Michael E. Porter, Ph.D.
In any field, improving performance and accountability depends on having a shared goal that unites the interests and activities of all stakeholders. In health care, however, stakeholders have myriad, often conflicting goals, including access to services, profitability, high quality, cost containment, safety, convenience, patient-centeredness, and satisfaction. Lack of clarity about goals has led to divergent approaches, gaming of the system, and slow progress in performance improvement.
Achieving high value for patients must become the overarching goal of health care delivery, with value defined as the health outcomes achieved per dollar spent.1 This goal is what matters for patients and unites the interests of all actors in the system. If value improves, patients, payers, providers, and suppliers can all benefit while the economic sustainability of the health care system increases.
Value — neither an abstract ideal nor a code word for cost reduction — should define the framework for performance improvement in health care. Rigorous, disciplined measurement and improvement of value is the best way to drive system progress. Yet value in health care remains largely unmeasured and misunderstood.
Value should always be defined around the customer, and in a well-functioning health care system, the creation of value for patients should determine the rewards for all other actors in the system. Since value depends on results, not inputs, value in health care is measured by the outcomes achieved, not the volume of services delivered, and shifting focus from volume to value is a central challenge. Nor is value measured by the process of care used; process measurement and improvement are important tactics but are no substitutes for measuring outcomes and costs.
Since value is defined as outcomes relative to costs, it encompasses efficiency. Cost reduction without regard to the outcomes achieved is dangerous and self-defeating, leading to false “savings” and potentially limiting effective care.
Outcomes, the numerator of the value equation, are inherently condition-specific and multidimensional. For any medical condition, no single outcome captures the results of care. Cost, the equation’s denominator, refers to the total costs of the full cycle of care for the patient’s medical condition, not the cost of individual services. To reduce cost, the best approach is often to spend more on some services to reduce the need for others.
Health care delivery involves numerous organizational units, ranging from hospitals to physicians’ practices to units providing single services, but none of these reflect the boundaries within which value is truly created. The proper unit for measuring value should encompass all services or activities that jointly determine success in meeting a set of patient needs. These needs are determined by the patient’s medical condition, defined as an interrelated set of medical circumstances that are best addressed in an integrated way. The definition of a medical condition includes the most common associated conditions — meaning that care for diabetes, for example, must integrate care for conditions such as hypertension, renal disease, retinal disease, and vascular disease and that value should be measured for everything included in that care.1
For primary and preventive care, value should be measured for defined patient groups with similar needs. Patient populations requiring different bundles of primary and preventive care services might include, for example, healthy children, healthy adults, patients with a single chronic disease, frail elderly people, and patients with multiple chronic conditions.
Care for a medical condition (or a patient population) usually involves multiple specialties and numerous interventions. Value for the patient is created by providers’ combined efforts over the full cycle of care. The benefits of any one intervention for ultimate outcomes will depend on the effectiveness of other interventions throughout the care cycle.
Accountability for value should be shared among the providers involved. Thus, rather than “focused factories” concentrating on narrow groups of interventions, we need integrated practice units that are accountable for the total care for a medical condition and its complications.
Because care activities are interdependent, value for patients is often revealed only over time and is manifested in longer-term outcomes such as sustainable recovery, need for ongoing interventions, or occurrences of treatment-induced illnesses.2 The only way to accurately measure value, then, is to track patient outcomes and costs longitudinally.
For patients with multiple medical conditions, value should be measured for each condition, with the presence of the other conditions used for risk adjustment. This approach allows for relevant comparisons among patients’ results, including comparisons of providers’ ability to care for patients with complex conditions.
The current organizational structure and information systems of health care delivery make it challenging to measure (and deliver) value. Thus, most providers fail to do so. Providers tend to measure only what they directly control in a particular intervention and what is easily measured, rather than what matters for outcomes. For example, current measures cover a single department (too narrow to be relevant to patients) or outcomes for a whole hospital, such as infection rates (too broad to be relevant to patients). Or they measure what is billed, even though current reimbursement practices are misaligned with value. Similarly, costs are measured for departments or billing units rather than for the full care cycle over which value is determined. Faulty organizational structure also helps explain why physicians fail to accept joint responsibility for outcomes, blaming lack of control over “outside” actors involved in care (even those in the same hospital) and patients’ compliance.
The concept of quality has itself become a source of confusion. In practice, quality usually means adherence to evidence-based guidelines, and quality measurement focuses overwhelmingly on care processes. For example, of the 78 Healthcare Effectiveness Data and Information Set (HEDIS) measures for 2010, the most widely used quality-measurement system, all but 5 are clearly process measures, and none are true outcomes.3 Process measurement, though a useful internal strategy for health care institutions, is not a substitute for measuring outcomes. In any complex system, attempting to control behavior without measuring results will limit progress to incremental improvement. There is no substitute for measuring actual outcomes, whose principal purpose is not comparing providers but enabling innovations in care. Without such a feedback loop, providers lack the requisite information for learning and improving. (Further details about measuring value are contained in a framework paper, “Value in Health Care,” in Supplementary Appendix 1, available with the full text of this article at NEJM.org.)
