Leaders at Hospital de Clínicas de Porto Alegre, a public tertiary care university teaching hospital, created a flexible model that could be scaled up or down based on need, revising the care delivery model to enable ward beds to be used for Covid-19 patients in need of critical care.
NEJM — New England Journal of Medicine
Mariana Rangel-Ribeiro Falcetta, MD; Dimitris Varvaki Rados, MD, PhD;
José Miguel Dora, MD, PhD
September 7, 2021
Summary
Brazil has faced significant challenges during the coronavirus pandemic. Early on, Hospital de Clínicas de Porto Alegre was appointed as a regional reference hospital for the treatment of critically ill patients with Covid-19.
Despite increasing the number of ICU beds, Covid-19 admissions surpassed operational capacity, and critical patients had to be treated outside ICUs.
Hospital administrative and on-site integrated care delivery leaders collaborated to develop a flexible Covid-19 ward model that could expand and contract based on need.
The institution was able to increase the number of Covid-19 dedicated professionals and beds, improve patient monitoring, institute a noninvasive ventilatory support team, and ensure 24–7 continuity of care and assertive transition of care communication.
Lessons learned from abroad and from the early pandemic days led to a ward able to adapt to provide care to critical patients outside ICUs. This flexible system provided the means to face the health care challenge.
Key Takeaways
- Implementation of specialized care transition strategies (a Covid-19 huddle and morning report) improves patient care and contributes to efficient bed management.
- Formation of an integrated team with ventilatory support skills is essential given the respiratory challenges associated with the virus.
- Obtaining and supporting adequate ventilatory support equipment and monitoring resources is necessary given the design of the temporary Covid-19 wards.
- Alignment of and continuous communication among colleagues serving the Covid-19 wards, the emergency department, and the intensive care units facilitates efficiency and a trusting environment.
- Identifying a problem and implementing of rapid response that involves executive leadership and frontline care delivery teams enhances development and deployment of an appropriate and flexible set of solutions.
The Challenge
With the worsening of the Covid-19 pandemic during the year 2020, the demand for intensive care unit (ICU) beds and ward beds increased abruptly in Brazil.
ICU occupancy rapidly reached 100% and, as all possible expansion options had been implemented, we had no options for further increases to the ICU. As a result, critical patients had to be accommodated at non-ICU beds and we had to attend to the unique patient profile of those infected with the coronavirus in common medical wards (Appendix).
Our institution, Hospital de Clínicas de Porto Alegre (HCPA), is a public tertiary care university teaching hospital in southern Brazil. Early in the Covid-19 pandemic, the federal government appointed HCPA as a regional reference hospital for the treatment of critically ill patients with Covid-19. As of August 2021, HCPA has 921 beds, divided as follows: 642 medical ward beds, 62 adult ICU beds, 135 ICU dedicated Covid-19 beds, 13 pediatric ICU beds, 20 neonatal ICU beds, 41 adult emergency room beds, and 8 pediatric emergency room beds.
Since March 2020, when the Covid-19 pandemic was declared, the hospital has undergone several sequential adaptations to care for this patient profile with its specific demands. When classified as a reference center for the treatment of Covid-19 critically ill patients, we implemented 85 extra beds in the ICU, and, as the pandemic worsened, that number grew to 135 new ICU beds. Covid-19-specific ward beds were also created, going from zero to a total of 84 (by relocating non-Covid-19 patients and postponing elective surgeries). However, as the number of patients arriving at our hospital increased and surpassed our operational capacity, critical patients with acute respiratory failure had to be treated outside ICUs. As a result, our 84-bed Covid-19 ward was filled with patients requiring advanced respiratory support.
In addition, we had to deal with national public health system limitations and the rapid spread of the epidemic in a country marked by wide socioeconomic inequalities and other health risks (such as age, infrastructure, and burden of chronic disease).
The Goal
Our goal was to meet the demands — with quality — of our increasingly severe patients in the wards, providing noninvasive ventilatory support, adequate monitoring, and respiratory physiotherapy.
The Execution
The development and deployment of this plan required both general and specific improvements.
