This is a republication of the paper “Finding the future of care provision: The role of smart hospitals”, published by “Bo Chen, Axel Baur, Marek Stepniak, and Jin Wang”, with the title above. The title above was given by the Editor of this site.

FULL VERSION

Finding the future of care provision: The role of smart hospitals
Finding the future of care provision: The role of smart hospitals
institute for
continuous health transformation (CHT)
Joaquim Cardoso MSc
Senior Advisor for
Continuous Health Transformation
and Digital Health
January 11, 2023
EXECUTIVE SUMMARY
Technological enablement, digitization, and automation are affecting industries today in profound ways. Healthcare delivery is no exception.
On the supply side, a host of new technologies can now be integrated into care delivery:
- Artificial intelligence (AI), robotics, precision medicine, 3-D printing, augmented reality/virtual reality, genomics, telemedicine, and more.
- Adoption of these technologies is being driven by both immediate needs (e.g., cost control and efficiency optimization) and longer-term goals (especially greater precision, fewer errors, and better outcomes).
On the demand side, new technologies have altered consumer expectations.
- An increasing number of today’s patients want healthcare services to be delivered with greater efficiency and in convenient, comfortable, near-normal settings.
As a result, the whole paradigm of care delivery is changing, and the changes will likely accelerate in the years ahead.
It is against this backdrop that hospitals, traditionally the center of healthcare delivery systems, are seeking-or being forced-to redefine themselves.
In many parts of the world, whole cities are being redesigned with “smart” features that take full advantage of new technologies.
- Typically, these cities include future-ready smart hospitals.
- These hospitals embed new technologies into their design and operations to improve the customer experience, as well as outcomes and costs.
- The technologies are used not only to improve care delivery within a smart hospital itself, but also to connect the hospital to a wider healthcare delivery ecosystem, one in which hospitals play an important but less central role.
In some cases, smart hospitals are being created in less technologically advanced cities, surpassing the general rate of infrastructure development there.
Most hospitals, however, are only beginning to take advantage of the technologies and must find ways to incorporate them into care delivery if they are to meet the challenges ahead.
The business case for smart hospitals is already very strong.
- Our experience suggests that in most OECD countries, implementing digital technologies in healthcare delivery could help realize cost savings of more than ten percent of overall annual national healthcare expenditures.
- Investors have recognized the opportunity-venture capital funding for digital health solutions has increased exponentially, from about US $1 billion in 2011 to more than US $8 billion in 2018.
… in most OECD countries, implementing digital technologies in healthcare delivery could help realize cost savings of more than ten percent of overall annual national healthcare expenditures.
The implications and imperatives for hospital investors and operators are clear.
- Greenfield hospitals should be built based on a fundamentally new, futuristic, and nimble design, one that will allow the hospital to stay agile and relevant for at least the next 20 to 30 years.
- For existing hospitals, doing nothing is not an option.
- They need to integrate new technologies in a phased manner, redesign how they are delivering acute care, rethink how they interact with other healthcare providers, and divest activities that can be outsourced to others who can perform them more efficiently or effectively.
Greenfield hospitals should be built based on a fundamentally new, futuristic, and nimble design, one that will allow the hospital to stay agile and relevant for at least the next 20 to 30 years.
In this paper
- The authors analyze the factors encouraging the development of smart hospitals, define the core characteristics of future-ready smart hospitals, …
- … and discuss their implications for hospital investors and operators.
BOX: WHERE SMART HOSPITALS STAND TODAY
At present, the United States leads in the adoption of smart hospital technologies.
Over 30 percent of US hospitals have been ranked at HIMSS EMRAM1 stage six or above, indicating that they are using electronic health record systems in a sophisticated way.
In most other regions, less than five percent of hospitals have that ranking.
Even in the United States, however, the value of these investments in smart technologies has not yet been fully realized — complimentary changes among the hospital staff and consumers are needed before the systems are fully effective.
The Asia–Pacific region is quickly catching up, however, given the number of new hospitals being built and the investments in technology being made.
