Credit: PBS
73 Experts Offer a Blueprint for Preventing Another Pandemic
Time
BY JEFFREY KLUGER
Thursday, June 10, 2021
As long as there are pathogens and hosts there will be outbreaks of disease. The best human beings can do is learn from previous experience — studying what went right or wrong in one pandemic and applying that wisdom to the next.
In an effort to do just that, TIME’s science and health team — led for this project by my colleague Emily Barone, with guidance from the University of Washington Alliance for Pandemic Preparedness — polled 73 experts in public health, infectious disease, immunology, hospital administration, data and technology, environment and climate, and more.
TIME sent each a list of about 50 initiatives that could mitigate the next health crisis and asked them to score each strategy’s priority and feasibility on a scale of 1 to 5.
When it came to priority, experts put
-
bolstering vaccine research and manufacturing at the top of the list, followed by
-
improving systems that track and alert the world to new diseases.
What’s more, both these proposals also scored highly on feasibility, meaning experts saw few barriers to implementation — indeed, the current pandemic stands as proof of that, Dr. Seth Berkley, CEO of GAVI, the Vaccine Alliance, reminded TIME, as he analyzed the results of the survey.
“When it came to COVID-19 … the scientific and vaccine manufacturing community rallied, producing the first safe and effective vaccine in record time — just 327 days.”
Similarly, Dr. Julie Gerberding, former director of the U.S. Centers for Disease Control and Prevention, and another analyst who weighed in on the survey results, was struck by the power of disease surveillance during the current crisis.
“Experts agree that a robust system for detecting emerging infections on a global basis is now technologically feasible,” she said, “ if we figure out coordinated planning and appropriate investment in modern data analytics and molecular diagnostics.”
Other initiatives that experts also ranked as essential look tougher to accomplish. Ranked as high priority but less feasible were
-
expanding health care access,
-
distributing vaccines fairly and
-
other strategies addressing inequalities that have exacerbated COVID-19’s toll on vulnerable populations.
That will take local action. “Individual governments can take matters into their own hands.
First, they must get their own shops in order,” says Dr. Leana Wen, former Health Commissioner of Baltimore. “They need to rigorously evaluate their country’s pandemic response and make necessary investments to the local public health infrastructure.”
None of these insights will, by themselves, prevent the next pandemic.
But all may make us better prepared to face it down.
In hindsight, we could have prepared more seriously, reacted more quickly, communicated more effectively, protected one another more actively and so on. But the next time there’s a public-health threat, we will do better. Right?
Not necessarily. Knowing the many ways that we mishandled COVID-19 is a bit like knowing the number of pages in a textbook to study before an exam. It gives us an idea of the task ahead but not how difficult the work will be.
True preparation means studying the problems and working out solutions. There’s a lot of material to cover from this pandemic.
And we have no idea when the next test is coming.
TIME’s science and health team, with guidance from the University of Washington Alliance for Pandemic Preparedness, set out to make a study guide of sorts. In late May, TIME sent a list of about 50 initiatives that could mitigate the next health crisis to experts who could expect to be involved. We asked them to score each strategy’s priority and feasibility on a scale of 1 to 5. Seventy-three responses came back from thought leaders in public health, infectious disease, immunology, hospital administration, data and technology, environment and climate, health inequity, supply chains and biosecurity. A third of them were outside the U.S., spanning 16 countries.
