Health N Tech Transformation
strategy institute
Joaquim Cardoso MSc
Chief Researcher for : Health N Tech Transformation — Institute
Chief Editor for : Health N Tech Transformation — Portal
Chief Senior Advisor for: Health N Tech Transformation — Advisory Consulting
May 24, 2023
ONE PAGE SUMMARY
CVDs are the leading cause of mortality and amount to about a third of all global deaths
- The estimated number of deaths due to CVDs globally increased from around 12.1 million in 1990 (equally distributed between males and females) …
- … to 18.6 million (9.6 million males and 8.9 million females) in 2019.
- While the number of deaths due to CVDs over the last 30 years has increased globally — in large part due to an ageing and growing population — the age-standardised death rate has declined by one third, from 354.5 deaths per 100,000 people in 1990 to 239.9 deaths per 100,000 people in 2019. This decline has slowed in recent years and is beginning to stall in some regions.
Global progress against cardiovascular disease (CVD) is flatlining.
- More than half a billion people around the world continue to be affected by cardiovascular diseases, which accounted for 20.5 million deaths in 2021[1] — close to a third of all deaths globally and an overall increase on the estimated 121 million CVD deaths.
- Up to 80% of premature heart attacks and strokes can be prevented.
There are, baseline approaches that every country should implement to lay the foundation from which to build tailored activities to tackle CVDs. This includes:
- implementing major policy initiatives that are essential to improving CVD health — such as National Tobacco Control Programmes,
- securing the availability of CVD drugs, and
- creating an Operational Unit in the Ministry of Health responsible for tackling non-communicable diseases (NCDs).
- Additionally, it requires adequately funding health systems and initiatives so that all communities can access the care they need.
EXECUTIVE SUMMARY

World heart report 2023 — Confronting the world’s number one killer
World Heart Federation (WHF).
Mariachiara Di Cesare, Honor Bixby, Thomas Gaziano, Lisa Hadeed, Chodziwadziwa Kabudula, Diana Vaca McGhie, Jeremiah Mwangi, Borjana Pervan, Pablo Perel, Daniel Piñeiro, Sean Taylor, Fausto Pinto.
Reviewers: Victor Aboyans, Álvaro Avezum, Rick Chazal, Jean-Luc Eiselé, Naomi Herz, Andre Pascal Kengne, Angela Koh, Amam Mbakwem, Jagat Narula, Gregory Roth, Saate Shakil.
Editor: Edward Fox.
The World Heart Report 2023 was made possible through support from Novartis Foundation.
KEY MESSAGES:
EXECUTIVE SUMMARY
Overview
Global progress against cardiovascular disease (CVD) is flatlining. Though rates of CVD deaths globally have fallen in the last three decades, this trend has begun to stall and, without concerted efforts, is at risk of reversing.
More than half a billion people around the world continue to be affected by cardiovascular diseases, which accounted for 20.5 million deaths in 2021[1] — close to a third of all deaths globally and an overall increase on the estimated 121 million CVD deaths.
Up to 80% of premature heart attacks and strokes can be prevented. The world has the tools and knowledge to mitigate harms to cardiovascular health, particularly with the advances in cardiovascular medicine in the last 50 years.
But too often the tools that can help diagnose, prevent, and treat CVDs are not benefitting the communities who need them most.
Around 4 in every 5 CVD deaths occur in low- and middle-income countries and progress in cardiovascular health is increasingly concentrated in High-Income countries — a glaring health inequity that must urgently be addressed.
There is no one-size-fits-all approach to improving cardiovascular health globally.
Every population is susceptible to different risk factors based on where they live and their lifestyles.
Whether that’s having higher prevalence of tobacco and alcohol use and higher sodium intake or being more exposed to dangerous levels of air pollution and having lower levels of physical activity.
This means that decision makers and stakeholders must look closely at the risk factor prevalence in their countries and regions to fully understand what policy areas need more focus to get CVD health moving in the right direction.
There are, however, baseline approaches that every country should implement to lay the foundation from which to build tailored activities to tackle CVDs.
This includes
- implementing major policy initiatives that are essential to improving CVD health — such as National Tobacco Control Programmes,
- securing the availability of CVD drugs, and
- creating an Operational Unit in the Ministry of Health responsible for tackling non-communicable diseases (NCDs).
Additionally, it requires adequately funding health systems and initiatives so that all communities can access the care they need.
The stalling progress in CVD health is not unique.
Almost every health initiative around the world suffered because of the COVID-19 pandemic and countries are now grappling with which areas to prioritise as they aim to boost and protect the health of their populations.