Singapore, for instance, has invested significant sums to digitally enable and integrate its entire healthcare ecosystem, including its hospitals.
Through a specialized agency called Integrated Health Information Systems, the Singapore Ministry of Health has rolled out a range of digital initiatives, platforms, and apps to improve the reach, quality, and value of care delivery.
China has published policies to encourage “internet plus” in healthcare (e.g., provide telemedicine service to patients in rural areas), …
… as well as the use of advanced analytics, to address critical issues within the country’s health system.
In March 2019, the National Health Commission of China announced a new grading system to set the standards for and guide the development of smart hospitals.
Japan recently announced that it will build ten new hospitals designed around artificial intelligence within the next five years to address the physician shortage there.
Outline of the publication
Five key trends are reshaping healthcare systems globally and encouraging the transition to smart hospitals:
- 1.Shift from disease treatment to health management
- 2.Quest for clinical outcomes and quality
- 3.“Retailization” of health services (the movement to outpatient settings)
- 4.The rise of informed patients
- 5.The new focus on value and accountability.
Five features define current and future smart hospitals:
- 1.Smart hospitals are digitally connected with the rest of the ecosystem
- 2.Smart hospitals have a high degree of automation
- 3.Smart hospitals are patient-centric and offer a better patient experience
- 4.Smart hospitals are driven by analytics and big data
- 5.Smart hospitals are holistic, interdisciplinary innovators.
Implications for hospital investors and operators
Smart hospitals require smart healthcare ecosystems, and those ecosystems cannot exist in the absence of a sophisticated IT system capable of letting all entities share information.
A few private-sector healthcare organizations have been able to develop such systems on their own.
In many cases, however, governmental support is likely to be required.
In summary, the smart hospitals of the future will look very different from the hospitals of today and the past.
- Smart hospitals will operate in an environment of decentralized care provision and will no longer serve as the predominant (or in some countries, sole) provider of all healthcare interventions.
- Smart hospitals will focus instead on a core set of in-house services and connect with a broader ecosystem for delivery of other care services in an agile and efficient manner.
- In smart hospitals, digitally enabled clinical staff will be able to deliver better outcomes and a more integrated patient experience, and continuously innovate in care delivery.
INFOGRAPHIC
DEEP DIVE

Finding the future of care provision: The role of smart hospitals
MHI
By Bo Chen, Axel Baur, Marek Stepniak, and Jin Wang
May 31, 2019
Trends driving smart hospitals
Five key trends are reshaping healthcare systems globally and encouraging the transition to smart hospitals:
- 1.Shift from disease treatment to health management
- 2.Quest for clinical outcomes and quality
- 3.“Retailization” of health services (the movement to outpatient settings)
- 4.The rise of informed patients
- 5.The new focus on value and accountability.
1.Shift from disease treatment to health management.
A major change in recent years is the shift in focus from disease treatment to health management, a term that encompasses wellness, healthy living, disease prevention, and rehabilitation.
The change is being driven both by patients, who want longer, healthier lives, and by payers, which are facing budgetary pressures (and, in some cases, financial losses).
The shift to health management is occurring in many countries around the world.
For instance, the Singapore government has established an organization called the Health Promotion Board that encourages residents to adopt healthy living habits through dissemination of evidence-based information and disease prevention programs at homes, workplaces, and schools.
All residents in Singapore are urged to pay attention to their diet, exercise regularly, and undergo preventive screening, all of which helps reduce the likelihood of disease development (or progression) and need for hospital care.
The Health Promotion Board also places greater focus on the nonhospital segments of the overall patient care pathway-and gives residents a tangible push to stay out of, and get out of, hospitals.

2.Quest for clinical outcomes and quality.
Shocking as it may sound, diagnostic and treatment errors are common in healthcare.
Research in the United States, for instance, has shown that five percent of outpatient diagnoses are incorrect, diagnostic errors contribute to about ten percent of patient deaths, and approximately 20 percent of orthopedic surgeons will conduct a wrong-site surgery at some point in their career.
