This is a republication of the paper “The Vaccine-Hesitant Moment”, with the title above.
NEJM
Dan L. Longo, M.D., Editor,
Heidi J. Larson, Ph.D., Emmanuela Gakidou, Ph.D., and Christopher J.L. Murray, M.D., Ph.D.
June 29, 2022, yale insights
Executive Summary edited by
Joaquim Cardoso MSc.
Health Revolution Institute
Vaccines and Vaccination Unit
June 29, 2022
Overview
- Vaccine hesitancy is a state of indecision and uncertainty about vaccination before a decision is made to act (or not act). It represents a time of vulnerability and opportunity.
- Multiple surveys that were conducted to examine the sentiments concerning coronavirus disease 19 (Covid-19) vaccination have exposed new levels of volatility around vaccine hesitancy, particularly when the hesitancy is powered by digital media platforms.
- Spikes in vaccine hesitancy often coincide with new information, new policies, or newly reported vaccine risks.
- Some of the variability is due to factors such as a decline in the public’s trust of experts, preferences for alternative health, political polarization, and belief-based extremism.
- In this review, we use the examples of hesitancy regarding the measles–mumps–rubella (MMR), human papillomavirus (HPV), and Covid-19 vaccines to look at the multifaceted issues that fuel vaccine hesitancy. Each of these examples is part of a larger, complex story.
Addressing New Challenges
- Social media and other digital platforms provide the opportunity to collect data on vaccine hesitancy in nearly real time70,71; they also allow new methods of analysis72 and the opportunity to investigate the effect of vaccine sentiment on actual vaccine uptake and vaccine-preventable diseases.
- The large volume of timely data on vaccine hesitancy has provided an opportunity to develop spatially detailed estimates of vaccine hesitancy (i.e., mapping by location). For example, vaccine hesitancy ranges from 7 to 49% across ZIP codes within the rural Stearns County, Minnesota. Such widespread variation within a county is common in all U.S. states
- Spatially refined estimates of vaccine hesitancy have proved to be useful in local efforts to increase vaccination rates.75,76 The information has been used by community outreach programs to tailor their efforts to local areas that have the greatest need. Other groups have used local patterns to help to decide where to provide mobile vaccination clinics and where to initiate other measures for reducing barriers to vaccination.
- Local information can also be used to monitor the effect of local interventions, including the effect of various types of vaccination mandates.
Next steps
- In the future, large and complex data sets on vaccine hesitancy, often referred to as big data, can be analyzed according to spatial identifiers such as ZIP code and various individual characteristics, including race or ethnic group, age, sex, and occupation, which can help to further microtarget vaccination outreach efforts. This information is also potentially critical for monitoring progress toward vaccine equity.
- One of the various challenges in taking such an approach to scale and applying it globally is the inequity in the access to and reach of digital media.
- As the digital revolution unfolds globally, the global health community must keep pace.
- The consequences of not doing so are loud and clear, as we have seen in the context of the Covid-19 pandemic with regard to the rapid spread of misinformation and consequent vaccine hesitancy.
Conclusions
- Given the dynamic and changing nature of vaccine hesitancy — particularly obvious in the context of Covid-19 — keeping vaccine conversations open and ongoing will be important in order to identify and address emerging concerns early.
- Ratzan and colleagues, in an article on vaccine hesitancy, point to a “variability in stages of readiness, the fluidity of people’s views, and the persuasive power of access to health professionals embedded in the communities where people live and work.”77
- Physicians and other health care providers are still among the most trusted persons when it comes to health care advice.
- The Wellcome Global Monitor surveyed people in 140 countries and found that 73% of the respondents said that they would trust a doctor or a nurse more than others; the percentage was 90% in the higher-income countries.78
- Vaccine acceptance can increase,79,80 but health care providers need to offer support and encouragement and listen to what matters from the patient’s perspective.
- Equipping physicians with information on the nature and scope of circulating concerns in their communities may help them address such concerns in the clinic, while also informing appropriate interventions at the community level.