Measuring, reporting, and comparing outcomes are perhaps the most important steps toward rapidly improving outcomes and making good choices about reducing costs.4 Systematic, rigorous outcome measurement remains rare, but a growing number of examples of comprehensive outcome measurement provide evidence of its feasibility and impact.
Determining the group of relevant outcomes to measure for any medical condition (or patient population in the context of primary care) should follow several principles. Outcomes should include the health circumstances most relevant to patients. They should cover both near-term and longer-term health, addressing a period long enough to encompass the ultimate results of care. And outcome measurement should include sufficient measurement of risk factors or initial conditions to allow for risk adjustment.
For any condition or population, multiple outcomes collectively define success. The complexity of medicine means that competing outcomes (e.g., near-term safety versus long-term functionality) must often be weighed against each other.
The outcomes for any medical condition can be arrayed in a three-tiered hierarchy (see Figure 1), in which the top tier is generally the most important and lower-tier outcomes involve a progression of results contingent on success at the higher tiers. Each tier of the framework contains two levels, each involving one or more distinct outcome dimensions. For each dimension, success is measured with the use of one or more specific metrics.
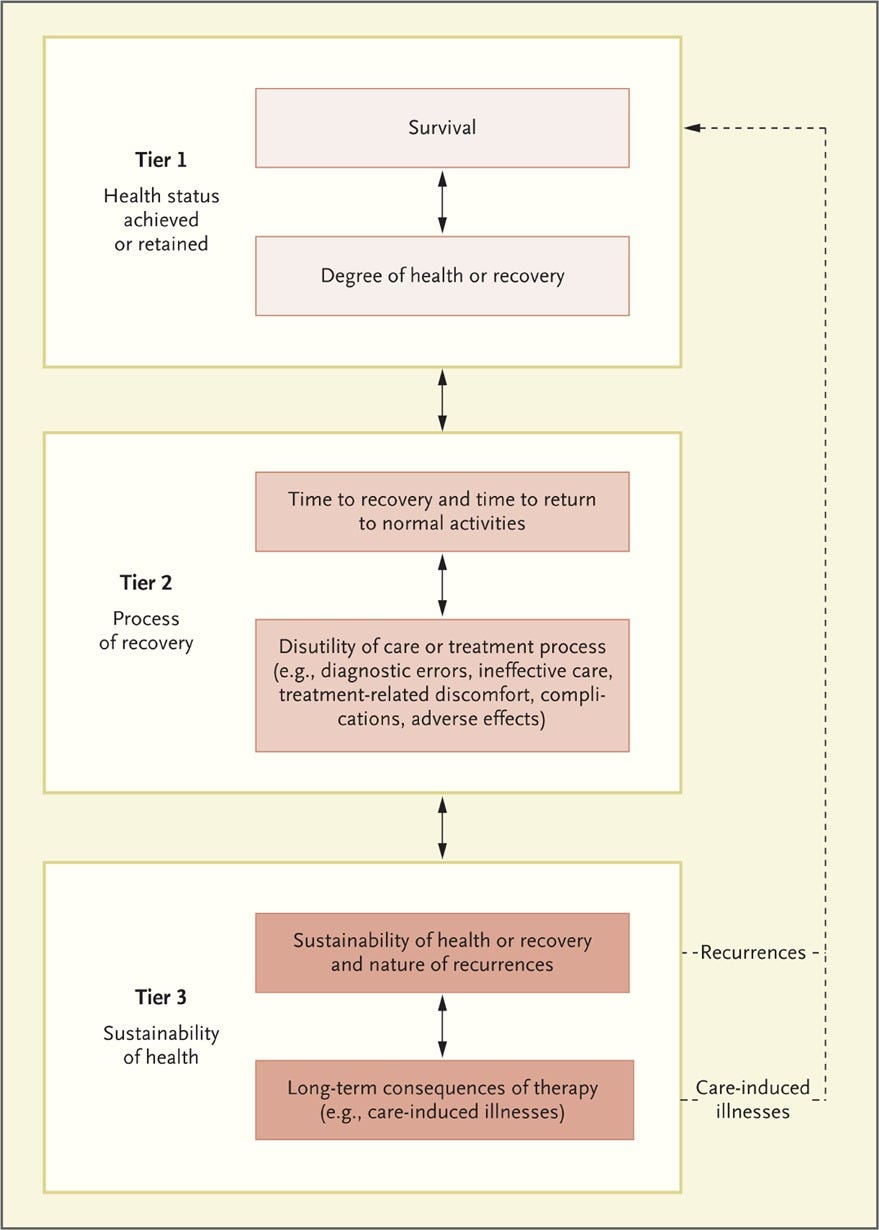
Tier 1 is the health status that is achieved or, for patients with some degenerative conditions, retained. The first level, survival, is of overriding importance to most patients and can be measured over various periods appropriate to the medical condition; for cancer, 1-year and 5-year survival are common metrics. Maximizing the duration of survival may not be the most important outcome, however, especially for older patients who may weight other outcomes more heavily. The second level in Tier 1 is the degree of health or recovery achieved or retained at the peak or steady state, which normally includes dimensions such as freedom from disease and relevant aspects of functional status.
