The Biden Administration has committed to increasing access to at-home tests … with plans to announce a $1 billion investment … Medicaid will also cover at-home tests
TIME
BY ALICE PARK
OCTOBER 7, 2021
Image: yalemedicine
As we close in on two years of living with COVID-19, quick and accurate tests for COVID-19 remain an urgent priority. In fact, as schools reopen, businesses resume operations and people return to work, rapid testing could be the key to preventing Delta or any new variants of SARS-CoV-2 from flaring into even larger outbreaks.
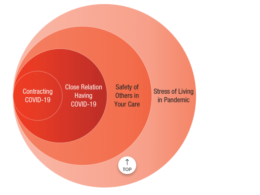
But that’s only if testing is used in the right way, at the right time and in the right places. With more opportunities for people to interact in public settings where the virus can spread, it’s never been more important to know who is infected and potentially seeding new COVID-19 infections, and who is not. But that doesn’t mean that blanket testing, especially using the rapid at-home tests now available at pharmacies and other retailers, will be the answer. Knowing when to use these tests, and how to interpret the results, are essential, say experts. And that means understanding what the tests can do, and what they can’t.
What’s the difference between at-home tests and the tests that a hospital, doctor’s office or lab perform?
The at-home kits that have been authorized by the U.S. Food and Drug Administration (FDA) are antigen tests, which means they can pick up things that the virus makes or shed, like proteins, but not the virus’s actual genetic material. So a positive antigen test picks up signs that the SARS-CoV-2 virus was or is present, similar to hairs that people or pets shed as a trail of where they’ve been.
Polymerase chain reaction (PCR) tests are the type that health care facilities or testing labs are most likely to use. They pick up the presence of viral genes. These tests are more sensitive, able to detect even a whisper of the virus’ genes and amplify that signal, while it takes a certain amount of viral protein to trip the alarms for an antigen test.
That difference also points to a major distinction in when the tests are most helpful. PCR tests can pick up the presence of old, non-active virus for weeks and even months after infection, says Dr. Michael Mina, assistant professor of epidemiology at Harvard T. H. Chan School of Public Health. It’s why the CDC suggests that if you get a positive PCR test for COVID-19, to wait for several weeks before getting another test to make sure the PCR isn’t still picking up the previous infection.
PCR tests may be more accurate, but because antigen tests require higher amounts of virus to produce a positive result, these tests are much more likely to identify people who are infectious and carrying around a heavy load of virus that can easily spread and infect others. That’s why Mina has been very vocal about the need to increase availability and access to at-home tests, so more people can have some reassurance of their COVID-19 status when it matters most: before they go to school, before they enter a restaurant, workplace or sports event, or before they attend a small private gathering. For these situations, a real-time result is more reliable and reassuring than one from a PCR test taken several days ago. “If you want to keep businesses running, or to be able to host a safe dinner at home, don’t ask people to get a PCR test two days before,” says Mina. “Ask them to use a rapid test within two hours of coming over. If a rapid test two hours before going to someone’s home is negative, it’s extremely unlikely that person is infectious and a risk to other people. It’s an extraordinarily effective way to keep dinner, concerts, workplaces and schools safe. Will it keep them 100% safe? No, but it will likely be 100% effective in stopping super spreaders from entering gatherings.”
Is an at-home test as reliable as a PCR test?
The gold standard test for diagnosing COVID-19 is a PCR test that laboratories perform. But antigen tests are typically 80–90% reliable in detecting the presence of SARS-CoV-2 proteins, which are a red flag that someone might be infected. These antigen tests are also especially good at identifying when an infected person is most contagious and likely to spread the virus to others.
Do at-home tests require a prescription?
There are several at-home tests now available over-the-counter, without a prescription, including ones made by Abbott, Becton Dickinson, Ellume, OraSure and Quidel. Generally the kits contain two tests, so people can repeat the test a day or two apart to verify the results. The FDA also just authorized a new at-home COVID-19 test from Acon Laboratories.
How do at-home testing kits work?
These kits, sold at pharmacies and other retailers like Walmart and grocery stores, can be broken down into two groups: at-home collection kits, and at-home testing kits.
Collection kits allow people to collect a sample, such as saliva or a nasal swab, at home, but you have to send that sample to a predetermined lab in order to get results.
At-home testing kits let you swab your nose and then smear the swab on a pre-treated card to which you add a provided solution. The results, like those of a pregnancy test, appear in a few minutes. Some of these kits also come with a phone number to a telehealth professional who can observe you taking the sample and doing the test and then verify the result with a digital certificate, if that’s what your employer or other organization requires. The completely DIY self-testing kits don’t provide such certification.