ORIGINAL PUBLICATION (full version)

The Vaccine-Hesitant Moment
NEJM
Dan L. Longo, M.D., Editor,
Heidi J. Larson, Ph.D., Emmanuela Gakidou, Ph.D., and Christopher J.L. Murray, M.D., Ph.D.
June 29, 2022, yale insights
Vaccine hesitancy is a state of indecision and uncertainty about vaccination before a decision is made to act (or not act).
It represents a time of vulnerability and opportunity. Multiple surveys that were conducted to examine the sentiments concerning coronavirus disease 19 (Covid-19) vaccination have exposed new levels of volatility around vaccine hesitancy, particularly when the hesitancy is powered by digital media platforms. Spikes in vaccine hesitancy often coincide with new information, new policies, or newly reported vaccine risks. Some of the variability is due to factors such as a decline in the public’s trust of experts, preferences for alternative health, political polarization, and belief-based extremism. In this review, we use the examples of hesitancy regarding the measles–mumps–rubella (MMR), human papillomavirus (HPV), and Covid-19 vaccines to look at the multifaceted issues that fuel vaccine hesitancy. Each of these examples is part of a larger, complex story.
Timing is everything when it comes to vaccine acceptance or hesitancy, …
… and the mutable nature of vaccine hesitancy calls for new modes of analysis to characterize not only the temporal features of hesitancy but also the spatial (e.g., regional) features and the many behavioral manifestations and their effects on vaccine uptake.
Such real-time data also allow investigation into contextual events that can help us understand the drivers of hesitancy. Vaccine acceptance can be increased, but responsiveness to emerging concerns is key. Given that physicians and other health care providers are still among the most trusted figures when it comes to health care advice, local information about the nature and scope of vaccine hesitancy in their communities may help them anticipate and support important conversations in the clinic.
Twelve years ago, a meeting of public health experts was convened to reflect on why there was such low uptake of the influenza A (H1N1) vaccine, …
… which was hurriedly developed in response to the pandemic alert issued by the World Health Organization (WHO).1
The title of the meeting report was “A Crisis of Public Confidence in Vaccines,” and it heralded a warning: “The lack of public confidence in vaccines risks undermining the political will necessary to rapidly respond to a more severe influenza pandemic in the future.”2
The initially feared 2009 H1N1 pandemic was not as severe as anticipated, and the early public eagerness for the H1N1 vaccine waned as the threat of the virus tapered.
By the time the H1N1 vaccines were available, few people wanted them, and some were angered at the perceived hyping of the pandemic risk.3 Ofri coined the term “emotional epidemiology” in her reflections on her patients’ roller-coaster sentiments concerning the H1N1 vaccine, from their impatience to get the vaccine to initial hesitancy and refusal.4 Even some patients who typically decided against receiving the seasonal influenza vaccine were eager for the H1N1 vaccine when the first alarm bells rang. The H1N1 vaccine is different, they told her.
Timing is everything regarding both the personal moment and the historical moment when it comes to making a decision about vaccination.
The uncertainty and constantly evolving nature of the Covid-19 pandemic and response measures, the rapid introduction of new vaccines, emerging variants, and the volatility of the surrounding politics and polarization have all contributed to public questioning and the trends in vaccine hesitancy.5–9

Defining Vaccine Hesitancy
As vaccine hesitancy became increasingly recognized as a global challenge and global immunization rates plateaued and even started to decline in some areas,10 the WHO Strategic Advisory Group of Experts (SAGE) on Immunization “noted with concern the impact of reluctance to accept immunization on the uptake of vaccines reported from both developed and developing countries.”
In 2011, SAGE established the Working Group on Vaccine Hesitancy,11 which defined vaccine hesitancy as “complex and context-specific,” “varying over time and place,” and “vaccine specific.”12 In 2019, WHO named vaccine hesitancy as one of the top 10 threats to global health.13
The definition of vaccine hesitancy, however, has not always been clear. In 2013, Dubé et al. observed that “despite the growing number of articles referring to vaccine hesitancy published in recent years, there are some discrepancies among publications about what exactly falls under the umbrella of ‘vaccine hesitancy.’”14 In 2015, Peretti-Watel and colleagues pointed to the “ambiguous notion” of vaccine hesitancy and noted that definitions of vaccine hesitancy “tend to be very broad and to embrace heterogeneous people/situations and many different explanatory factors,” and they proposed that vaccine hesitancy be considered “a kind of decision-making process.”15 In 2021, Maya Goldenberg, in her book Vaccine Hesitancy, defines it as “an attitude of ambivalence.”16
In this review, we focus on vaccine hesitancy as a state of indecision and uncertainty that precedes a decision to become (or not become) vaccinated.