News reports in developing countries suggest that the misdiagnosis rates there could be even higher.
The World Health Organization estimates that even in developed countries, seven out of every 100 hospitalized patients develop a healthcare-related infection each year.
In the United States alone, more than US $210 billion is wasted annually on “unnecessary services.”
These statistics make it clear that the concept of hospitals as the major site of care delivery needs fundamental transformation to improve the quality of care.
AI, robotics, and other new technologies can improve treatment precision and dramatically decrease the probability of error.
…the concept of hospitals as the major site of care delivery needs fundamental transformation to improve the quality of care.
AI, robotics, and other new technologies can improve treatment precision and dramatically decrease the probability of error.

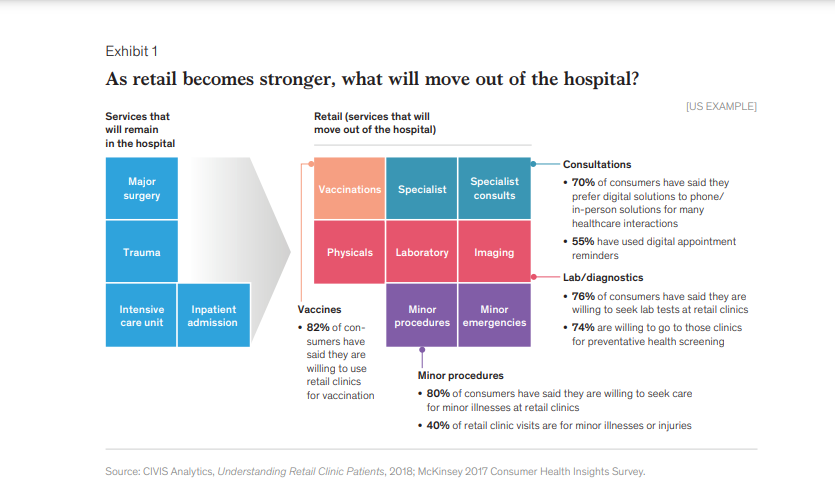
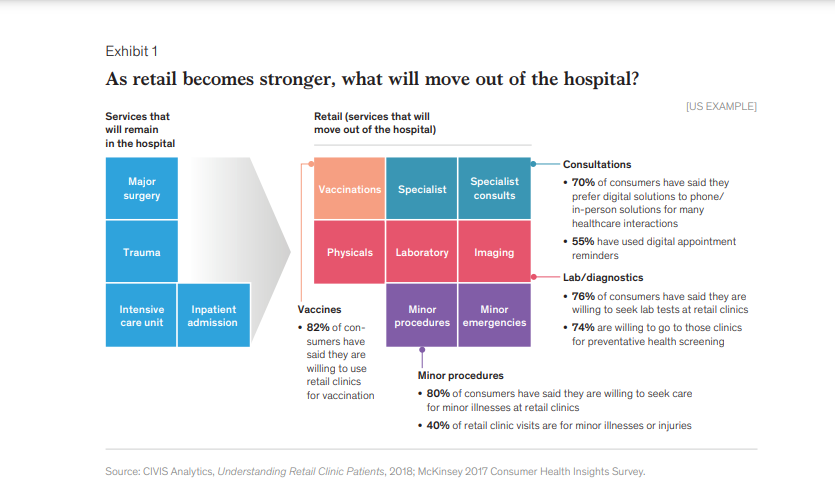
3.“Retailization” of health services (the movement to outpatient settings).
The old model of hospitals as stand-alone facilities that provide all services to all people is disappearing rapidly.
Increasingly, hospitals are becoming just one component of larger, interdependent ecosystems that include multiple other facilities (e.g., primary care providers, clinics, pharmacies, rehabilitation centers).
Already, many types of care are being shifted out of hospitals (Exhibit 1).
Increasingly, hospitals are becoming just one component of larger, interdependent ecosystems that include multiple other facilities (e.g., primary care providers, clinics, pharmacies, rehabilitation centers).
