For the unrecognized depression group, annual direct healthcare costs averaged $10,463–149% higher than the $4,194 for people with no symptoms of depression
and 38% higher than the $7,564 for people who acknowledged having experienced depression in the past year.
This is a republication of the article below, under the title above, preceded by an Executive Summary by the editor of the blog.
Strategies to Address the Causality Dilemma of Depression and Chronic Illness
The healthcare industry needs to begin tackling depression head-on to focus on early detection and access to care.
MURRAY ZUCKER, MD
Chief Medical Director, Happify Health
Executive Summary
by Joaquim Cardoso MSc.
Chief Editor of “The Health Strategy Blog”
March 11, 2022
The Happify study
Happify’s Health Economics and Outcomes Research team’s conducted an analysis of the National Health and Wellness Survey. The findings are alarming:
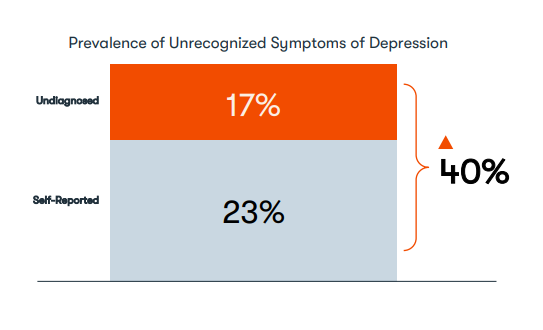
- Nearly one-in-five (17%) Americans have symptoms of mild to severe depression but are unable to correctly identify those symptoms.
- Healthcare costs attributed to this population are a staggering 38% higher than costs for people with the same levels of depression severity who are able to identify their symptoms.
- For the unrecognized depression group, annual direct healthcare costs averaged $10,463–149% higher than the $4,194 for people with no symptoms of depression and 38% higher than the $7,564 for people who acknowledged having experienced depression in the past year.
- The number of individuals suffering from depressive symptoms — both recognized and unrecognized — has been on the rise for years, but the pandemic exacerbated the problem
The previous Kaiser Family Foundation Report
Kaiser Family Foundation had reported that the number of adults with anxiety or depression increased 400% in the 19 months following the COVID-19-related lockdowns.
- What wasn’t clear, prior to the analysis of NHWS data, was the prevalence of mild to severe depression symptoms among people who reported “not experiencing depression” and “never being diagnosed with depression.”
- This is a group that would not have raised their hand in the KFF study to say, “yes I’m experiencing depression.”
- When this group is included in the data set, we found an additional 17% of the population had symptoms of unrecognized depression, on top of the 23% who were aware of their symptoms, putting the total number of people with mild to severe symptoms at 40% — a total of two-in-five Americans.
The methodology of the Happify Study
- The HEOR team used responses to the Patient Health Questionnaire-9 survey — an assessment used in clinical settings to measure the severity of depression symptoms — to find that 17% of people in the general population have “unrecognized” symptoms of depression.
- The analysis took multiple variables into account, including age, gender, demographics, and comorbidities.
- The data consistently showed that the segment with these “unrecognized” symptoms had higher direct healthcare costs and costs increased with the severity of depression.
The Cost of Undiagnosed Depression
- Not only does unrecognized and undiagnosed depression correlate to an increase in direct healthcare costs, it also impacts the patient’s total health.
- Another pivotal finding was the prevalence of depressive symptoms among people with specific chronic illnesses once those with unrecognized depressions symptoms were factored in:
- 71% — multiple sclerosis (including 20% with unrecognized symptoms)
- 69% — migraines (including 18% with unrecognized symptoms)
- 58% — heart failure (including 18% with unrecognized symptoms)
- 53% — arthritis (including 15% with unrecognized symptoms)
- 47% — Type 2 diabetes (including 13% with unrecognized symptoms)
- 42% — cancer (including 16% with unrecognized symptoms)
- 41% — hypertension (including 12% with unrecognized symptoms)
Early detection is key
- An estimated 132 million Americans — nearly 40% of the population — live in an area with a significant shortage in these providers, leaving patients waiting months for treatment once they decide to reach out for care.