Vaccine hesitancy is an attitude or sentiment, whereas vaccination is an action, which is measured to determine vaccine coverage. The period of hesitancy and indecision is a time of vulnerability, as well as opportunity. Sentiments concerning whether to undergo vaccination can change, and change again, as evidenced in multiple surveys showing that Covid-19 vaccine sentiments are influenced by factors such as a new report of vaccine risks or perceptions of increasing or decreasing disease threats.17,18
The State of Things
Vaccine hesitancy is not a new issue, but it has escalated in scope and scale.
The high degree of vaccine questioning and reluctance to accept vaccination is amplified by social media platforms. In addition, the introduction of new vaccines and combinations of vaccines19 prompts new questions and consequent searching for information in a landscape of confusing misinformation and disinformation alongside accurate, scientifically based information. As Davies and colleagues note in one of the early studies on the role of the Internet in propagating negative vaccine sentiments, “The antivaccination message on the internet is far more unbridled than in other media…. The internet represents a greater potential for the public to make uninformed decisions about vaccination.”20
Some of these changes are due to contextual factors, including a wider decline in trust of expertise and authority, and different modes of belief-based extremism.21
Political polarization, as well as libertarian views and alternative health care advocacy, triggers public questioning about the importance, safety, and effectiveness of vaccines.22 In addition, the hyperconnected digital landscape offers a new opportunity for people with shared beliefs to self-organize across geographic regions, influencing and sometimes disrupting public confidence and cooperation. As Kata notes, in transitioning from the notion of antivaccine messages to the recognition of a more widespread movement, “many people search online for health information, and the information found impacts patient decision-making; it is therefore essential to understand what is shared online.… The anti-vaccination movement has taken advantage of this milieu to disseminate its messages.”23
Some vaccine hesitancy is tied to a specific vaccine, …
… such as hesitancy based on the now-debunked yet persistent belief that the MMR vaccine could cause autism24,25 or the possible link between hepatitis B vaccination and multiple sclerosis, which caused anxiety in France and has also been repeatedly disproved.26
Vaccine hesitancy can also be triggered by anxiety about the administration of vaccines, including fear of needles,27 or by concern about possible side effects (e.g., concern on the part of adolescent girls who are anxious about potential reactions to HPV vaccination28–30), including those associated with the new Covid-19 vaccines.31
Other concerns are related to vaccine ingredients, such as thimerosal, which is used as a preservative, or adjuvants that boost the effectiveness of vaccines.32 Parents may contest the childhood immunization schedule, claiming “too many, too soon,” or express concern that the schedule overwhelms the child’s immune system; some parents may seek bespoke schedules for their children, which could make them more vulnerable to infectious diseases.33
Faced with a growing number of questions and trying to navigate evolving information about multiple new vaccines, even some health care professionals have reported feeling hesitant about accepting or recommending some vaccines.34–37
New vaccines, new vaccine policies, and newly reported research about a vaccine typically prompt questions, as do population-wide vaccine campaigns, such as the campaigns to eradicate poliomyelitis and to control the 2009 H1N1 and the Covid-19 pandemics.
A literature review on vaccine hesitancy showed that the number of articles on adolescent and adult vaccines increased from 2007 to 2012, with publications on the HPV vaccine (approved in 2006) and the influenza vaccines (largely those developed in response to the H1N1 pandemic) tripling over the study period.38,39
Similarly, the current surge in publications on Covid-19 vaccine hesitancy reflects widespread public attention to the pandemic and new Covid-19 vaccines.6,40–43
The importance of context and the public’s appetite for focusing on a particular vaccine issue are key factors that determine how much traction, and how big a response, any particular issue gets and, consequently, how much hesitancy it generates.