Given the severe burden of CVDs both in terms of mortality and morbidity, this area of health cannot be neglected.
The world will struggle to meet the ambitious targets it set to reduce premature mortality from NCDs by 25% compared to 2010 levels, by 2025.
There is still time, however, to accelerate action toward meeting the Sustainable Development Goal 3.4 of reducing by one-third premature mortality from NCDs, including cardiovascular diseases.
This goal aligns with the World Heart Federation’s (WHF) World Heart Vision 2030.
WHF, with its membership of more than 200 heart foundations, scientific societies, and patient organizations across more than 100 countries, is a committed partner to resuscitating progress on CVDs.
To help promote action at every level against CVDs, this report provides the following key recommendations:
1.Countries and other relevant stakeholders should continue efforts to improve data for CVDs and their risk factors, particularly in LMICs where data gaps exist. This will help to understand why certain populations are at higher risk for certain CVDs.
2.Countries should ensure that their health expenditure as a percentage of GDP is at least 5%, in line with recommendations from the World Health Organization.
3.Countries should implement policies to combat CVDs, guided by the burden of disease and predominant risk factors, and ensure that their implementation is adequately resourced and monitored for progress.
4.As a matter of urgency, countries should prioritise coverage of interventions for the prevention and management of CVDs in Universal Health Coverage (UHC) benefit packages to help minimize out-of-pocket expenditure.
5.Lessons-learned in improving CVD prevention, management and improved access to care and therapies need to be implemented across all regions to address inequities and the uneven progress in CVD mortality declines.

KEY FINDINGS
CVD mortality
- CVDs are the leading cause of mortality and amount to about a third of all global deaths
- The estimated number of deaths due to CVDs globally increased from around 12.1 million in 1990 (equally distributed between males and females) to 18.6 million (9.6 million males and 8.9 million females) in 2019.
- While the number of deaths due to CVDs over the last 30 years has increased globally — in large part due to an ageing and growing population — the age-standardised death rate has declined by one third, from 354.5 deaths per 100,000 people in 1990 to 239.9 deaths per 100,000 people in 2019. This decline has slowed in recent years and is beginning to stall in some regions.
- The decline in death rates for CVDs has been much faster in High-Income countries (HICs) compared to low- and middle-income countries (LMICs), where more than 80% of CVD deaths occur globally. The world is far from achieving the equitable distribution of prevention, diagnosis, and treatment of CVDs.
- In 2019, for females, no region, other than Latin America and the Caribbean, had registered a decline in the CVD death rate to the level registered in the High-Income region in 1990.
- The highest levels of age-standardised CVD death rates occur in the Central Europe, Eastern Europe, and Central Asia region and the North-Africa and Middle East region.
- Ischaemic heart disease is the leading cause of CVD mortality in all regions except for females in Sub-Saharan Africa and for both males and females in South Asia (where stroke is the main cause).
- In most regions, age-standardised CVD death rates are higher in males than in females; however, in a large proportion of West African countries, females are at a higher risk of dying due to CVD than males.
- There is a correlation between lower expenditure on health as a percentage of GDP and higher CVD mortality.
In addition, the higher the proportion of out-of-pocket expenditure for health, the higher the CVD mortality.

CVD risk factors
- Raised blood pressure is the leading CVD risk factor globally and contributed to about 10.8 million deaths in 2021.
- Most CVD risk factors, including physical inactivity, alcohol consumption, tobacco smoking, raised blood pressure, and diabetes are higher in males in comparison to females.
- Obesity is the only risk factor that is higher in females.
- The distribution of CVD risk factors varies markedly by region.
For example, countries in the Sub-Saharan Africa region are among those with the highest prevalence of raised blood pressure, while countries in the Southeast Asia, East Asia and Oceania region have among the highest sodium consumption and prevalence of diabetes.
Countries in South Asia are among those with the highest levels of ambient air pollution.
- The distribution of CVD risk factors varies by sex.
For example, for males the prevalence of smoking is highest in the Southeast Asia, East Asia, and Oceania region while for females it is highest in the High-Income region.
The North Africa and Middle East region had the highest prevalence of obesity for females and the Southeast Asia, East Asia, and Oceania had the highest for males.
Non-HDL levels are highest in the Central Europe, Eastern Europe and Central Asia region for males and females.
WHF Policy Index
- The WHF Policy Index showed that the lowest implementation of key policies for improving CVD health is in the Sub-Saharan Africa region, where over 50% of the countries do not have availability of CVD drugs in public health facilities, a CVD National Plan or an NCD Unit.