General Improvements
Increase of Medical Teams
Initially, one single team concentrated all inpatient care in the wards. With the rapid increase in the number of patients during the first half of 2020, this team became overwhelmed. Thus, more Covid-19-specific teams were created to assist Covid-19 ward patients. Initially they followed the usual teaching medical-team structure, composed of a preceptor and two to three residents. Later, more professionals were relocated to the Covid-19 ward and additional teams were created. In March 2021, during what was then the most critical moment of the pandemic in southern Brazil, a total of seven medical teams were working in the ward to assist exclusively patients with Covid-19. These ward teams were a mix of teaching (preceptor and residents) and of non-teaching (two or three staff physicians). On average, each team assisted 8–12 patients.
On a daily basis, a representative from the internal bed management committee and from the social service discuss in person with Covid-19 medical teams the possibility of discharging patients from the hospital, transferring patients to post-acute care hospitals, and monitoring the need for ICU care.
Increase of Beds
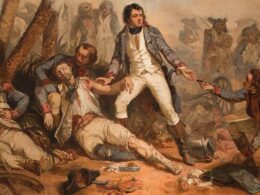
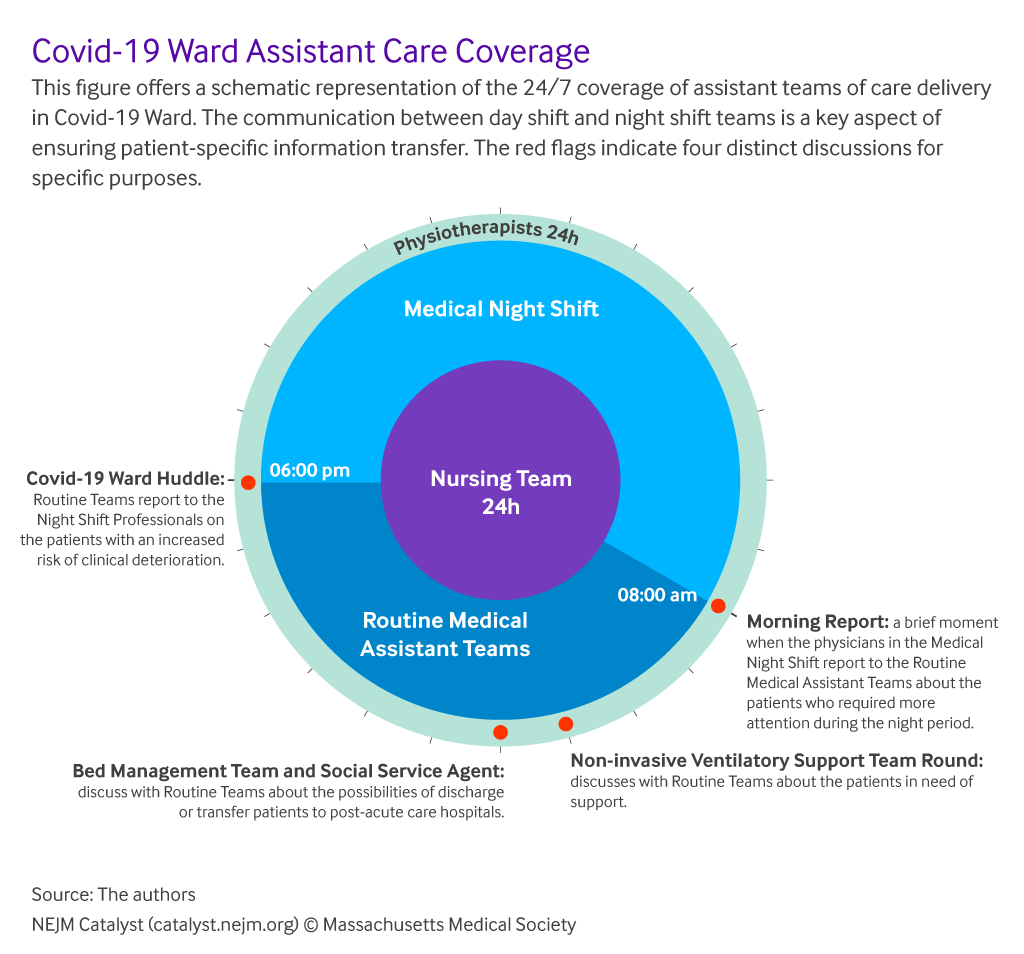
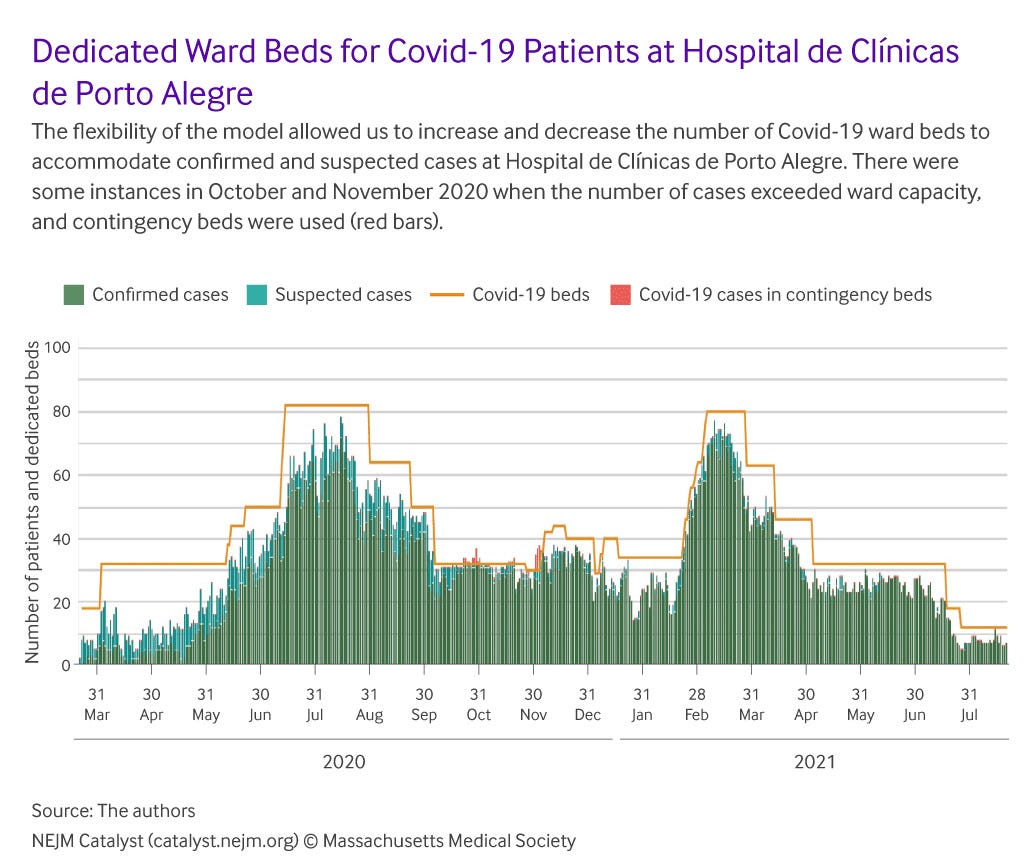
The number of ward beds to assist patients with Covid-19 was adapted to the demand at different epidemiological moments ().
