Key messages
There is a gap between early- and late-adopting hospitals and healthcare facilities when it comes to data technology
- Unlike early adopters, late adopters feel that in order to succeed with new data strategies, they need: (1) more clarity around how data is being used, and (2) greater access to data specialists and better tracking of performance metrics and KPIs.
- Investment priorities differ too Late adopters are more likely to be investing in voice recognition tools (35% vs. 20%), perhaps because many are still catching up when it comes to digital health records.
- One way of addressing these concerns could be through forging mentoring partnerships with early adopters in other hospitals and healthcare facilities.
This is an excerpt of the publication below, with the title above, focusing on the topic in question.
Philips
June, 2022
The Future Health Index is commissioned by Philips
Jan Kimpen, Philips Chief Medical Officer
Excerpt by:
Joaquim Cardoso MSc.
Health Revolution . Institute
Digital, Health and Care Revolution
June 13, 2022
4.The divide between early and late technology adopters
There is a gap between early- and late-adopting hospitals and healthcare facilities when it comes to data technology
Unlike early adopters, late adopters feel that in order to succeed with new data strategies, they need:
- more clarity around how data is being used,
- greater access to data specialists and better tracking of performance metrics and KPIs.
One way of addressing these concerns could be through forging mentoring partnerships with early adopters in other hospitals and healthcare facilities.
Unlike early adopters, late adopters feel that in order to succeed with new data strategies, they need: (1) more clarity around how data is being used, (2) greater access to data specialists and better tracking of performance metrics and KPIs.
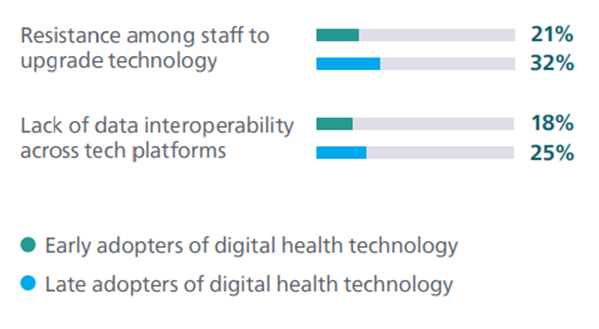
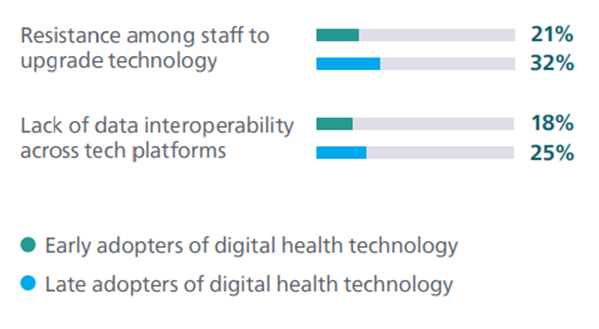
Late adopters are more likely to report having issues among staff when it comes to upgrading technology (32% vs. 21%), suggesting early adopters may have more systems in place to help their staff adjust to changes in technology.
Late adopters are also more likely to experience a lack of data interoperability across technology platforms (25% vs. 18%).
Late adopters are more likely to report having issues among staff when it comes to upgrading technology (32% vs. 21%) …
… and are also more likely to experience a lack of data interoperability across technology platforms (25% vs. 18%).
When it is difficult for late adopters to upgrade technology due to challenges with training staff, they are also less likely to resolve interoperability issues.
When it is difficult for late adopters to upgrade technology due to challenges with training staff, they are also less likely to resolve interoperability issues.
These hospitals could benefit from multifaceted solutions that help train staff for an easier transition to advanced technology, enabling them to use data more effectively.
Investment priorities differ too Late adopters are more likely to be investing in voice recognition tools (35% vs. 20%), perhaps because many are still catching up when it comes to digital health records.
Many hospitals that are still in the process of adopting digital health records rely on manual record-keeping, and therefore have a greater need to invest in voice recognition to help save time.