Tier 2 outcomes are related to the recovery process. The first level is the time required to achieve recovery and return to normal or best attainable function, which can be divided into the time needed to complete various phases of care. Cycle time is a critical outcome for patients — not a secondary process measure, as some believe. Delays in diagnosis or formulation of treatment plans can cause unnecessary anxiety. Reducing the cycle time (e.g., time to reperfusion after myocardial infarction) can improve functionality and reduce complications. The second level in Tier 2 is the disutility of the care or treatment process in terms of discomfort, retreatment, short-term complications, and errors and their consequences.
Tier 3 is the sustainability of health. The first level is recurrences of the original disease or longer-term complications. The second level captures new health problems created as a consequence of treatment. When recurrences or new illnesses occur, all outcomes must be remeasured.
With some conditions, such as metastatic cancers, providers may have a limited effect on survival or other Tier 1 outcomes, but they can differentiate themselves in Tiers 2 and 3 by making care more timely, reducing discomfort, and minimizing recurrence.
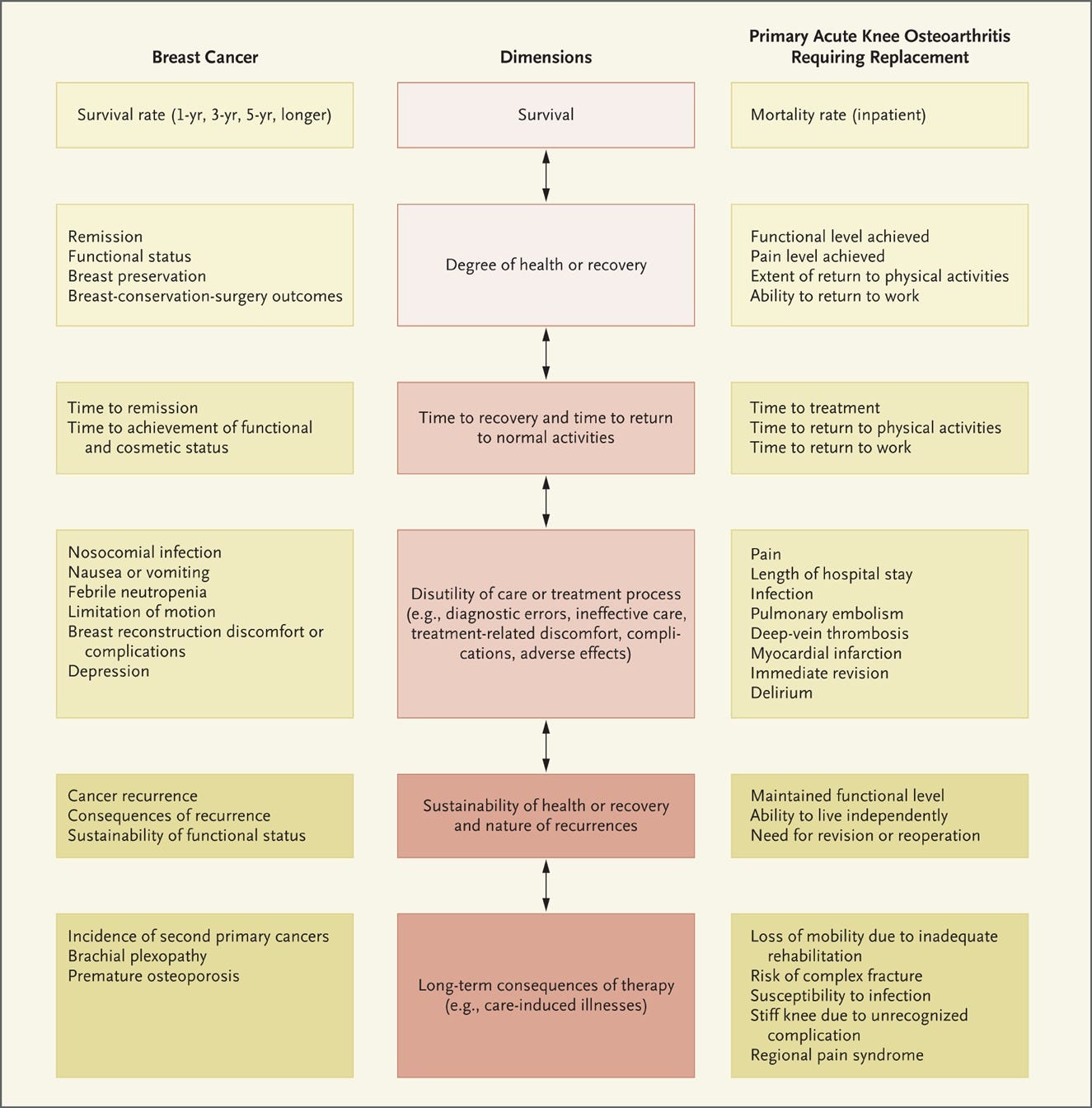
Each medical condition (or population of primary care patients) will have its own outcome measures. Measurement efforts should begin with at least one outcome dimension at each tier, and ideally one at each level. As experience and available data infrastructure grow, the number of dimensions (and measures) can be expanded.