Initially, 18 beds were made available, with a subsequent increase to 32, then 50, and a further increase to 82 beds in August 2020. Conditions allowed for a reduction to 32 beds during the months of September and October 2020, but a new increase to 84 was necessary in March 2021, when the second wave reached our country.
On March 26, 2021, it was possible to reduce Covid-19 ward beds from 82 to 63. On April 9, ward beds were reduced to 43, in early May to 32, and then again on July 14 to 18 beds. As of late July 2021, we have 12 beds in the wards and one dedicated team. The variations in the number of beds shows great elasticity of the system and, despite the quick installation, it was a complex process and mobilized a number of staff (administrators, nurses, physiotherapists, and physicians).
Vaccination was a determinant for reducing both the demand for ward beds and the severity of hospitalized patients. During our regional efforts, the nation and our state — Rio Grande do Sul — continued to make progress in delivering vaccinations. On March 25, 2021, only 12.8% of the state’s population of approximately 11.4 million inhabitants had been vaccinated with the first dose and 3.9% were fully vaccinated. By April 30, 2021, these numbers were 27.0% and 12.2% respectively, progressing to 54.9% and 21.9% on June 30, 2021, and 71.5% and 33.1% on July 28, 2021. By July 29, 2021, the percentage of the population that was fully vaccinated was 45.2% in the city of Porto Alegre, 33.1% in the state of Rio Grande do Sul, and 18.7% in the country.
