the health transformation
institute for continuous health transformation
Joaquim Cardoso MSc
Founder and Chief Researcher & Editor
December 23, 2022
Executive Summary
Overview:
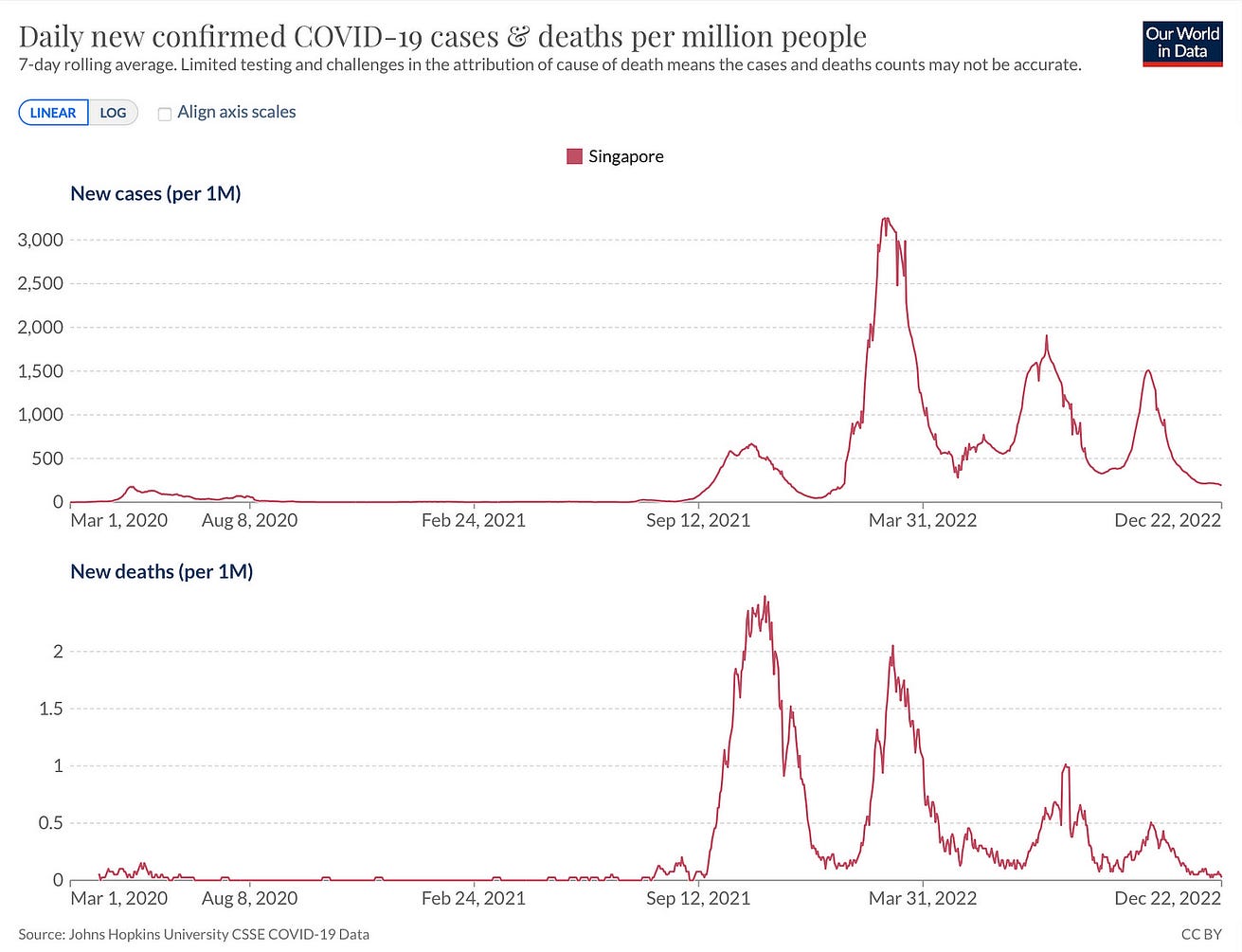
- The United States is the first country to have a XBB.x (subvariant) become dominant regionally following Singapore’s XBB. Singapore had a significant wave in October as shown here for cases and deaths.