Many hospitals that are still in the process of adopting digital health records rely on manual record-keeping, and therefore have a greater need to invest in voice recognition to help save time.
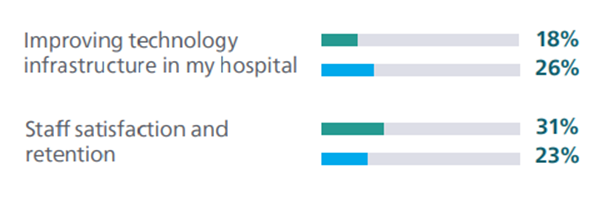
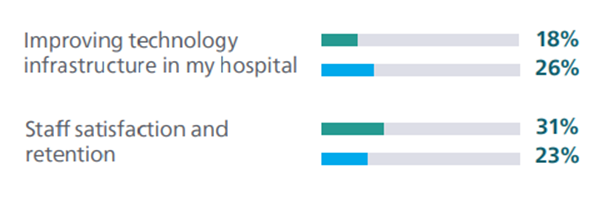
Indeed, late adopters are more likely to prioritize improving the technology infrastructure in their hospital (26% vs. 18%) and driving efficiencies in the hospital (27% vs. 20%).
On the other hand, early adopters have moved on to prioritize more recent needs in healthcare, like telehealth (27% vs. 20%) and staff satisfaction and retention (31% vs. 23%).
Late adopters are more likely to prioritize improving the technology infrastructure in their hospital (26% vs. 18%) and driving efficiencies in the hospital (27% vs. 20%).
Early adopters have moved on to prioritize more recent needs in healthcare, like telehealth (27% vs. 20%) and staff satisfaction and retention (31% vs. 23%).
Differences in current priorities between early and late adopters of digital health technology
Differences in barriers to using data between early and late adopters of digital health technology

ORIGINAL PUBLICATION (Chapter 2)

Structure of the publication
Unlocking the power of data (Chapter 2)
- Unlocking the power of data
- 1.Healthcare data proves its worth
- 2.Regardless of their rate of technology adoption, healthcare leaders still encounter data challenges
- 3.Driving data adoption across care settings
- 4.The divide between early and late technology adopters
- 5.A growing need for collaboration with peers
- 6.Leaders are keen to partner with healthcare technology companies

Unlocking the power of data
Confidence is high
Healthcare leaders are increasingly using data in both operational and clinical workflows.
Doing so helps improve efficiencies and guides swifter, more informed decision-making to help treat patients faster.
The effective use of data has become a key component for healthcare leaders as they look to tackle the organizational crises within their facilities, helping to extend and improve care.
Healthcare leaders are confident that the wealth of critical, high-quality data they have at their fingertips can unlock enormous potential.
Analyzing this information allows them to create robust healthcare strategies and unlock actionable insights that can enable new ways of predicting, diagnosing and treating diseases.
These insights in turn can help to fuel greater efficiencies while reducing treatment costs and improving the quality of care.
Healthcare leaders are confident that the wealth of critical, high-quality data they have at their fingertips can unlock enormous potential.
These insights — from the information analysis — in turn can help to fuel greater efficiencies while reducing treatment costs and improving the quality of care.
Navigating the remaining frustrations
Yet, while they acknowledge the value of data, healthcare leaders continue to experience frustrations, such as siloed data and limited infrastructure, in capturing and deploying that data effectively.
Keenly aware that they lack the internal resources to unlock the true potential of the information they have, they are looking to their peers and other partners for support, training, and knowledge sharing.
Yet, while they acknowledge the value of data, healthcare leaders continue to experience frustrations, such as siloed data and limited infrastructure, in capturing and deploying that data effectively.
The following chapter explores what healthcare leaders value in data and their current challenges to data utilization, proposes solutions to those challenges and looks at how partnerships can help.
“It’s better to prevent than to cure… there will be greater possibilities for prevention using advancements in digital [health] technology.”
Chief Medical Information Officer, Urban hospital, the Netherlands
Keenly aware that they lack the internal resources to unlock the true potential of the information they have, they are looking to their peers and other partners for support, training, and knowledge sharing.