Already, many types of care are being shifted out of hospitals
In the United States, for instance, some leading retail companies offer patients a number of routine tests and treatments through clinics located within retail stores.
In China, medical resources have traditionally been concentrated in tertiary hospitals, but the government is now shifting the focus toward primary care through a massive effort to build a family physician network and community clinics.
In China, medical resources have traditionally been concentrated in tertiary hospitals, but the government is now shifting the focus toward primary care through a massive effort to build a family physician network and community clinics.
New technologies are a key component of the move toward outpatient care, since they make it possible to establish strong integration among the various entities, which improves quality of care.
4.The rise of informed patients.
Around the world, many patients are becoming more informed about, and more empowered to make, healthcare decisions.
In some countries, rising education and literacy levels are fueling this change; almost everywhere, increased internet access and the growing use of digital devices have fundamentally altered the information available to patients.
As a result, many providers see an opportunity to become more patient-centric.
Instead of passively receiving treatment, patients now often ask for more information and expect to be involved when treatment choices are made.
Often, decisions about hospitalization are made jointly by the patient and provider.
Patients can make clear whether they want, and can afford, to be hospitalized, and whether they would prefer to pursue alternative treatments.
New technologies that make possible online consultations, multidisciplinary team support, and other new models of care delivery are helping hospitals become more patient-centric.

5.The new focus on value and accountability.
The rising cost of healthcare has been a major concern in most countries. For the past decade, the United States has spent more than 17 percent of its GDP on healthcare each year.
Even in a country like China, which spends about six percent of its GDP on healthcare, costs have been rising year over year, and as a result many provinces and cities are facing growing deficits.
Payment reforms that focus on value and introduce greater risk-sharing between payers and providers are being tested in a range of health systems.
For instance, episodes of care have been introduced in the United States; diagnosis-related group (DRG) schemes are being rolled out nationwide in China.
Payment reforms that focus on value and introduce greater risk-sharing between payers and providers are being tested in a range of health systems.
Our research suggests that digital interventions that support connected electronic health records (EHRs), hospital automation, care coordination, and primary prevention can help support payment reforms and deliver considerable savings.
… digital interventions that support connected electronic health records (EHRs), hospital automation, care coordination, and primary prevention can help support payment reforms and deliver considerable savings.
Furthermore, the value creation potential is probably higher in developing markets than mature markets, since the digital devices would make it possible for hospitals in developing markets to leapfrog over older forms of care delivery.
Furthermore, the value creation potential is probably higher in developing markets than mature markets, since the digital devices would make it possible for hospitals in developing markets to leapfrog over older forms of care delivery.

The look and feel of smart hospitals