Strategies to mitigate future health crises
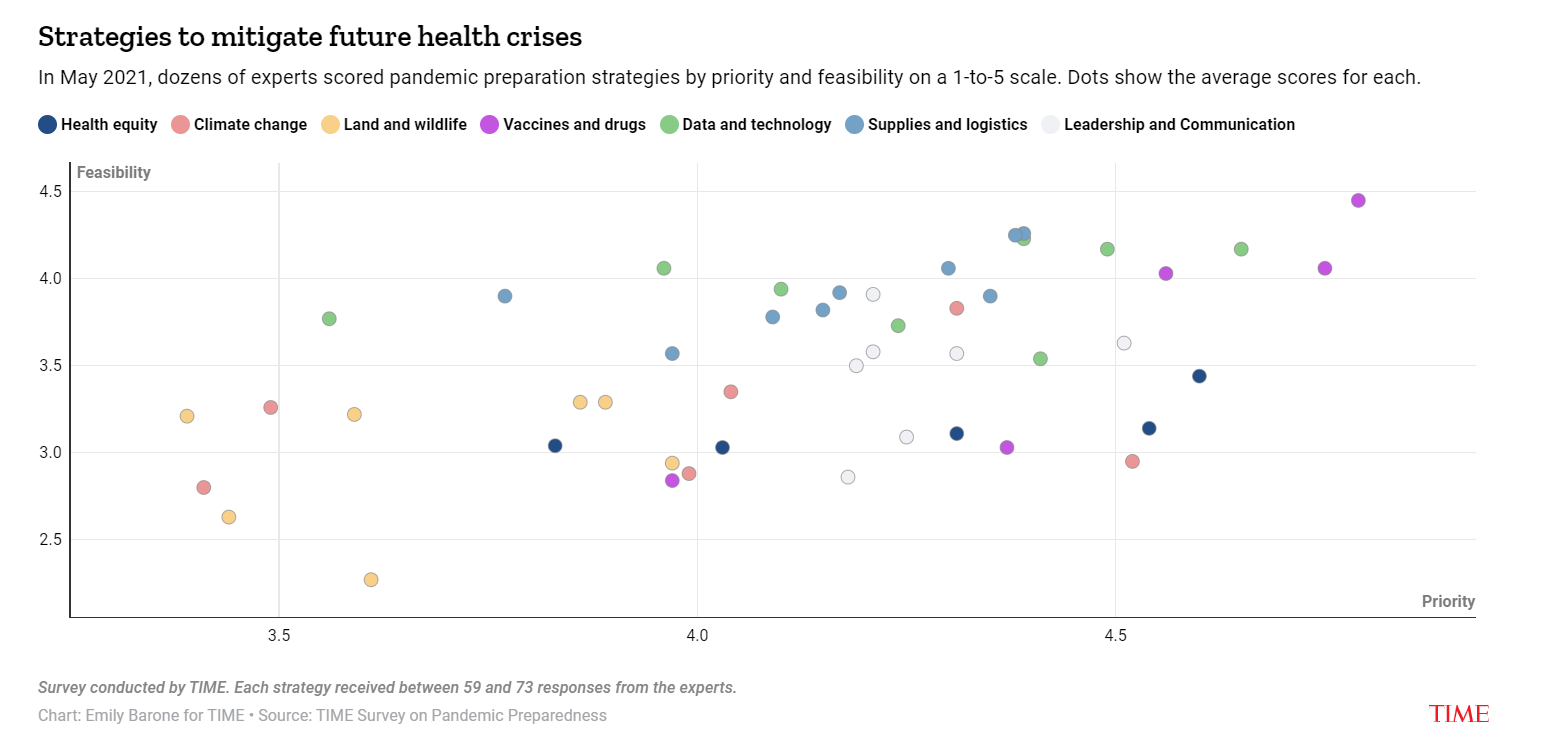
-
Vaccines and drugs
-
Data and technology
-
Supplies and logistics
-
Leadership and communication
-
Health equity
-
Land and wildlife
-
Climate change
The responses offer a blueprint for a more prepared world. At the top of the list was bolstering vaccine research and manufacturing — rated by experts as the most urgent and highest-impact initiatives. Improving systems that track and alert the world to new diseases also scored high. What’s more, these proposals also produced high feasibility scores, meaning experts saw either few barriers to implementation or strong momentum to overcome the challenges.
Other initiatives look tougher to accomplish. Ranked as high priority but less feasible were expanding health care access, distributing vaccines fairly and other strategies addressing inequalities that have exacerbated COVID-19’s toll on vulnerable populations.
Leadership and communication strategies were ranked as fairly high priority and moderately feasible, while on the other end of the spectrum, land-use and live-animal-trade strategies were deemed not very effective and also not very likely to happen.
The above chart shows the average rating for each strategy but does not in every case indicate consensus. A number of the strategies received both high and low scores. Some of those differences surely follow from differences in the disciplines the experts range across.
To capture that essential context, five health leaders previously recognized as TIME100 influencers analyzed the most significant findings in the links below.
The points they make not only underscore what we already know — that we could have managed COVID-19 better — but also where to look for the right answers.
Originally published at time