1.Healthcare data proves its worth
Healthcare leaders are confident in the value that data can bring to their work
Data plays a crucial role in delivering healthcare, helping to drive smarter clinical decisions and encourage greater operational efficiency.
Actionable insights provide healthcare leaders with operational forecasting and clinical predictions, and enhance both the patient and staff experience.
Data plays a crucial role in delivering healthcare, helping to drive smarter clinical decisions and encourage greater operational efficiency.
Nearly two-thirds (65%) of healthcare leaders believe the value data brings in areas such as digital health records, patient monitoring and medical devices makes the time and resource investments required worthwhile.
Nearly two-thirds (65%) of healthcare leaders believe the value data brings in areas such as digital health records, patient monitoring and medical devices makes the time and resource investments required worthwhile.
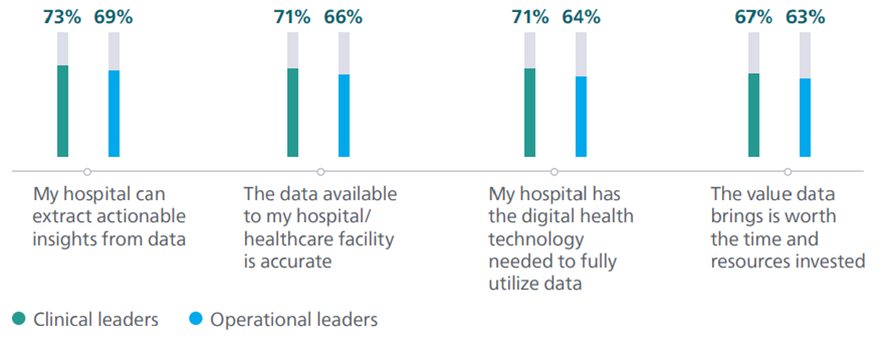
Trust in the insights provided by data is also strong across both clinical and operational settings, while confidence in data utilization is particularly high among clinical leaders, who are more likely to have a positive outlook on data than their peers who work on the operational side.
Lack of trust is among the lowest barriers to using data
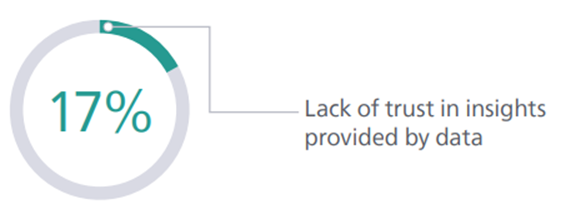
Confidence in data utilization

Clinical leaders are more likely to show confidence in data utilization than operational leaders
BOX: Mixed views from patients on data sharing
The Lancet’s 2020 study, Public perceptions on data sharing: key insights from the UK and the USA, examined public attitudes towards data sharing*, data access and the use of AI in healthcare.
Most of those questioned were happy to share their data with their doctor.
However, there was a suggestion that patients were concerned that data might not be protected from commercial end-use.
Respondents were less probable to be willing to share their details with an institution that was likely to use the data for commercial purposes (e.g. insurance company) than a public body (e.g. government, research institution).
The implication is that more needs to be done to educate, inform and reassure the public on how their health data is used.

2.Regardless of their rate of technology adoption, healthcare leaders still encounter data challenges
Despite their confidence, many leaders are frustrated about the lack of progress in embedding data throughout care pathways
Limited technology infrastructure; staff reluctance or data illiteracy; the sheer amount of data to be processed:
most of these barriers have been a constant presence for healthcare leaders since the Future Health Index research began in 2016.
Limited technology infrastructure; staff reluctance or data illiteracy; the sheer amount of data to be processed: most of these barriers have been a constant presence for healthcare leaders since the Future Health Index research began in 2016.