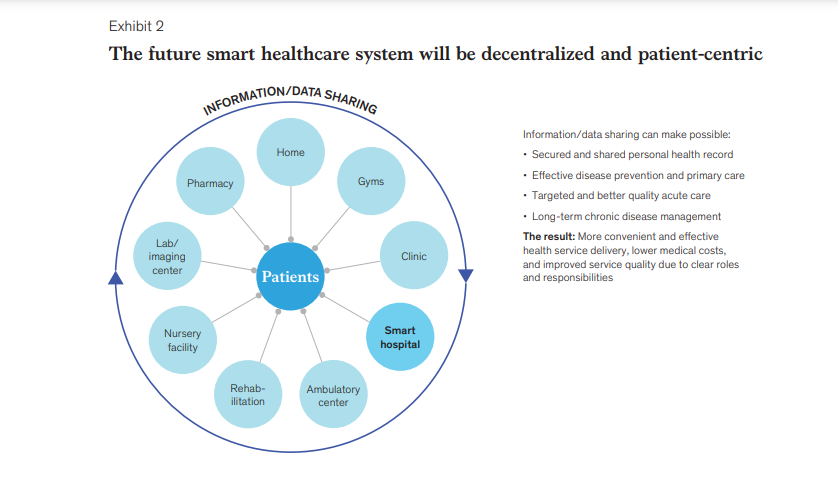
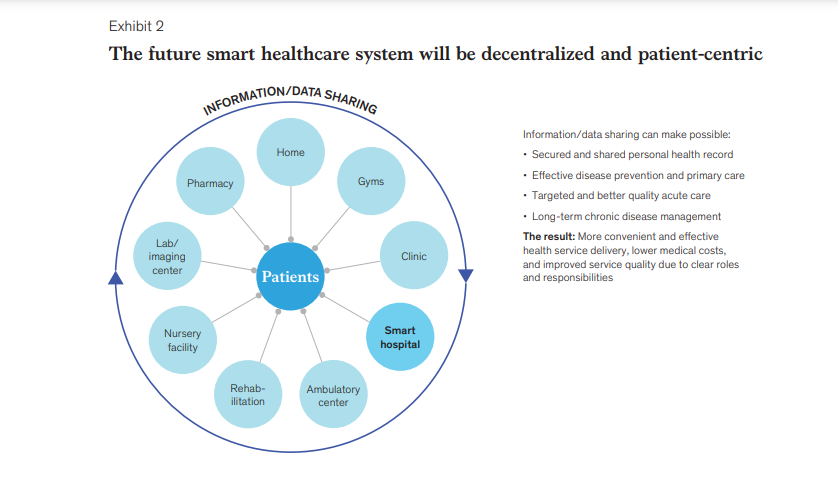
Smart hospitals do not attempt to deliver all services under one roof; …
… rather, they deliver a narrower set of high-value services within a broader ecosystem of entities, many of which have not traditionally been associated with healthcare delivery (Exhibit 2).
- In such an ecosystem, preventive services and healthcare management programs, for instance, are delivered at clinics, at gyms, and even in patients’ homes.
- Other medical treatments and minor procedures are provided at ambulatory centers.
- Diagnostic testing (imaging and laboratory services) is offered at independent centers.
- Hospitals are responsible only for major surgeries, intensive care, the management of severe trauma, and treatment for other acute, severe, complicated conditions.
Smart hospitals do not attempt to deliver all services under one roof; …
… rather, they deliver a narrower set of high-value services within a broader ecosystem of entities, many of which have not traditionally been associated with healthcare delivery
Five features define current and future smart hospitals:
- 1.Smart hospitals are digitally connected with the rest of the ecosystem
- 2.Smart hospitals have a high degree of automation
- 3.Smart hospitals are patient-centric and offer a better patient experience
- 4.Smart hospitals are driven by analytics and big data
- 5.Smart hospitals are holistic, interdisciplinary innovators.
1.Smart hospitals are digitally connected with the rest of the ecosystem.
Smart hospitals are part of an integrated, interconnected ecosystem that include government data platforms, population health agencies, and payers, as well as other providers.
Data sharing among all entities (to the extent permissible by law, balanced against the need to protect patient privacy) is crucial if the ecosystem is to ensure that patients receive high-quality healthcare efficiently and conveniently.
Smart hospitals are part of an integrated, interconnected ecosystem that include government data platforms, population health agencies, and payers, as well as other providers.
Here are a few examples of how such an ecosystem could work:
- Personal health records are collected from primary care providers and independent service centers. These records serve as the foundation for the information system. Data from hospital EHR systems is added to the personal health records.
- The information system enables real-time data sharing and connectivity between the hospital and other players. If legally permissible, health data can be further integrated with claims and payment data (from payers) and even data about health behaviors (from government agencies and technology companies).
- To ensure data connectivity, all entities (including hospitals) must agree on the standard and structure of submitted information, as well as the rules for data collection, storage, transmission, usage, etc. The rules should be designed to ensure that the data is used appropriately and kept secured so that patient privacy is protected.
- Within hospitals, patients and the staff engaged in direct patient care use interactive equipment (e.g., wearables) to enable real-time data collection, tracking, and transmission. In addition, clinical staff members are able to access the data through mobile devices to allow for more efficient clinical operations. Sydney Adventist Hospital in Australia, for instance, has transformed itself into a digital hospital with its own electronic medical record system, virtualized data centers that collect and centralize information, and mobile apps that allow the clinical staff and patients to access data within seconds.
