsmedicine.org/news/media/releases/the_johns_hopkins_hospital_ launches_capacity_command_center_to_enhance_hospital_operations (accessed 6 January 2020).
[8] Basu, M., and Rohaidi, N., “Exclusive: Tan Tock Seng Hospital builds ‘artificial brain’ to manage services”, GovInsider, https://govinsider.asia/smart-gov/exclusive-tan-tock-seng-hospital-builds-artificial-brain-to-manage-services/ (accessed January 6, 2020).
[9] “What the radiologist should know about artificial intelligence — an ESR white paper”, Insights into Imaging, European Society of Radiology 2019, vol. 10, №44; McKinney, S.M., Sieniek, M., Godbole, V. et al. “International evaluation of an AI system for breast cancer screening”. Nature, 2020, 577, 89–94; Hosny, A. et al., “Artificial intelligence in radiology”, Nature, May 17, 2018, vol. 18, p. 500–510. https://www.nature.com/articles/s41568-018-0016-5.
[10] Remedios, D., et al., “Collaboration, campaigns and champions for appropriate imaging: feedback from the Zagreb workshop”. Insights Imaging 2018, vol. 9, №2, p. 211–214; Choy, G. et al., “Current applications and future impact of machine learning in radiology”. Radiology 2018, vol. 288, №2, p. 318–328; Hosny, A. et al., “Artificial intelligence in radiology”, Nature, May 17, 2018, vol. 18, p. 500–510. https://www.nature.com/articles/s41568-018-0016-5.
[11] The Topol Review: Preparing the healthcare workforce to deliver the digital future, NHS, February 2019.
[12] Rubin, D.L. and Kahn, C.E. Jr “Common Data Elements in Radiology”. Radiology 2017, vol. 283, №3, p. 837–844; Hong, Y., and Kahn C.E. Jr “Content analysis of reporting templates and freetext radiology reports”. J Digit Imaging, 2013, vol. 26, №5, p. 843–849.
[13] McKinney, S.M., Sieniek, M., Godbole, V. et al. “International evaluation of an AI system for breast cancer screening”. Nature, 2020, 577, 89–9.
[14] Codari, M., et al., “Artificial intelligence for breast MRI in 2008–2018: A systematic mapping review”. AJR Am J Roentgenol, 2019, vol. 212, p. 280–292 https://doi.org/10.2214/AJR.18.20389; Wang, J., et al., “Machine learningbased analysis of MR radiomics can help to improve the diagnostic performance of PI-RADS v2 in clinically relevant prostate cancer”. Eur Radiol, 2017, vol. 27, №10, p.4082–4090; Rajpurkar, P., et al., “Deep learning for chest radiograph diagnosis: A retrospective comparison of CheXNeXt to practicing radiologists”. PLoS Med, 2018, vol. 15, №11; Yasaka, K., et al., “Deep learning with convolutional neural network for differentiation of liver masses at dynamic contrastenhanced CT: A preliminary study”, Radiology, 2018, vol. 286, №3, p. 887–896.
[15] Alaa, A M, et al., “Personalized risk scoring for critical care prognosis using mixtures of Gaussian processes”, IEEE Transactions on Biomedical Engineering, 2018, vol. 65, №1.
[16] When data meets disease head-on: new trends in treating and managing epilepsy, IBM Research, October 2018, https://researcher.watson.ibm.com/researcher/files/au1-sharrer/EpilepsyWP_Nov2018.pdf.
[17] “AI that detects cardiac arrest during emergency calls will be tested across Europe this summer”, The Verge, April 25, 2018, https://www.theverge.com/2018/4/25/17278994/ai-cardiac-arrest-corti-emergency-call-response.
[18] “Germany introduces Digital Supply Act to digitalise health”, Healthcare IT News, November 13, 2019, https://www. healthcareitnews.com/news/europe/germany-introduces-digital-supply-act-digitalise-healthcare. Providers will have to prove to the federal Institute for Drugs and Medical Devices (BfArM) that their apps can improve patient care.
[19] Muro, Mark et al., Digitization and the American workforce, Brookings Institute, November 2017.
[20] France, Germany, Hungary, Italy, Portugal, Sweden and the UK.
[21] The Topol Review: Preparing the healthcare workforce to deliver the digital future, NHS, February 2019.
[22] AI and the Health Care Workforce, American Hospital Association, 2019, https://www.aha.org/system/files/media/ file/2019/09/Market_Insights_AI_Workforce_2.pdf.