- One part of the solution … is to permanently waive the rules that require clinicians to be licensed in the states where patients are located. …
- we also need to provide better guidance for the consumers who will use these products.
The Important Role for Digital Health Technology
- The role technology can play in healthcare becomes incredibly clear against the backdrop of COVID-19, a lack of providers, and the high number of Americans suffering from both recognized and unrecognized depression.
- Today, there are an estimated to 20,000 mental health apps available in the App Store, but less than 2% have been validated for safety and efficacy by studies or clinical trials.
- The Food and Drug Administration can’t actively regulate all of these apps, which means the entrepreneurs and investors who build them need to adhere to the rigorous scientific standards that exist to ensure patient safety.

ORIGINAL PUBLICATION
Nearly one-in-five (17%) Americans have symptoms of mild to severe depression but are unable to correctly identify those symptoms.
Healthcare costs attributed to this population are a staggering 38% higher than costs for people with the same levels of depression severity who are able to identify their symptoms.
Nearly one-in-five (17%) Americans have symptoms of mild to severe depression but are unable to correctly identify those symptoms.
Healthcare costs attributed to this population are a staggering 38% higher …
The findings are the result of Happify’s Health Economics and Outcomes Research team’s analysis of the National Health and Wellness Survey. We used the data to model the incremental burden of depression symptoms at the individual and population level.
When the team weighted the average healthcare costs by the severity of the depression symptoms, they found that the group failing to recognize their symptoms — the unrecognized depression group — had consistently higher costs.
For the unrecognized depression group, annual direct healthcare costs averaged $10,463–149% higher than the $4,194 for people with no symptoms of depression and 38% higher than the $7,564 for people who acknowledged having experienced depression in the past year.
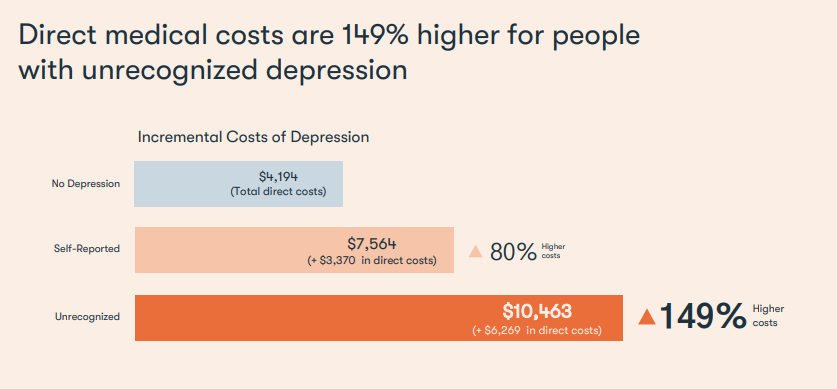
For the unrecognized depression group, annual direct healthcare costs averaged $10,463–149% higher than the $4,194 for people with no symptoms of depression and 38% higher than the $7,564 for people who acknowledged having experienced depression in the past year.
A National Dilemma
The Labor Department on January 25 issued its annual report to Congress on the Mental Health Parity and Addiction Equity Act of 2008.
As in years past, the report found that “health plans and insurance companies are falling short of providing parity in mental health … benefits.”
This year, however, Labor Secretary Marty Walsh said, “The pandemic is having a negative impact on the mental health of people in the U.S.,” and that “enforcement of this (mental health parity) law is a top priority for the Department of Labor.”
Growing Prevalence of Depression
The number of individuals suffering from depressive symptoms — both recognized and unrecognized — has been on the rise for years, but the pandemic exacerbated the problem.
At a time when people were deferring healthcare to prevent exposure to COVID-19, avoiding social activities and living in a constant state of fear and anxiety, Kaiser Family Foundation reported that the number of adults with anxiety or depression increased 400% in the 19 months following the COVID-19-related lockdowns.