A third wave of Covid-19 cases was described in several states in Brazil in early June 2021; however, vaccination distribution and administration efforts in our state meant that we did not experience that wave and we did not see an increase in the demand for Covid-19 ward beds in our hospital at that time. We also observed a decrease in the severity of symptoms of patients who were hospitalized during this period.
Another factor to consider is the still-low circulation of the Delta variant in our state. As of August 7, 2021, the Delta variant (B.1.617.2) has been identified in 88 (5.8%) of 1,514 samples analyzed for variants of interest, with the P.1 variant (Gamma) the most seen variant among Covid-19 cases in Rio Grande do Sul.
Institution of Bed Management Team Dedicated to Covid-19
On a daily basis, a representative from the internal bed management committee and from the social service discuss in person with Covid-19 medical teams the possibility of discharging patients from the hospital, transferring patients to post-acute care hospitals, and monitoring the need for ICU care.
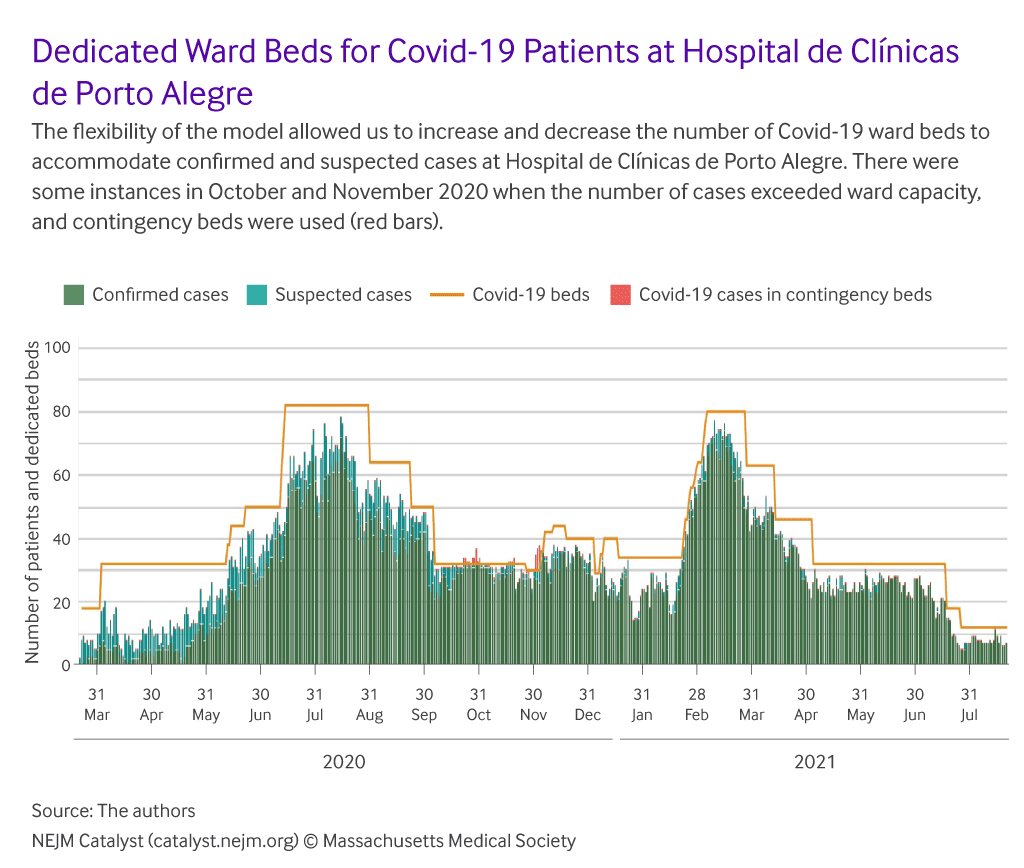
24–7 Continuity of Care
To ensure inpatient 24–7 continuity of care, we instituted a daily Covid-19 Ward Huddle for exchanging brief information, minimizing failures, and providing timely reevaluations. It was set up 30 minutes before the night shift (6:00 p.m.) starts. The objective was to point out to the night team the patients who were at increased risk of clinical deterioration and who needed to be reassessed by the physiotherapist, by the medical physicians on duty, or by the rapid response team (RRT), which comprises ICU and internist physicians. Participants in the Covid-19 Ward Huddle are one representative of each Covid-19 medical team, physiotherapists and nurses of the Covid-19 wards, one medical resident on duty exclusively to Covid-19 ward (for the night shift), one preceptor physician of the night shift, and one physician of the RRT.