- Fortunately, there was some uncoupling of the case-to-death ratio from its previous waves. It should also be noted that Singapore has one of the highest vaccination and booster rates in the world (compared with the United States below).
- New York is the bellwether for what is happening with XBB.1.5 and it doesn’t look good with a marked rise in hospitalizations, especially among seniors, in recent weeks as this variant has been taking hold.
- Of course, other factors are likely contributing such as waning of immunity, indoor/holiday gatherings, cold weather, lack of mitigation.
- But it is noteworthy that New York’s Covid hospital admission rate is the highest since late January (and also exceeds the summer 2021 Delta wave, but with some ambiguity as to how hospitalization were categorized then and now).
So we don’t know for sure how much of this is being driven by XBB.1.5, but it doesn’t look favorable.
- It is at the very least contributing-too much of a coincidence to see such a striking rise of the variant along with New York’s data.
- But only time will tell in the weeks ahead in contiguous states with XBB dominance how this will play out.
What can be done about it?
- This week in NEJM, the Emory group published the data on the bivalent BA.5 booster and how it helped against XBB:
- “Persons who received the BA.5-containing bivalent booster had better neutralizing activity against all Omicron subvariants (especially against BA.2.75.2, BQ.1.1 and XBB) than those who received 1 or 2 monovalent [original] boosters.”
- This finding of some cross-immunity protection has been backed up by live virus lab studies by 3 other groups.