- Globally, 106 countries (64% of 166 countries with available information), have implemented at least 7 of the 8 policies.
- The largest proportion of countries with the maximum score (8) were in the South Asia region (80%), the Central Europe, Eastern Europe, and Central Asia region (68%), and the High-Income (62%) region.

Key Recommendations:
All countries and stakeholders must urgently unite to accelerate efforts on improving CVD health and get progress back on track so that Sustainable Development Goal 3.4 of reducing by one-third premature mortality from NCDs can be achieved. This goal aligns with the World Heart Federation’s (WHF) World Heart Vision 2030.
To help promote action at every level against CVDs, WHF recommends the following, which are complementary to other key recommendations included in recent policy briefs and reports:
1.Countries and other relevant stakeholders should continue efforts to improve data for CVDs and their risk factors, particularly in LMICs where data gaps exist. This will help to understand why certain populations are at higher risk for certain CVDs.
3.Countries should ensure that their health expenditure as a percentage of GDP is at least 5%, in line with recommendations from the World Health Organization.
4.Countries should implement policies to combat CVDs, guided by the burden of disease and predominant risk factors, and ensure that their implementation is adequately resourced and monitored for progress.
4. As a matter of urgency, countries should prioritise coverage of interventions for the prevention and management of CVDs in Universal Health Coverage (UHC) benefit packages to help minimize out-of-pocket expenditure.
Lessons-learned in improving CVD prevention, management and improved access to care and therapies need to be implemented across all regions to address inequities and the uneven progress in CVD mortality declines.

SELECTED IMAGES
GLOBAL BURDEN OF CARDIOVASCULAR DISEASES MORTALITY
- CVDs are the leading cause of mortality and a major contributor to disability.
- Globally, the estimated number of deaths due to CVDs increased from around 12.1 million in 1990 (equally distributed between males and females) to 18.6 million (9.6 million males and 8.9 million females) in 2019 (Figure 1).
Figure 1: Global trends in number of deaths due to cardiovascular diseases, 1990–2019.
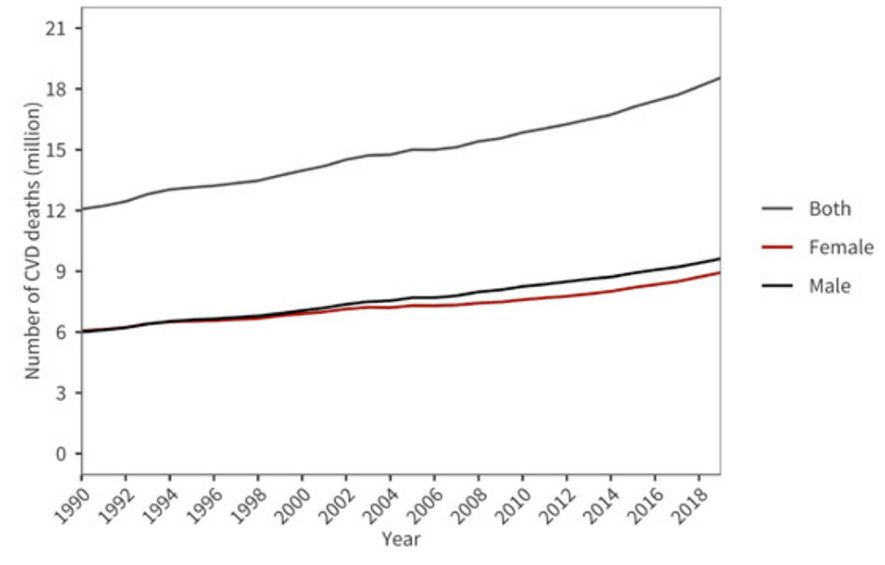
Source: Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington, 2020. Available from http:// vizhub.healthdata.org/gbdcompare. (18 March 2023).
- The number of deaths due to CVDs in 2019 represented 33% of all global deaths, with ischaemic heart disease (9.1 million deaths) …
- … and stroke (6.6 million deaths) totalling 85% of all CVD deaths worldwide.
- While the number of deaths due to CVDs over the last 30 years has increased globally — in large part due to an ageing and growing population — the age-standardised death rate has declined by one third, from 354.5 deaths per 100,000 people in 1990 to 239.9 deaths per 100,000 people in 2019 (Figure 2).
Age-standardization is a technique used to better compare disease outcomes, such as death rates, across populations.
It calculates what the disease outcome would be if the population age-structure were the same for all countries. This allows an assessment of whether the observed differences are due to factors related to the disease, rather than the age structure of the population.