Top barriers to effective use of data
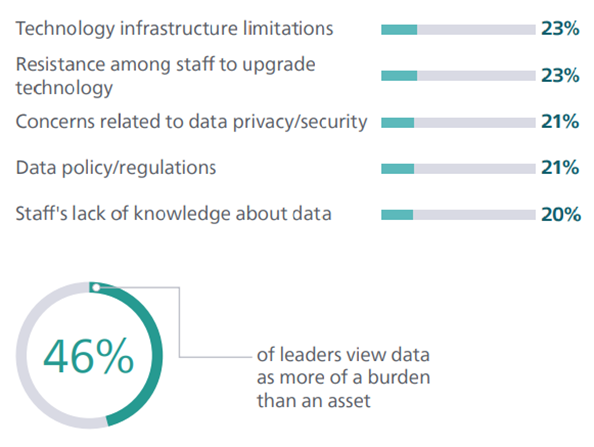
Technology infrastructure limitations
Almost one-quarter (23%) of healthcare leaders say this is the top impediment.
However, with technologies like digital health records close to the top of leaders’ investment priority lists, it is also clear that they are trying to address this.
Siloed data
Just over half (51%) of healthcare leaders say that data silos hinder their ability to utilize data effectively.
This is closely linked to the fact that 20% of healthcare leaders have difficulties managing a high volume of data and 19% have difficulties obtaining data.
Just over half (51%) of healthcare leaders say that data silos hinder their ability to utilize data effectively.
This is closely linked to the fact that 20% of healthcare leaders have difficulties managing a high volume of data and 19% have difficulties obtaining data.
Grouped with frustrations surrounding technology infrastructure and staff knowledge, leaders may struggle to resolve data access and management challenges.
Siloed data is a greater issue for healthcare leaders in small- (56%) and medium-sized (51%) hospitals (based on the number of locations), than for their peers in larger hospitals (39%).
This suggests that multi-site facilities are, by necessity, taking more action to address the issue of data silos.
Data security and policy
One in five (21%) leaders say that data policy and/ or regulations impede their ability to use data to its full potential, with the same number citing concerns about data privacy and security.
This is not surprising considering the volume and scale of reported healthcare data breaches.
Staff knowledge and mindset
Today’s healthcare leaders report inadequate staff understanding of how to use data (20%) and staff feeling overwhelmed by the volume of data (55%).
Today’s healthcare leaders report inadequate staff understanding of how to use data (20%) and staff feeling overwhelmed by the volume of data (55%).
Staff resistance to using more advanced technologies can present challenges too. Healthcare leaders see staff development as vital, with about one-fifth (22%) saying that training and educating staff would most support them in using data.
Staff resistance to using more advanced technologies can present challenges too. Healthcare leaders see staff development as vital, with about one-fifth (22%) saying that training and educating staff would most support them in using data.
With data considered the bedrock of so many digital technologies that underpin efficiencies, care outcomes and patient and staff experiences, these obstacles can impact leaders’ ability to deliver on key priorities, like expanding care and improving staff morale.
BOX: Ransomware: an invisible yet growing threat for healthcare systems
A type of malicious software designed to block access to computer systems until a sum of money is paid, ransomware attacks represent a significant risk to healthcare organizations.
The Federal Bureau of Investigation’s (FBI) 2021 Internet Crime Report[1] found that the healthcare sector faced the most ransomware attacks in 2021 compared to any other critical infrastructure sector.
A heavy reliance on technology to treat patients, coupled with the high volume of data typically held by hospitals and healthcare facilities, means they are especially vulnerable to being targeted by hackers.
Such attacks create delays in medical procedures, can lead to longer patient stays and increase patient mortality rates, as well as requiring extensive funds to resolve the impacts of the attack — …
… a ransomware attack on the Irish healthcare system in May 2021 resulted in costs of more than €100 million[2].

3.Driving data adoption across care settings
Leaders pinpoint key measures to improve adoption of data technologies
Healthcare leaders are considering several initiatives to help drive uptake of data-centric healthcare technologies, including staff training, improved tracking, and the addition of data specialists to manage and analyze data.
Healthcare leaders are considering several initiatives to help drive uptake of data-centric healthcare technologies, including staff training, improved tracking, and the addition of data specialists to manage and analyze data.