- In some health systems, smart hospitals are the information aggregators, responsible for integrating data, storing it, and making it accessible to others (again, to the extent permissible by law). In other systems, payers or government agencies are serving as data aggregators; the smart hospitals in those systems are able to track the full continuum of care patients receive across all care settings. Connectivity is crucial because the hospitals must understand what happened before hospital admission, manage all inpatient care, and oversee post-discharge interventions.

2.Smart hospitals have a high degree of automation.
Traditionally, hospital care has been very labor intensive.
Smart hospitals rely much more heavily on a range of devices to upgrade operations and automate workflows, which significantly boosts the overall productivity and accuracy of hospital care.
Smart hospitals rely much more heavily on a range of devices to upgrade operations and automate workflows, which significantly boosts the overall productivity and accuracy of hospital care.
For instance:
- Radiofrequency identification (RFID), bar codes, and other new sensing technologies are used to optimize internal asset management and ensure that all people and materials can be identified, tracked, and traced in real time.
- Automated procedures and devices replace certain human activities in a range of care settings, freeing up the staff to spend more time on direct patient care. Automation is also used to improve the efficiency of many back-office and front-office processes.
- Web-based tracking of all patient services, electronic capacity allocation, and digital patient record management further improve the efficiency of hospital operations.
Leading hospitals in many parts of the world are already demonstrating what automation can accomplish.
Humber River Hospital in Canada, for instance, is using robots and other digital technologies to allow the clinical staff to spend more time with patients, introduce other improvements in clinical care, and automate almost 80 percent of its back-of-the-hospital services, such as pharmacy, laundry, and food delivery.
The result has been huge productivity gains and higher-quality care delivery.
Humber River Hospital in Canada, for instance, is using robots and other digital technologies to allow the clinical staff to spend more time with patients, introduce other improvements in clinical care, and automate almost 80 percent of its back-of-the-hospital services, such as pharmacy, laundry, and food delivery.

3.Smart hospitals are patient-centric and offer a better patient experience.
New healthcare technologies are being introduced to reinforce patient-centricity and improve patient satisfaction (Exhibit 3).
Indeed, the emergence of smart technologies could enhance the patient experience before, during, and after a hospital stay.
A few examples bring this to life:
- Before treatment, a patient can use wearables or remote-sensing devices to detect and record blood pressure in real time. The devices send automated warnings to the patient when they detect something unusual; the patient can then upload the blood pressure data and communicate with online staff, who can help the patient identify an appropriate specialist and confirm an appointment.
- Upon arrival at the hospital, the patient can verify his/her identity with an ID card, fingerprint, or facial recognition. The IT system greets the patient and performs automated triage, noting in the record the type of insurance the patient has. The system then explains to the patient where he/she should go next, what examinations will be performed, and what instructions need to be followed. Once the exams are completed, the system automatically delivers the results to the patient.
- After the treatment has been administered, all of the patient’s data can be aggregated on a cloud platform so that a report on current treatment can be generated. The patient can check the results at any time using a mobile device. The device also sends the patient reminders about medication adherence and notifications about upcoming care, rehabilitation services, and insurance matters. The hospital also uses a telehealth platform to regularly assess the progress of the patient’s recovery and provide consultations as needed.
Samsung Medical Center in South Korea has rolled out an RFID system to enhance patient experience at its health screening center.
- Every patient is assigned an integrated RFID tag;
- the system can then automatically detect a patient’s location, display personalized information (e.g., waiting time) at a wall-mounted panel at that location,
- and send progress reports to an app on the patient’s mobile phone.
Cleveland Clinic Abu Dhabi (CCAD) is using digital apps as part of its treatment process to enhance patient experience.
- Before admission, patients can use the apps to communicate with the medical staff and finish all admission procedures.
- During their hospital stay, patients can use smart pads to access detailed clinical information and daily treatment plans, and to order food and other services.