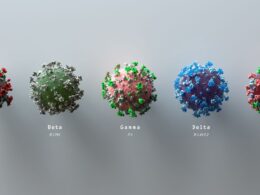
Can at-home tests detect the Delta variant?
Currently available COVID-19 tests, including PCR tests, are designed to detect any version of SARS-CoV-2, and are not specific for different variants.
When should I use an at-home test?
Doctors and public health officials are divided over who should use at-home rapid tests. The CDC recommends that workplaces, schools or other organizations take advantage of rapid tests among people who aren’t vaccinated, to determine if they are infected and could spread COVID-19.
Many doctors, however, recommend them only for people with symptoms, such as a runny nose, fever or cough, who want to know if they have COVID-19 or the flu (or any other respiratory infection, for that matter).
“These tests are best used to assist diagnosis of symptomatic COVID-19,” says Omai Garner, director of clinical microbiology for the University of California, Los Angeles Health System and director of point of care testing “I hold a strong line there.”
He doesn’t support more frequent, routine testing of people without symptoms because as more people perform more tests, the small chance of false positives only increases.
That’s especially true in areas where there is relatively high vaccination coverage and low prevalence of disease. “Doing regular antigen testing among people without symptoms in a low [COVID-19] prevalence setting is really just asking for false positives,” he says. “I do not think they should be used for asymptomatic screening for any reason.”
Mina, on the other hand, points out that for public health purposes, knowing people’s COVID-19 status based on asymptomatic screening can be useful in controlling spread of the disease, especially since many people are infected without showing symptoms. As more students return to school, testing kids before they board the bus could alert parents, and schools, to when kids should stay home if they’re infected. Mina also thinks at-home rapid tests should be used before people enter workplaces, board a plane or attend a sports event, among other scenarios. The idea is to know quickly who is infected and who isn’t to ensure everyone is safe.
What about false positives for at-home tests?
No test, including the gold standard PCR tests, are 100% sensitive, so false positives and false negatives are always a possibility.
(Ellume, an Australia-based manufacturer, recently recalled 200,000 test kits after one of the components of the test led to inaccurate false positive results.) But generally, the rate of false positives for at-home tests is relatively low, and
Mina suggests an easy way to address that problem. If you get a positive result, try testing again with another test; if it too is positive, then it’s likely accurate.
Mina also points out that rapid testing has a different purpose than PCR testing.
A PCR test is an important tool for the medical community — for doctors and health care workers to confirm if someone is infected with SARs-CoV-2. At-home rapid tests also identify people who are infected, but for a different, broader purpose — these tests are most useful in finding people who are infectious or contagious, and therefore shouldn’t be going out in public settings.
The rapid antigen tests are more of a public health tool, and so don’t have to do what PCR does and pick up any shred of SARS-CoV-2, including residual, inactive virus from an old infection. It’s like the difference between having a TSA agent at the airport ask every passenger to open their bags and then inspect each one by hand — the PCR standard — or scanning every bag through a detector — the rapid antigen standard. Yes, the latter may miss some security breaches, but it will likely pick up the most obvious ones.
Are states or the U.S. government going to start paying for at-home tests?
The Biden Administration has committed to increasing access to at-home tests.
On Oct. 6, the New York Times reported that the White House plans to announce a $1 billion investment to make more at-home tests available, quadrupling the number of kits available for consumers by the end of the year.
To make testing more accessible, earlier this year the Biden Administration asked retailers like Amazon, Walmart and Kroger to sell at-home test kits at cost rather than for profit, which could save people about 35% from the current $25-$30 cost per kit.
Medicaid will also cover at-home tests, and the federal government will send 25 million testing kits to 1,400 community health centers and food banks around the country so more people can take advantage of knowing their COVID-19 status.
On Oct. 6, the New York Times reported that the White House plans to announce a $1 billion investment to make more at-home tests available, quadrupling the number of kits available for consumers by the end of the year.
Medicaid will also cover at-home tests, and the federal government will send 25 million testing kits to 1,400 community health centers and food banks …
Originally published at https://time.comWhy, When and How to Test At-Home for COVID-19
What experts say about the best way to use at-home COVID-19 testing kitstime.com
Names cited:
Omai Garner, director of clinical microbiology for the University of California, Los Angeles Health System and director of point of care testing;
Dr. Michael Mina, assistant professor of epidemiology at Harvard T. H. Chan School of Public Health.