Top factors that would support healthcare leaders in fully utilizing data
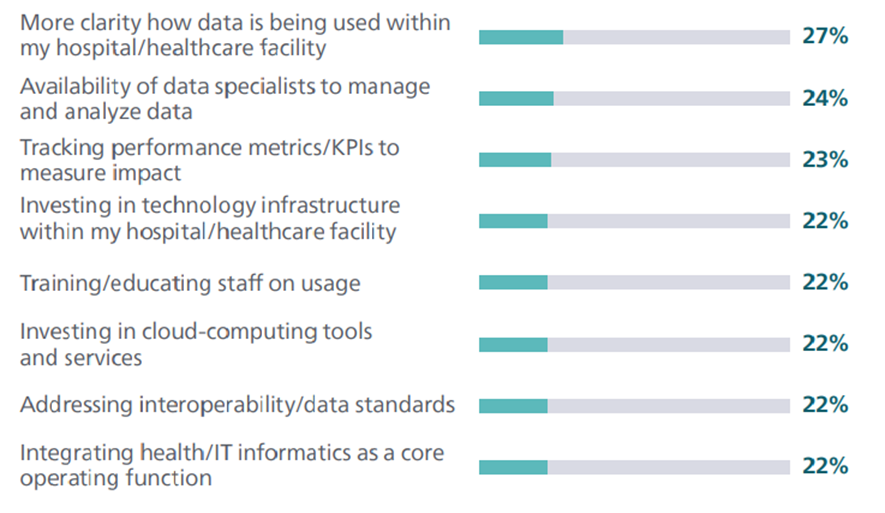
Just over one-fifth (21%) of all healthcare leaders surveyed say that implementing data security and privacy systems would be most helpful, a need that also ranked highly in the Future Health Index 2021 report.
Interestingly, despite data privacy and security being concerns for these leaders, this isn’t a significant priority for them, either today or three years from now.
Interestingly, despite data privacy and security being concerns for these leaders, this isn’t a significant priority for them, either today or three years from now.
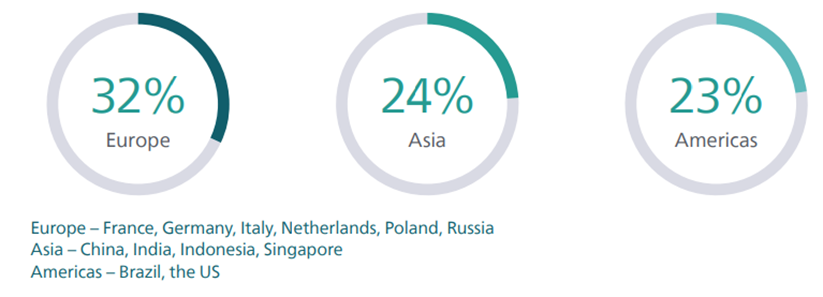
Healthcare leaders in Europe (32%) are more likely to want more clarity on how data is being used compared to those in Asia (24%) or the Americas (23%), reflecting stricter data privacy regulations in the European Union.
This is observed in the fact that healthcare leaders in the Netherlands are more likely to want clarity than their peers in most of the countries surveyed.
Healthcare leaders in Europe are most likely to seek clarity on how their data is being used

4.The divide between early and late technology adopters
There is a gap between early- and late-adopting hospitals and healthcare facilities when it comes to data technology
Unlike early adopters, late adopters feel that in order to succeed with new data strategies, they need:
- more clarity around how data is being used,
- greater access to data specialists and better tracking of performance metrics and KPIs.
One way of addressing these concerns could be through forging mentoring partnerships with early adopters in other hospitals and healthcare facilities.
Unlike early adopters, late adopters feel that in order to succeed with new data strategies, they need: (1) more clarity around how data is being used, (2) greater access to data specialists and better tracking of performance metrics and KPIs.
Late adopters are more likely to report having issues among staff when it comes to upgrading technology (32% vs. 21%), suggesting early adopters may have more systems in place to help their staff adjust to changes in technology.