- Although we don’t know how well the bivalent booster does against XBB.1.5 yet, there’s no reason to think it would not be helpful added antibody protection compared with not getting the booster.
What are the recommendations
- So if you haven’t had a booster in the past 4+ months, this would be well advised.
- Other than the bivalent booster, it’s the usual stuff of high quality masks, ventilation, air filtration, testing, etc.
- As the editorial in Nature published today was titled: “There is no room for COVID complacency in 2023.”
So if you haven’t had a booster in the past 4+ months, this would be well advised. Other than the bivalent booster, it’s the usual stuff of high quality masks, ventilation, air filtration, testing, etc.
ORIGINAL PUBLICATION
A new variant alert — The XBB.1.5 variant is on a growth spurt in the United States
Eric Topol
December 23, 2022
As everyone who has been following the Omicron family of SARS-CoV-2 descendants in recent months, there are a swarm of new subvariants.
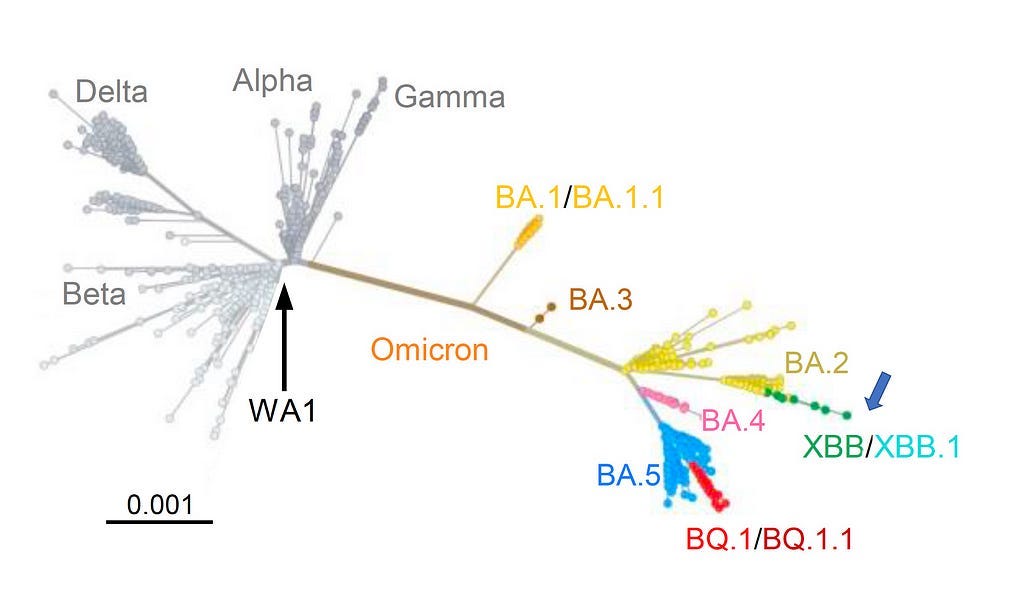
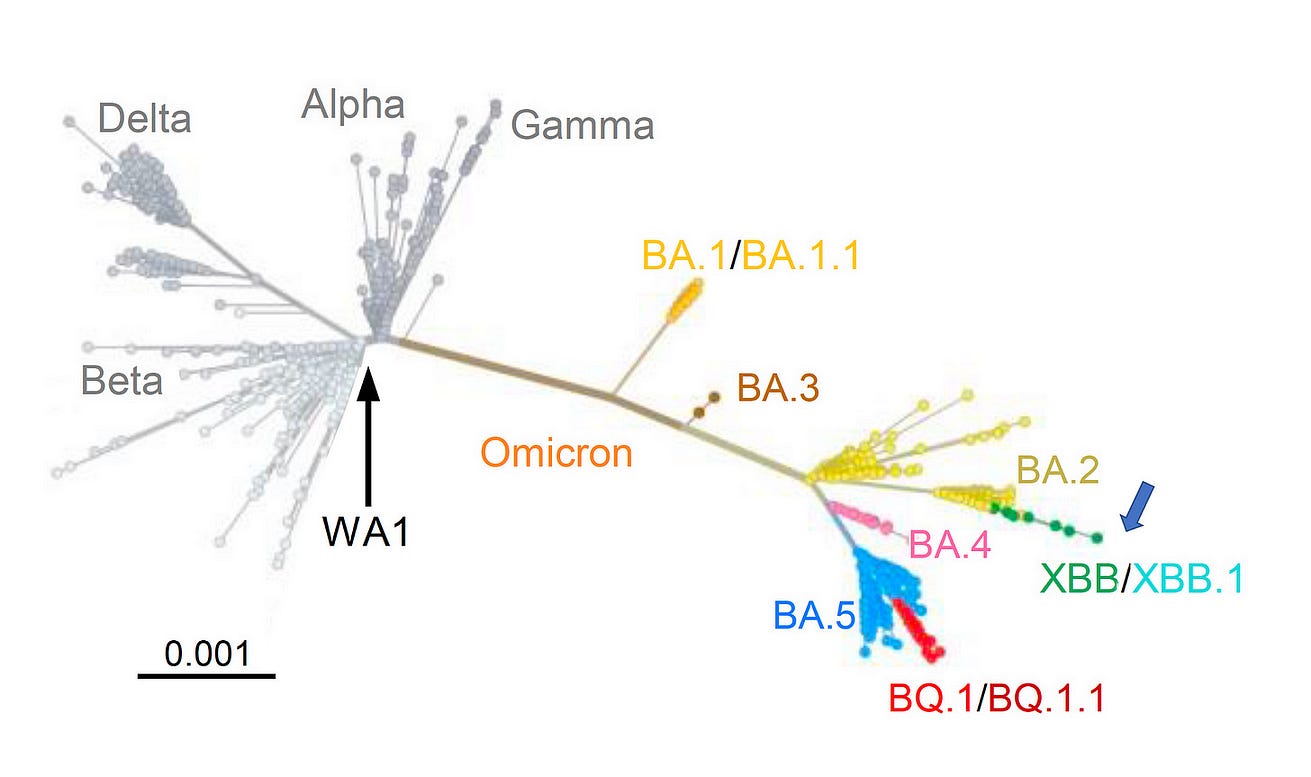
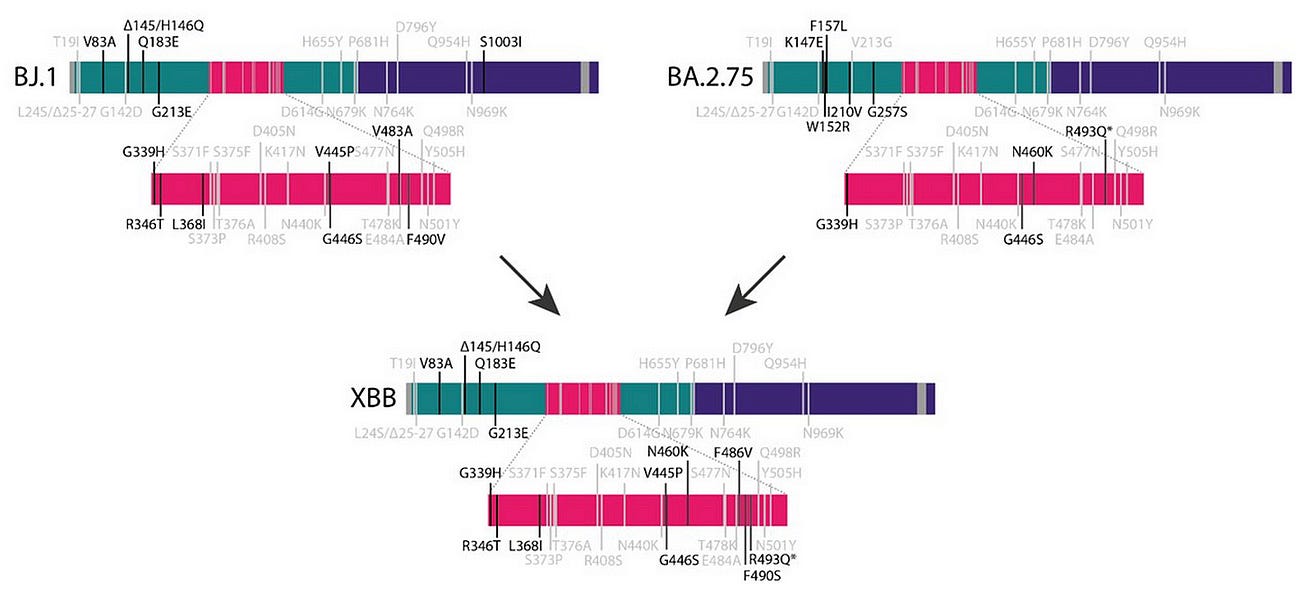
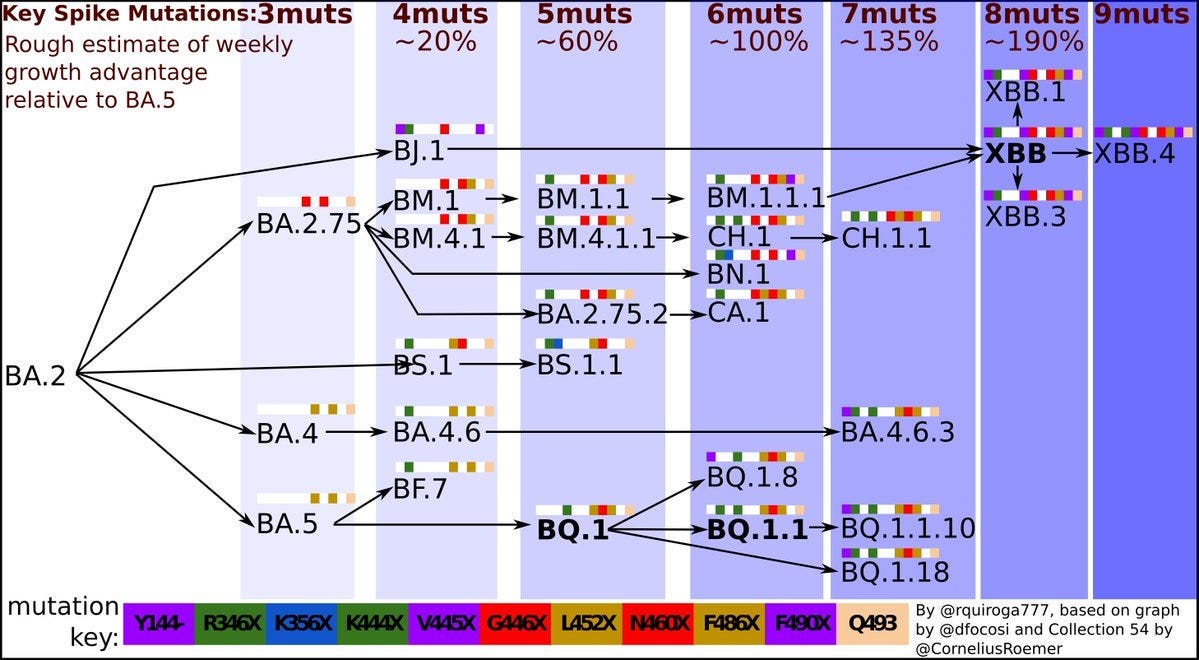
One of these is XBB, which is a recombinant (fusion) of 2 different BA.2 variants, BJ.1 (BA.2.10.1.1) and BA.2.75, depicted below by both the tree and mutation map.
Now that is playing out in New York and the Northeast regions of the United States.
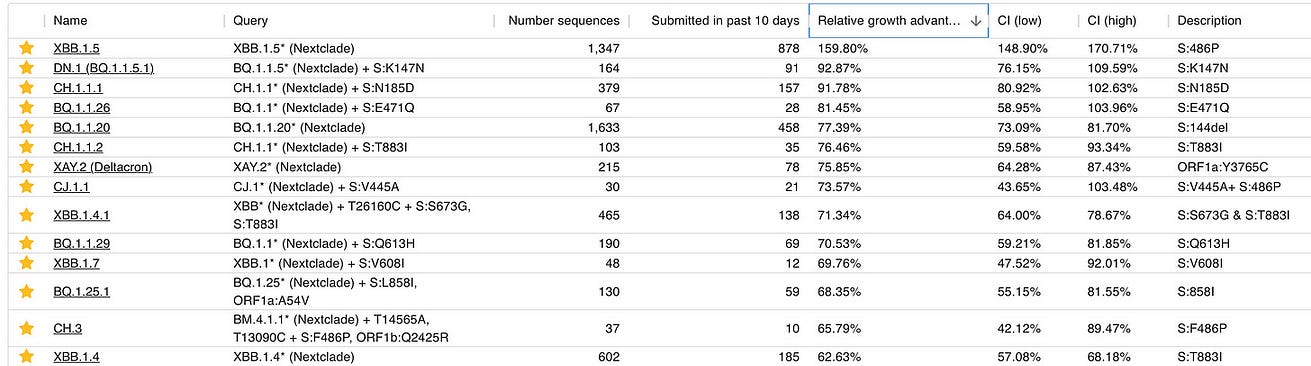
Of all the variants in the current mix, XBB.1.5 has the most growth advantage vs. BA.5 with substantial dropdown for the others as seen in the Cov-spectrum Table below, and a large number of sequenced samples to narrow the confidence intervals (CI).
Here is the most updated variant mix in New York through December 17th showing the rise of XBB.