Participants in the Covid-19 Ward Huddle are one representative of each Covid-19 medical team, physiotherapists and nurses of the Covid-19 wards, one medical resident on duty exclusively to Covid-19 ward (for the night shift), one preceptor physician of the night shift, and one physician of the RRT.
Additionally, at the end of the night shift (8:00 a.m.), the physicians in charge perform a morning report and contact the daily Medical Assistant Teams to notify them about Covid-19 patients in need of early morning reevaluation. A senior Internal Medicine resident leads the event and addresses reevaluation plans for these most critical patients. shows a schematic representation of 24–7 coverage of Covid-19 assistant teams (care delivery professionals).
The standard medical teams in daily routine are composed of a medical preceptor and two to three resident physicians (standard team). Teams without the usual composition were formed at the most critical moments of the pandemic, where a team had only two assistant medical physicians each.
Monitoring
Early in the pandemic there was a change in the functioning of medical teams. Usually, medical teams have patients in different wards. But due to the need to isolate Covid-19 patients, the dedicated Covid-19 medical teams’ activities were restricted to the Covid-19 wards. This simple change in the way care is delivered led to some unanticipated benefits, including improved patient monitoring and enhanced integration among physiotherapists, nurses, and medical staff. In addition, early in the pandemic, it was clear that more intensive monitoring would be needed in a challenging environment; our wards are composed of closed rooms with two beds. When ICU capacity was overwhelmed, the medical, physiotherapist, and nurse staffs worked in a synchronous way to ensure adequate monitoring, despite the physical limitations of closed rooms. Also, four beds received multiparameter monitors, and respective telemetry was installed at the nursing station, which allowed for the continuous monitoring of the most critical patients of the Covid-19 wards.
Specific Improvements
Implementing a Specialized Ventilatory Support Team
To deploy specific knowledge to the Covid-19 medical teams, we instituted medical co-management with a team of pneumologists specialized in noninvasive ventilatory support. Early in the pandemic this group of pneumologists was relocated to help ward teams with their expertise. This ventilatory team assisted in the evaluation of patients in need of this kind of therapy with guidance on indication, definition of parameters, adjustment, and withdrawal. Currently, representatives of the ventilatory support team meet daily in small rounds with the Covid-19 medical teams to discuss the current ventilatory-support patients, or potential candidates.
Specific Training for Assistance Teams in the Ventilatory Support
All physicians working on Covid-19 teams received formal training in noninvasive ventilatory support. Additionally, periodic hands-on training in noninvasive ventilatory support and high-flow nasal cannula was offered to the Covid-19 teams (physicians, nurses, and physiotherapists).
This simple change in the way care is delivered led to some unanticipated benefits, including improved patient monitoring and enhanced integration among physiotherapists, nurses, and medical staff.
Increase in the Number of Physiotherapists
To attend to the demand created by Covid-19 patients, physiotherapists from other areas were reallocated to the Covid-19 wards. Additionally, the institution had to hire more physiotherapists. At first, Covid-19 physiotherapist teams worked in 6-hour shifts, covering the period from 8:00 a.m. to 11:00 p.m. Later, the shift was expanded to cover the period from 8:00 a.m. to 1:00 a.m., and now the team covers 24 hours a day (with a limit of 12 consecutive hours per physician).
Equipment
A total of 18 noninvasive ventilatory machines available at our hospital were relocated to the Covid-19 wards by August 2020. Additionally, in March 2021, we received 12 noninvasive ventilatory machines by donation and acquired 4 high-flow nasal cannulas for use in the Covid-19 wards.