Late adopters are also more likely to experience a lack of data interoperability across technology platforms (25% vs. 18%).
When it is difficult for late adopters to upgrade technology due to challenges with training staff, they are also less likely to resolve interoperability issues.
These hospitals could benefit from multifaceted solutions that help train staff for an easier transition to advanced technology, enabling them to use data more effectively.
Investment priorities differ too Late adopters are more likely to be investing in voice recognition tools (35% vs. 20%), perhaps because many are still catching up when it comes to digital health records.
Many hospitals that are still in the process of adopting digital health records rely on manual record-keeping, and therefore have a greater need to invest in voice recognition to help save time.
Many hospitals that are still in the process of adopting digital health records rely on manual record-keeping, and therefore have a greater need to invest in voice recognition to help save time.
Indeed, late adopters are more likely to prioritize improving the technology infrastructure in their hospital (26% vs. 18%) and driving efficiencies in the hospital (27% vs. 20%).
On the other hand, early adopters have moved on to prioritize more recent needs in healthcare, like telehealth (27% vs. 20%) and staff satisfaction and retention (31% vs. 23%).
Late adopters are more likely to prioritize improving the technology infrastructure in their hospital (26% vs. 18%) and driving efficiencies in the hospital (27% vs. 20%).
Early adopters have moved on to prioritize more recent needs in healthcare, like telehealth (27% vs. 20%) and staff satisfaction and retention (31% vs. 23%).
Differences in current priorities between early and late adopters of digital health technology
Differences in barriers to using data between early and late adopters of digital health technology

5.A growing need for collaboration with peers
Healthcare leaders know they can’t do it alone
In the Future Health Index 2021 report, more than one-third (41%) of healthcare leaders said they believed strategic partnerships were the best way to successfully implement digital health technologies.
Such partnerships offer rich opportunities to access skills, knowledge and expertise from technology companies.
They also enable a more bespoke approach for each hospital or healthcare system and present less risk.
More than one-third (41%) of healthcare leaders said they believed strategic partnerships were the best way to successfully implement digital health technologies.
Today, research shows the need for partnerships is even more pressing, regardless of where leaders are on their adoption journeys.
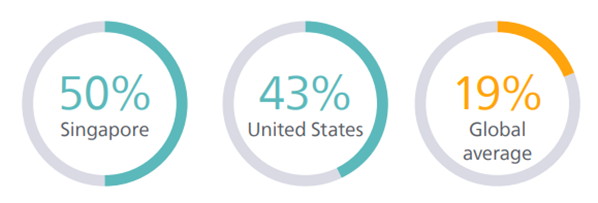
Fewer than one-fifth (19%) say they have all the expertise they need internally to make full use of the available data.
And, there are still 69% of early adopters who do not yet have all of the expertise they need to fully utilize data.
There are still 69% of early adopters who do not yet have all of the expertise they need to fully utilize data.
Learning from peers
It is clear that healthcare leaders place significant value in what they can learn from their peers, particularly in relation to data.
Over one-third (37%) today say that other hospitals and healthcare facilities would be the external partner of preference to help them fully utilize data, and more than one-quarter of healthcare leaders say that success stories from other hospitals or healthcare facilities would strengthen their trust in predictive analytics.
The COVID-19 pandemic resulted in many strong healthcare partnerships that improved the agility of — and access to — the healthcare sector.
Collaboration with hospitals and healthcare systems, once considered competitors*, demonstrated the power of partnerships in advancing patient care.
The COVID-19 pandemic resulted in many strong healthcare partnerships that improved the agility of — and access to — the healthcare sector.