The number of individuals suffering from depressive symptoms — both recognized and unrecognized — has been on the rise for years, but the pandemic exacerbated the problem
Kaiser Family Foundation reported that the number of adults with anxiety or depression increased 400% in the 19 months following the COVID-19-related lockdowns.
What wasn’t clear, prior to the analysis of NHWS data, was the prevalence of mild to severe depression symptoms among people who reported “not experiencing depression” and “never being diagnosed with depression.”
This is a group that would not have raised their hand in the KFF study to say, “yes I’m experiencing depression.”
When this group is included in the data set, we found an additional 17% of the population had symptoms of unrecognized depression, on top of the 23% who were aware of their symptoms, putting the total number of people with mild to severe symptoms at 40% — a total of two-in-five Americans.
the total number of people with mild to severe symptoms at 40% — a total of two-in-five Americans.

The Cost of Undiagnosed Depression
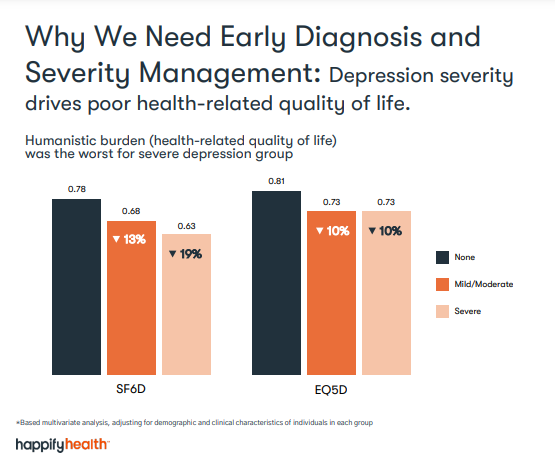
Not only does unrecognized and undiagnosed depression correlate to an increase in direct healthcare costs, it also impacts the patient’s total health.
Not only does unrecognized and undiagnosed depression correlate to an increase in direct healthcare costs, it also impacts the patient’s total health.
Our HEOR team used responses to the Patient Health Questionnaire-9 survey — an assessment used in clinical settings to measure the severity of depression symptoms — to find that 17% of people in the general population have “unrecognized” symptoms of depression.
These are people who scored 5 or greater on the PHQ-9 survey but reported having not experienced depression in the last 12 months. The PHQ-9 survey is part of the NHWS data.
Our HEOR team used responses to the Patient Health Questionnaire-9 survey — an assessment used in clinical settings to measure the severity of depression symptoms — to find that 17% of people in the general population have “unrecognized” symptoms of depression.
The analysis took multiple variables into account, including age, gender, demographics, and comorbidities.
The data consistently showed that the segment with these “unrecognized” symptoms had higher direct healthcare costs and costs increased with the severity of depression.