The Hurdles
Our hurdle was to implement the above cited adjustments, in a short time frame, with limited resources ( Table 1).
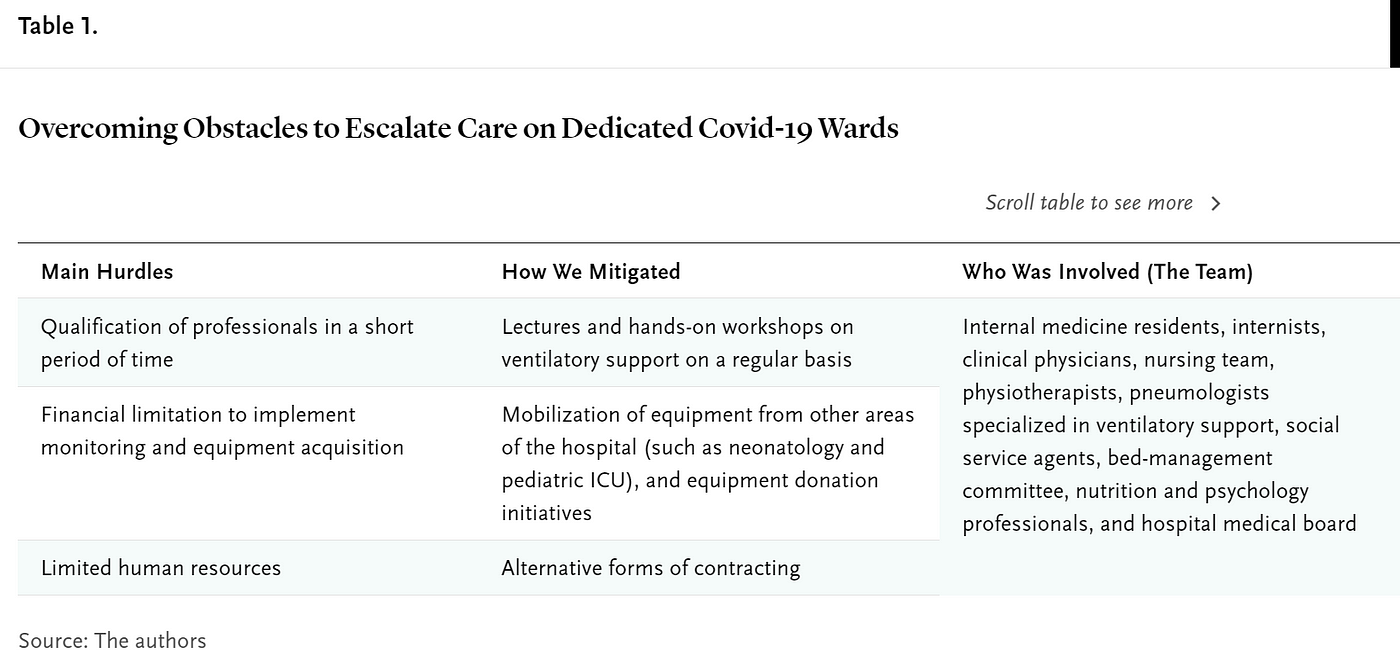
ualification of professionals in a short period of time
Lectures and hands-on workshops on ventilatory support on a regular basis
Internal medicine residents, internists, clinical physicians, nursing team, physiotherapists, pneumologists specialized in ventilatory support, social service agents, bed-management committee, nutrition and psychology professionals, and hospital medical board
Financial limitation to implement monitoring and equipment acquisition
Mobilization of equipment from other areas of the hospital (such as neonatology and pediatric ICU), and equipment donation initiatives

Limited human resources
Alternative forms of contracting
Lectures and hands-on ventilatory support workshops were one of the most important means to continually train new members and retrain staff. Workshops were regularly provided in ward discussion rooms, always in small groups.
Equipment (mostly noninvasive ventilators and high-flow nasal cannulas) were directed to ICU and emergency departments, in addition to the invasive mechanical ventilation resources already allocated in those areas. Later, as patient severity increased in the wards, more equipment was relocated to the wards and additional equipment was bought with Covid-19-specific funds.