Figure 2: Global trends in age-standardised cardiovascular disease death rate (per 100,000 people), 1990–2019.
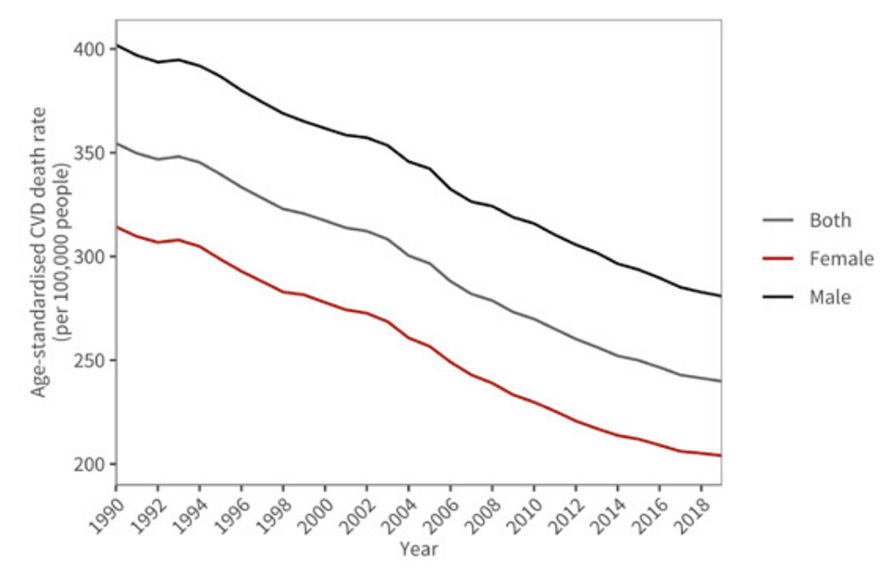
Source: Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington, 2020. Available from http://vizhub.healthdata.org/gbd-compare. (18 March 2023).
CVD death rates declined across all regions in this period, though the decline has been slowing in the past decade and is uneven across regions (Figure 3).
- The High-Income region, for example, experienced the fastest average rate of decline for both males and females from 1990 to 2019 (average annual rate of change of 2.6%).
- The slowest rate of decline in both sexes was observed in the Southeast Asia, the South Asia, East Asia and Oceania, and the SubSaharan Africa regions. Almost no improvement in CVD death rate for males was observed in these regions.
- Underscoring the disparities in progress, the death rate in the Sub-Saharan African region was 1.2 times higher than the High-Income region in 1990, whereas by 2019 the gap had grown to a death rate 2.1 times higher in Sub-Saharan Africa than in the High-Income region.
- The High-Income region had the lowest CVD death rate overall (102.1 and 153.8 deaths per 100,000 people for females and males respectively).
Only the Latin America and the Caribbean region achieved a decline in female death rates in 2019 that reached the rate the High-Income region had registered in 1990.
- For males, in 1990 the lowest levels of CVD death rate were recorded in Latin America and the Caribbean, Sub-Saharan Africa, and High-Income regions with South Asia only achieving a decline in 2019 that reached those levels.
The Central Europe, Eastern Europe and Central Asia region had the highest age-standardized CVD death rates for males and females in both 1990 (670.2 and 467.2 deaths per 100,000 people respectively) and 2019 (524.1 and 345.7 deaths per 100,000 people respectively).
The North Africa and Middle East region had the second highest rates for males and females in 2019 (376.7 and 339.8 deaths per 100,000 people for males and females respectively).

TABLE OF CONTENTS OF THE REPORT (TOC)
Executive Summary
Introduction
Global burden of cardiovascular disease mortality
Cardiovascular disease deaths by sex
Cardiovascular disease deaths by cause
Relationship between cardiovascular disease mortality and health expenditure
Cardiovascular disease premature mortality
Risk factors for cardiovascular diseases
– Physical activity
– Sodium intake
– Alcohol consumption
– Tobacco smoking
– Obesity
– Raised blood pressure
– Diabetes
– Lipids
– Ambient air pollution
Comparative levels of risk factors by country and region
The WHF Policy Index
Key findings
Key recommendations
Appendix — Supplementary Figures
References
[1] This report largely relies on 2019 data throughout, as that is the most recent year with the level of disaggregation required for analyses undertaken.
Citation
World Heart Report 2023: Confronting the World’s Number One Killer. Geneva, Switzerland. World Heart Federation. 2023.