As Sturgis and colleagues point out in their article on social consensus and vaccine confidence, “While scholarly attention to date has focused almost entirely on individual-level drivers of vaccine confidence,… macro-level factors play an important role in understanding individual propensity to be confident about vaccination.”44

MMR, HPV, and Covid-19 Vaccine Hesitancy
Although many observers point to the 1998 Lancet article by Wakefield et al. (retracted in 2010) as the source of parental fears that MMR vaccination might cause autism, the search for what could be causing the seeming increase in autism was already brewing.
In the United States, however, anxieties were more focused on thimerosal in vaccines as a possible cause of autism.45
The attention to thimerosal emerged in the context of a larger global movement that highlighted concern about mercury in food and drugs and in the environment.
In 1999, as part of a review of mercury-related ingredients in all food and drugs, the Food and Drug Administration called for an assessment of thimerosal in childhood vaccines, although the small amount of thimerosal used in vaccines contains only a minute amount of ethylmercury and does not contain any methylmercury (the more dangerous type of mercury), which was the prime focus of the larger review.46
The U.S. Public Health Service and the American Academy of Pediatrics followed with a recommendation to remove thimerosal from childhood vaccines as a precautionary measure.47
Even though the recommendation was precautionary, with no evidence of harm, it reinforced public concern and prompted an initial 38% decrease in the hospitals that offered hepatitis B vaccination with thimerosal-containing vaccines for infants.48
Figure 1.
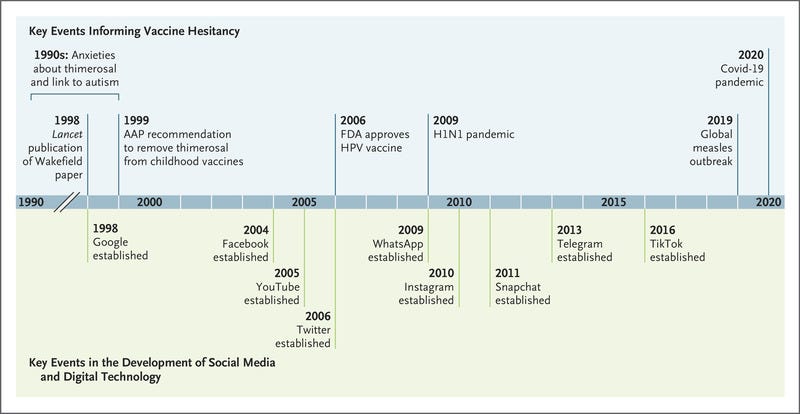
Timeline of Key Events Prompting Vaccine Hesitancy and Milestones in the Expansion of Social Media and Digital Technology.
To address the growing concerns, the Institute of Medicine conducted a major review of studies investigating links between vaccines and autism and concluded that neither MMR vaccines (which do not contain thimerosal) nor thimerosal-containing vaccines could cause autism.49
Meanwhile, some attention was shifted to the possibility that the increased number of vaccines given to children could be a cause of autism, a concern that is also not supported by any evidence. Nonetheless, the parental concerns have persisted. One study showed 70 additional MMR vaccine–related injury claims per month in the United States after publication of the report by Wakefield et al.50 Other research pointed to the effect of concern about a link between the MMR vaccine and autism on vaccine hesitancy in Somali immigrant communities in Norway and the United States.51 In 2012, a court ruling in Italy granted compensation for vaccine-related injury on the basis of the report by Wakefield and colleagues, which further amplified public anxiety. Having lost his credentials as a general practitioner in the United Kingdom, Wakefield became an activist, appealing to concerned parents and reinforcing their vaccine anxieties, alongside environmental lawyer turned vaccine critic Robert F. Kennedy, Jr., whose previous work on the toxic effects of mercury in the environment provided fertile ground for his campaign against thimerosal and vaccine safety risks more broadly. The launch of Google in 1998, followed by a cascade of new Internet-based and social media technologies, allowed widespread access to information, as well as misinformation, and fueled the viral spread of questioning about vaccines (Figure 1).52
A study in Italy investigated YouTube video content between 2007 and 2017 that focused on the suspected link between the MMR vaccine and autism.53,54
In addition to an escalation in the amount of negative content over the 10-year study period, partly reflecting the growth of YouTube after its 2005 launch, the study showed that negative videos about the MMR vaccine outnumbered positive ones by a factor of 3, with the negative videos more widely viewed. Another Italian study of vaccine-related content on YouTube had similar findings. A number of studies investigating HPV vaccine content on YouTube also showed that negative videos attracted a larger following than positive ones.55–57