Early adopters of technology are investing heavily in the right expertise today
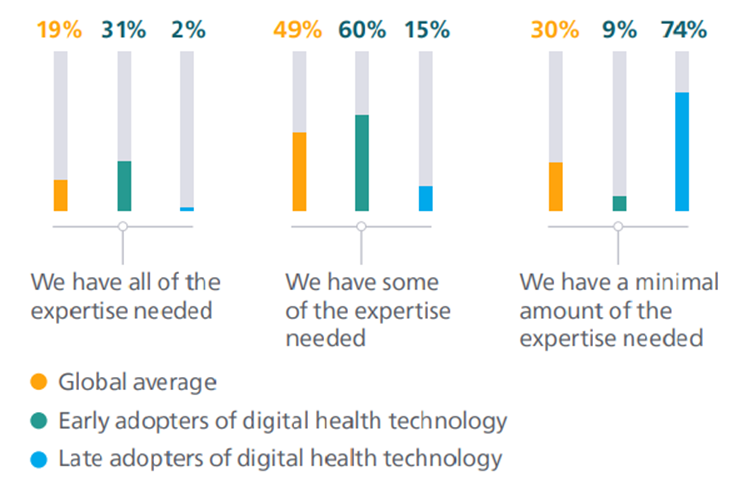
Healthcare leaders in Singapore and the United States are most likely to say they have all the internal expertise they need

6.Leaders are keen to partner with healthcare technology companies
Partnering with healthcare technology companies is seen to offer numerous benefits
Last year’s research found that 36% of healthcare leaders wanted to collaborate with health IT or informatics companies to help drive digital transformation.
This trend continues in 2022, with one-third (33%) of healthcare leaders citing health technology companies as a partner of preference.
33% of healthcare leaders want to collaborate with health IT or informatics companies to help drive digital transformation.
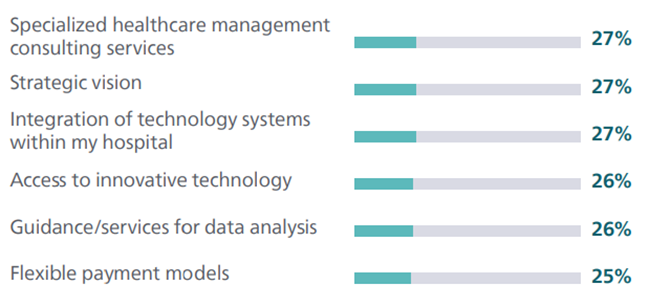
There are particular areas of knowledge that leaders want to tap into with these partnerships.
They seek extensive support from strategic partnerships with health technology companies, in areas including:
- strategic vision,
- specialized healthcare management consulting services, guidance/services for data analysis,
- access to innovative technology, and
- flexible payment models.
They seek extensive support from strategic partnerships with health technology companies, in 4 main areas ..
The varied range of areas that leaders are looking for support with implies that partnering with companies with broad healthcare expertise would be most beneficial in order to collaborate in all of these priority areas.
Unsurprisingly, they also look to health technology companies to support their staff, with over one-quarter (26%) citing staff training and education as the most important benefit from such a partnership.
… they also look to health technology companies to support their staff, with over one-quarter (26%) citing staff training and education as the most important benefit from such a partnership.
Partnership requirements also vary depending on the maturity of technology adoption.
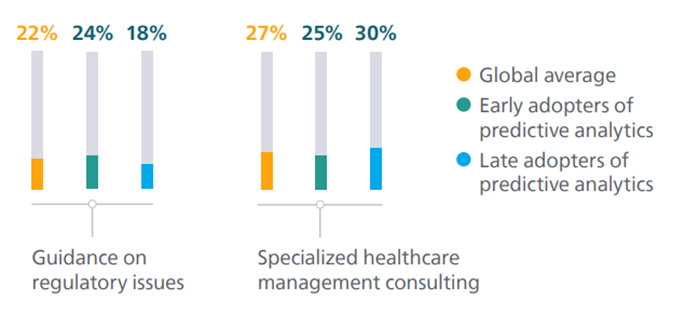
For example, healthcare leaders who are early adopters of predictive analytics are more likely to seek guidance on regulatory issues from a partnership than their late-adopting peers, who express greater preference for healthcare management consulting.
The support healthcare leaders seek from health technology companies
Differences between what early and late adopters of predictive analytics want from a partnership
References
See original publication
Originally published at https://www.philips.com