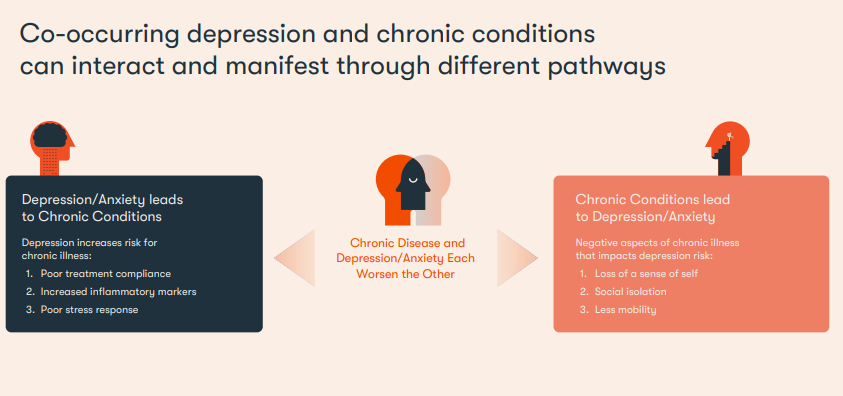
Another pivotal finding was the prevalence of depressive symptoms among people with specific chronic illnesses once those with unrecognized depressions symptoms were factored in:
- 71% — multiple sclerosis (including 20% with unrecognized symptoms)
- 69% — migraines (including 18% with unrecognized symptoms)
- 58% — heart failure (including 18% with unrecognized symptoms)
- 53% — arthritis (including 15% with unrecognized symptoms)
- 47% — Type 2 diabetes (including 13% with unrecognized symptoms)
- 42% — cancer (including 16% with unrecognized symptoms)
- 41% — hypertension (including 12% with unrecognized symptoms)
Another pivotal finding was the prevalence of depressive symptoms among people with specific chronic illnesses once those with unrecognized depressions symptoms were factored in
Early Detection is the Key
To address the impact on well-being, as well as the effect depression has on worsening chronic conditions, there needs to be greater focus on early detection and access to care when needed.
We must first address the unprecedented shortage of mental health professionals, including psychiatrists, psychologists, behavioral therapists and counselors.
An estimated 132 million Americans — nearly 40% of the population — live in an area with a significant shortage in these providers, leaving patients waiting months for treatment once they decide to reach out for care.
An estimated 132 million Americans — nearly 40% of the population — live in an area with a significant shortage in these providers, leaving patients waiting months for treatment once they decide to reach out for care.
One part of the solution that I have argued for in the past is to permanently waive the rules that require clinicians to be licensed in the states where patients are located.
This was allowed earlier in the pandemic, temporarily enabling providers in well-staffed states, like New Jersey and Massachusetts, to extend help in under-staffed states, such as Wyoming and Utah.
One part of the solution … is to permanently waive the rules that require clinicians to be licensed in the states where patients are located.
… we also need to provide better guidance for the consumers who will use these products.
Even as the pandemic recedes, the need for mental healthcare remains high. By opening the universe of providers to those who need them, regardless of where they’re located, patients will have an easier time accessing care quickly.
The Important Role for Digital Health Technology
The role technology can play in healthcare becomes incredibly clear against the backdrop of COVID-19, a lack of providers, and the high number of Americans suffering from both recognized and unrecognized depression.
The role technology can play in healthcare becomes incredibly clear against the backdrop of COVID-19, a lack of providers, and the high number of Americans suffering from both recognized and unrecognized depression.
The potential exists for technology to deliver personalized, clinically-validated digital assessments and therapeutics that shorten the distance between need and care and produce outcomes validated by data.
Our ability to limit suffering, improve quality of life and reduce healthcare costs is limited only by how quickly we embrace new models of care delivery without sacrificing quality.
In addition to addressing the shortage of mental health professionals by permanently waiving the rules that prohibit clinicians from delivering care via telemedicine across state lines, we also need to provide better guidance for the consumers who will use these products.
Today, there are an estimated to 20,000 mental health apps available in the App Store, but less than 2% have been validated for safety and efficacy by studies or clinical trials.
Today, there are an estimated to 20,000 mental health apps available in the App Store, but less than 2% have been validated for safety and efficacy by studies or clinical trials.
The Food and Drug Administration can’t actively regulate all of these apps, which means the entrepreneurs and investors who build them need to adhere to the rigorous scientific standards that exist to ensure patient safety.
The advancement of digital therapeutics is necessary to improve physical and mental health at scale, but they will require carefully crafted guardrails to ensure patient safety.
MURRAY ZUCKER is the
Chief Medical Director, Happify Health
About Happify Health
Happify Health is a clinical grade technology company. We shorten the distance between need and care by configuring personalized digital therapeutics and care solutions to deliver each person the care they need, when they need it, in the way they want.
Original publication
Economic Burden of the ‘Silent’ Mental Health Epidemic