Regarding work capacity, our institution usually hires through a selective process and holds positions for an indefinite term. Due to the pandemic, we started to carry out simplified processes (fewer steps) for temporary jobs, and, at the most critical moment of the pandemic, we had to hire health professionals temporarily without the usual competitive process of comparing multiple candidates.
The Team
Internal medicine, infectology, and pneumology physicians, nurses, physiotherapists, and administrative staff teamed up to face the challenge. With the evolving demand and complexity of the Covid-19 wards, the need to establish care-coordination leadership was evident. By August 2020, at the request of the hospital’s Vice President for Medical Affairs, the Internal Medicine Division assumed responsibility for the medical coordination of care for the Covid-19 ward.
Metrics
Admitted Patients
From March 18, 2020, to August 1, 2021, a total of 3,405 patients (2,501 confirmed Covid-19 cases and 904 suspected cases) were admitted to the Covid-19 wards; the distribution throughout that time can be seen in . Most of our confirmed Covid-19 patients, 49.7%, came from the emergency department, 28.7% from the ICU, and 21.6% from non-Covid-19 wards.
Lectures and hands-on ventilatory support workshops were one of the most important means to continually train new members and retrain staff. Workshops were regularly provided in ward discussion rooms, always in small groups.
Clinical Results
By August 1, 2021, we had assisted 2,501 confirmed cases in Covid-19 wards. Of these, 50.8% were men, and the mean age was 56.2 ± 17.2 years. The median length of stay in the Covid-19 wards was 4.8 days (P25–75 2.2–7.9); however, the total length of stay in the hospital was longer, 10.4 days (P25–75 4.8–22.2). Patients could be discharged home (40.1%), transferred to post-acute care hospitals (3.4%), or transferred to a bed in the hospital’s ICU (21.3%) or a non-Covid-19 ward (28.9%).
Our Covid-19 ward mortality was 158 (6.3%). Over time, the care delivered to Covid-19 patients in the wards resulted in a low percentage of deaths in this environment (review of medical records of patients who died in the wards showed that a considerable share — 97% — had advance care directives to not be resuscitated, mechanically ventilated, or to go to the ICU). When considering mortality in patients who were later moved from that Covid-19 ward to the ICU, the mortality number went up to 548 patients (21.9%). Of note, only confirmed cases of Covid-19, with a positive rt-PCR test, are reported here.
Although we cannot directly compare the developed model, considering the severity of Covid-19 and the severity profile of our patients (as a tertiary hospital), we consider this to be a low mortality rate in the Covid-19 ward. The literature shows an in-hospital mortality rate of 17%-32%,-however that rate is considered in all hospital environments.
The mortality rate that goes up to 21.9% (548) refers to patients who died in the Covid-19 wards (158) plus the ones who passed through the ward then went to ICU and died there (390). It does not count patients who went straight from the emergency room to ICU or came from other hospitals to our ICU and died there. These two flows account for a high number of patients in our institution, since it is a critical care reference for south Brazil. Still, overall Covid-19 mortality in our hospital is 23.0%.
Where to Start
The first steps to improve Covid-19 ward care were the identification of the problem and the implementation of rapid response through both administrative and on-site integrated care delivery leadership. Although these steps may seem obvious, they must not be overlooked. The core mission was to bring together medical teams, noninvasive ventilatory support consultants, nurses, and physiotherapists to care for patients with advanced ventilatory support needs outside the intensive care environment. Besides that, alignment and continuous communication with emergency and intensive care units and a trusting environment are also key points.
Mariana Rangel-Ribeiro Falcetta, MD
Physician, Internal Medicine Division, Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
Dimitris Varvaki Rados, MD, PhD
Physician, Residency Supervisor, Executive Coordinator of Bed Management Team, Internal Medicine Division, Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
José Miguel Dora, MD, PhD
Head of the Internal Medicine Division, Coordinator of the Digital Governance Committee, Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil; Professor of Medicine, Internal Medicine Department and Post-Graduation Program in Endocrinology, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
PDF version
chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Fcatalyst.nejm.org%2Fdoi%2Fpdf%2F10.1056%2FCAT.21.0251