Concern about one vaccine can also prompt questioning and hesitancy regarding other vaccines, such as the reported risks associated with a dengue vaccine (Dengvaxia) in the Philippines that contributed to a drop in measles vaccination58 and an HPV vaccine scare in Denmark that triggered a decline in MMR vaccine uptake. After HPV vaccine uptake declined (from 95% to just over 30%) after negative media reports, two-dose MMR vaccine coverage also dropped, from 86% to 80% among girls and from 85% to 79% among boys.59
The negative media reports that sparked HPV vaccine hesitancy and refusal in Denmark were part of a global trail of episodes of reported symptoms after HPV vaccination, from dizziness to fainting and fatigue, which the WHO now characterizes as “Immunization Stress-Related Responses.”60
One episode occurred in Japan in 2013, with related events in 2014 sparking HPV vaccine hesitancy in Denmark, Ireland, and Colombia.61
The reactions in Japan provoked a Twitter-enabled anti–HPV vaccine movement led by mothers of the affected girls, prompting the government to suspend its active recommendation of the HPV vaccine in 2013.
The suspension lasted for nearly 9 years, with reenactment of the active recommendation in April 2022.62
The story of Japan’s sustained suspension traveled around the world through news outlets and social media,63 prompting a viral global spread of HPV vaccine hesitancy.
In a 2020 modeling study, the missed opportunities and hesitancy regarding vaccination between 2013 and 2019 were predicted to result in more than 25,000 cases of preventable cervical cancer and between 5000 and 5700 deaths from cervical cancer.64
The role of social media in fueling the spread of vaccine hesitancy and its increasingly documented health consequences cannot be overstated, and vaccine hesitancy has escalated over the past decade, reaching new levels in the context of the Covid-19 pandemic.65–67
At the 2020 Munich Security Conference, WHO Director-General Tedros Adhanom Ghebreyesus called attention to the fact that alongside efforts to control the spread of Covid-19, we were faced with a challenging “infodemic” to control.68
Given the dramatic changes in the communication landscape that fuel the rapid spread of vaccine information alongside misinformation, new methodologies are needed to monitor emerging vaccine concerns over time and place in order to better inform appropriate responses.69
Mapping vaccine hesitancy at a local level is one important step toward addressing it, along with other needed interventions at the individual and community levels.
Given the dramatic changes in the communication landscape that fuel the rapid spread of vaccine information alongside misinformation, new methodologies are needed to monitor emerging vaccine concerns over time and place in order to better inform appropriate responses

Addressing New Challenges
Social media and other digital platforms provide the opportunity to collect data on vaccine hesitancy in nearly real time70,71; they also allow new methods of analysis72 and the opportunity to investigate the effect of vaccine sentiment on actual vaccine uptake and vaccine-preventable diseases.
Facebook collaborated with Carnegie Mellon University and the University of Maryland to collect survey data on a wide variety of behaviors related to the Covid-19 pandemic.73
Starting in January 2021, Facebook users who agreed to participate in the survey were asked about their attitudes toward Covid-19 vaccines and reasons underlying vaccine hesitancy.
Although data collected on social media platforms, such as Facebook, Twitter, and YouTube, may not be representative, since the users of the platform are not a random sample of the population, the data have aligned well with other, less frequently compiled survey data that are available for select topics and populations.
In addition, sometimes data collected through online platforms are the only available information about vaccine hesitancy (e.g., when large-scale surveys have not been conducted).
Furthermore, the large samples and the speed with which data are collected and made available make real-time analysis possible for what has become a volatile topic.
As data collected through social media platforms become more widely used, we anticipate that validation studies will be conducted, with improvements made in the sampling, weighting, and interpretation of the data.