- At discharge, CCAD uses mobile apps to send drug prescriptions to patients’ local pharmacies and to allow patients to confirm discharge times and check their bills.
Samsung Medical Center in South Korea has rolled out an RFID system to enhance patient experience at its health screening center.
Cleveland Clinic Abu Dhabi (CCAD) is using digital apps as part of its treatment process to enhance patient experience.

4.Smart hospitals are driven by analytics and big data.
On its own, a hospital does not always have sufficient data to unleash the full potential of analytics-it would benefit from having access to the clinical data amassed by other entities in the health ecosystem.
In all cases, the efforts to gather data should take into account both what is legally permissible and what is necessary to protect patient privacy.
However, when hospitals are able to easily access data via digital connections, they can use advanced analytics to make significant improvements in treatment quality and operational efficiency.
On its own, a hospital does not always have sufficient data to unleash the full potential of analytics-it would benefit from having access to the clinical data amassed by other entities in the health ecosystem.
For instance, analytics can help them
- expedite diagnosis,
- enable early risk identification and intervention, and
- optimize the utilization of key facilities.
Examples of such applications include:
Deep neural networks can help diagnose a range of diseases via image analysis, and research suggests that the AI now has a diagnostic accuracy rate comparable to that of human physicians.
- For instance, Sir Run Run Shaw Hospital, the first hospital in China to be accredited by the Joint Commission International, is studying how an AI system compares with the current standard for diagnosing liver disease.
- Research teams from Guangzhou Women and Children’s Medical Center in China and the University of California San Diego in the United States recently demonstrated that deep learning techniques can be used to process large quantities of EHR data and achieve an accuracy rate in diagnosing common childhood diseases comparable to that of experienced physicians.
Big data analytics of clinical records is being used to help patients in need of early intervention and care provision.
- In both developed and developing markets, we have found that it is feasible to build predictive models based on behavioral, medical, and claims data to identify high-risk patients for hospital readmission or chronic disease progression.
- Economically viable preventative programs or interventions can then be designed for target patient segments. In developing markets, a common challenge is the lack of high-quality data; however, our experience has shown that even with only a few years of claims data, it is possible to build a reasonably accurate risk model that allows for better design of population health management programs.
Big data analytics can also integrate a host of variables from hospital records (e.g., the time required to perform various procedures and time for patient transport) to improve operating room schedules.
As a result, the amount of idle time between procedures can be reduced.

5.Smart hospitals are holistic, interdisciplinary innovators.
Although smart hospitals require advanced IT technologies, becoming a smart hospital is not an IT project.
Rather, it is a holistic, deeply embedded, system-wide process that requires the participation of all staff, including physicians, nurses, and management.
Ongoing, open collaboration is also required to ensure that potential problems are detected rapidly-and potential solutions are quickly identified, designed, piloted, and rolled out.
This way, clinical processes, quality of care, and patient experience keep improving on a continuing basis, yet costs are kept under control.
Intermountain Healthcare, a US integrated system with a reputation for sustained quality improvement and innovation, provides a good example of how a system-wide effort can be run.
Clinical teams at the local and regional level are encouraged to identify prevention and management challenges in priority disease areas, conduct analyses, develop new care programs, and review progress once the programs are implemented.
The teams include physicians, nurses, statisticians, data managers, and support staff from medical informatics, finance, and other functions.
The rigorous processes used to develop new programs, as well as the involvement of diverse experts, ensure that the care delivery continues to be rationalized, optimized, and improved.

Implications for hospital investors and operators
Smart hospitals require smart healthcare ecosystems, and those ecosystems cannot exist in the absence of a sophisticated IT system capable of letting all entities share information.
A few private-sector healthcare organizations have been able to develop such systems on their own.
In many cases, however, governmental support is likely to be required.
- i.Regional governments
- ii.Hospital operators
i.Regional governments
In many developing markets, regional governments already lead healthcare system design and are major investors in hospitals.