Improving one outcome dimension can benefit others. For example, more timely treatment can improve recovery. However, measurement can also make explicit the tradeoffs among outcome dimensions. For example, achieving more complete recovery may require more arduous treatment or confer a higher risk of complications. Mapping these tradeoffs, and seeking ways to reduce them, is an essential part of the care-innovation process.
Figure 2 illustrates possible outcome dimensions for breast cancer and acute knee osteoarthritis requiring knee replacement. Most current measurement efforts fail to capture such comprehensive sets of outcomes, which are needed to fully describe patients’ results. No organization I know of systematically measures the entire outcome hierarchy for the medical conditions for which it provides services, though some are making good progress. (Further details, including risk adjustment, are addressed in a framework paper, “Measuring Health Outcomes,” in Supplementary Appendix 2, available at NEJM.org.)
The most important users of outcome measurement are providers, for whom comprehensive measurement can lead to substantial improvement.5 Outcomes need not be reported publicly to benefit patients and providers, and public reporting must be phased in carefully enough to win providers’ confidence. Progression to public reporting, however, will accelerate innovation by motivating providers to improve relative to their peers and permitting all stakeholders to benefit fully from outcome information.
Current cost-measurement approaches have also obscured value in health care and led to cost-containment efforts that are incremental, ineffective, and sometimes even counterproductive. Today, health care organizations measure and accumulate costs around departments, physician specialties, discrete service areas, and line items such as drugs and supplies — a reflection of the organization and financing of care. Costs, like outcomes, should instead be measured around the patient. Measuring the total costs over a patient’s entire care cycle and weighing them against outcomes will enable truly structural cost reduction, through steps such as reallocation of spending among types of services, elimination of non–value-adding services, better use of capacity, shortening of cycle time, provision of services in the appropriate settings, and so on.
Much of the total cost of caring for a patient involves shared resources, such as physicians, staff, facilities, and equipment. To measure true costs, shared resource costs must be attributed to individual patients on the basis of actual resource use for their care, not averages. The large cost differences among medical conditions, and among patients with the same medical condition, reveal additional opportunities for cost reduction. (Further aspects of cost measurement and reduction are discussed in the framework paper “Value in Health Care.”)
The failure to prioritize value improvement in health care delivery and to measure value has slowed innovation, led to ill-advised cost containment, and encouraged micromanagement of physicians’ practices, which imposes substantial costs of its own. Measuring value will also permit reform of the reimbursement system so that it rewards value by providing bundled payments covering the full care cycle or, for chronic conditions, covering periods of a year or more. Aligning reimbursement with value in this way rewards providers for efficiency in achieving good outcomes while creating accountability for substandard care.
Disclosure forms provided by the author are available with the full text of this article at NEJM.org.
This article (10.1056/NEJMp1011024) was published on December 8, 2010, at NEJM.org.
Michael Porter is the founder of the modern strategy field and one of the world’s most influential thinkers on management and competitiveness. The author of 19 books and over 130 articles, he is the Bishop William Lawrence University Professor at Harvard Business School and the director of the school’s Institute for Strategy and Competitiveness, which was founded in 2001 to further his work and research.
Porter and Teisberg introduced value-based healthcare (VBHC) in their seminal 2006 book, Redefining Health Care.
From Harvard Business School, Boston.
Originally published at https://www.nejm.org.