Figure 2.
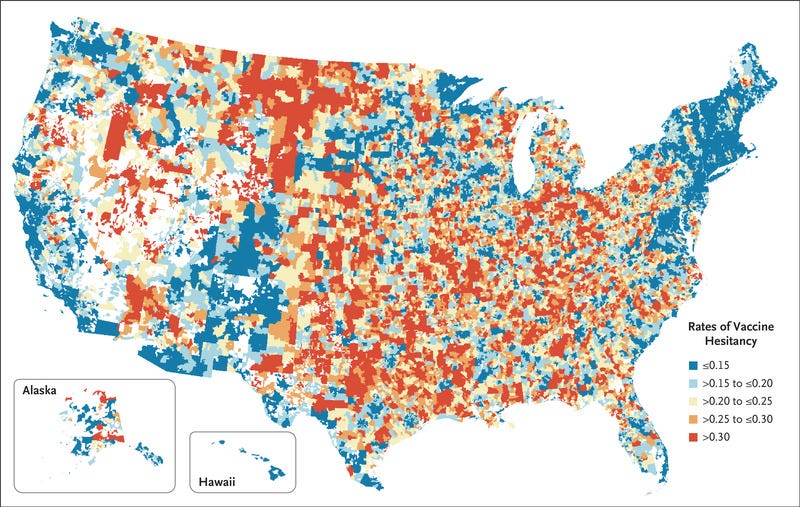
Rates of Vaccine Hesitancy across U.S. ZIP Codes, December 2021.
The large volume of timely data on vaccine hesitancy has provided an opportunity to develop spatially detailed estimates of vaccine hesitancy (i.e., mapping by location).
For the United States, surveys administered through Facebook have been used to estimate vaccine hesitancy according to week and ZIP code.
These spatial analyses show that vaccine hesitancy varies substantially within a county.
For example, vaccine hesitancy ranges from 7 to 49% across ZIP codes within the rural Stearns County, Minnesota. Such widespread variation within a county is common in all U.S. states (Figure 2).
Spatially refined estimates of vaccine hesitancy have proved to be useful in local efforts to increase vaccination rates.75,76
The information has been used by community outreach programs to tailor their efforts to local areas that have the greatest need.
Other groups have used local patterns to help to decide where to provide mobile vaccination clinics and where to initiate other measures for reducing barriers to vaccination.
Local information can also be used to monitor the effect of local interventions, including the effect of various types of vaccination mandates.
In the future, large and complex data sets on vaccine hesitancy, often referred to as big data, can be analyzed according to spatial identifiers such as ZIP code and various individual characteristics, …
… including race or ethnic group, age, sex, and occupation, which can help to further microtarget vaccination outreach efforts.
This information is also potentially critical for monitoring progress toward vaccine equity.
One of the various challenges in taking such an approach to scale and applying it globally is the inequity in the access to and reach of digital media.
As the digital revolution unfolds globally, the global health community must keep pace.
The consequences of not doing so are loud and clear, as we have seen in the context of the Covid-19 pandemic with regard to the rapid spread of misinformation and consequent vaccine hesitancy.

Conclusions
Given the dynamic and changing nature of vaccine hesitancy — particularly obvious in the context of Covid-19 — keeping vaccine conversations open and ongoing will be important in order to identify and address emerging concerns early.
Ratzan and colleagues, in an article on vaccine hesitancy, point to a “variability in stages of readiness, the fluidity of people’s views, and the persuasive power of access to health professionals embedded in the communities where people live and work.”77
Physicians and other health care providers are still among the most trusted persons when it comes to health care advice.
The Wellcome Global Monitor surveyed people in 140 countries and found that 73% of the respondents said that they would trust a doctor or a nurse more than others; the percentage was 90% in the higher-income countries.78
Vaccine acceptance can increase,79,80 but health care providers need to offer support and encouragement and listen to what matters from the patient’s perspective.
Equipping physicians with information on the nature and scope of circulating concerns in their communities may help them address such concerns in the clinic, while also informing appropriate interventions at the community level.
References and additional information
See the original publication.
Originally published at https://www.nejm.org.