In these cases, the governments have the option of using their administrative power to support the creation of smart, decentralized healthcare ecosystems.
Among the most important steps regional governments could consider taking are these:
- Lead overarching planning. Rather than build big, comprehensive, stand-alone hospitals, a government could take a more nuanced approach by issuing policy guidance that favors decentralization and then using its administrative power to ensure that a top-level plan for a smart healthcare ecosystem is developed. It could then supervise the system’s creation, making sure that all stakeholders have an opportunity to collaborate. By enabling all stakeholders to play to their strengths, the government can encourage them to cooperate.
- Build an integrated network platform. In some countries, government involvement may be crucial if the foundational IT system is to be brought online. It is not simply a question of the resources required to build the system. Connectivity among a network of providers is not sufficient-the providers must also be able to share appropriate data, which requires that operational and data standards be established. Government involvement could also help ensure that if a data center capable of integrating and storing the data from all providers is created, the center includes adequate controls to ensure that the data is used correctly and that patient confidentiality is protected. In developing markets, some cities and regions might have an opportunity to build a brand new health system; in these cases, the government could make certain that new technologies are integrated in the data infrastructure (in existing health systems, this type of integration is typically difficult and costly).
- Establish supporting mechanisms. A decentralized smart healthcare service ecosystem requires a series of supporting mechanisms to ensure effective information dissemination as well as strategies to ensure the alignment of different stakeholders. (For example, a payer might offer nonfinancial incentives to patients to encourage them to try innovative digital care tools or disease management programs.)
ii.Hospital operators
Although regional governments are often deeply involved in the initial creation of a smart healthcare ecosystem, it is the hospital operators (from either the public or private sectors) who play a crucial role in ensuring that a smart hospital functions effectively.
This is particularly true for the operators of existing hospitals, who will have to lead the staff through a significant transformation.
These operators must be able to envision how the hospital will operate in the future, communicate that vision to the staff, and help them develop the capabilities needed to ensure the transformation’s success.
Among the important steps that all hospital operators could take are:
- Help build the smart healthcare ecosystem. Hospital operators can benefit if they help build the ecosystem, since it gives them greater latitude to position their facilities within it. Rather than trying to provide all services, the operators should identify the diagnostic and treatment services that other entities cannot provide, and then determine how their hospital can efficiently deliver those services with a high level of quality.
- Design smart hospital “use cases.” In the not-distant future, hospitals will no longer see “smart” as a goal, but rather as a way to differentiate themselves and promote sustainable innovation. A sustainable smart hospital should have a grand vision, a clear roadmap toward specific use cases (e.g., being the leading cardiology center in the country), and renewed processes in place to make the vision work, rather than blind investments centered on hardware upgrades.
- Enhance an innovative environment. Although smart hospitals require innovative technologies, it is even more important that the hospital staff continually innovates to improve patient outcomes. Sophisticated hardware and software platforms can only take a hospital so far. Among the steps hospital operators can take are these:
- Establish open collaborations with universities, research institutes, and innovative technology companies to embolden the staff to develop new approaches that improve care quality.
- Set up similar collaborations with government agencies, opinion leaders, and industry unions to encourage the staff to think about healthcare delivery in broader terms.
- Make significant investments in hospital staff to deepen their knowledge of what smart hospitals-and smart ecosystems-can do, and to build the capabilities needed to ensure that the best outcomes are achieved. The best results are often achieved when as much attention is paid to change management as to the changes themselves. Addressing the mind-sets and cultures of both the clinical and nonclinical staff is crucial.

In summary, the smart hospitals of the future will look very different from the hospitals of today and the past.
Smart hospitals will operate in an environment of decentralized care provision and will no longer serve as the predominant (or in some countries, sole) provider of all healthcare interventions.
Smart hospitals will focus instead on a core set of in-house services and connect with a broader ecosystem for delivery of other care services in an agile and efficient manner.
In smart hospitals, digitally enabled clinical staff will be able to deliver better outcomes and a more integrated patient experience, and continuously innovate in care delivery.