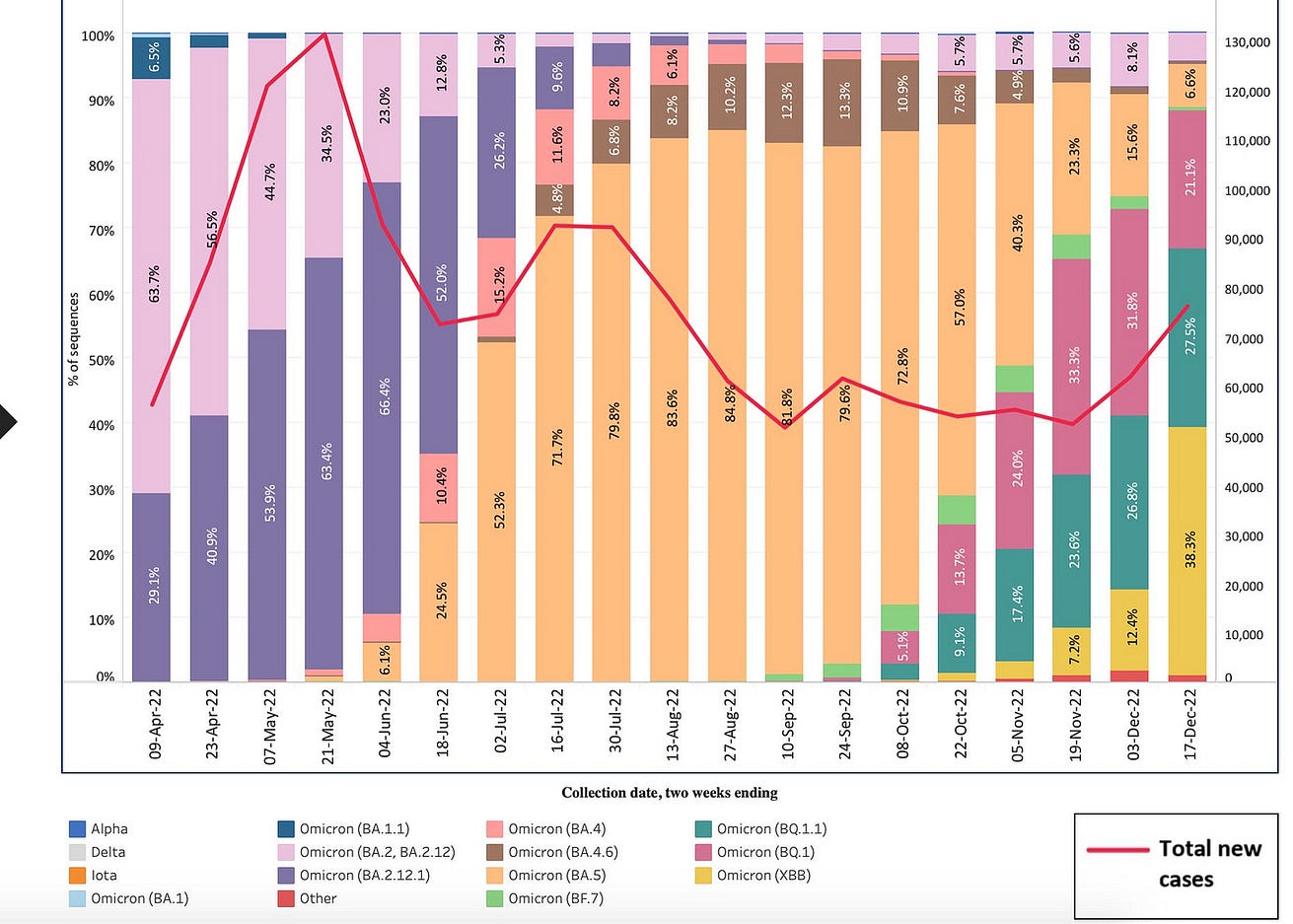
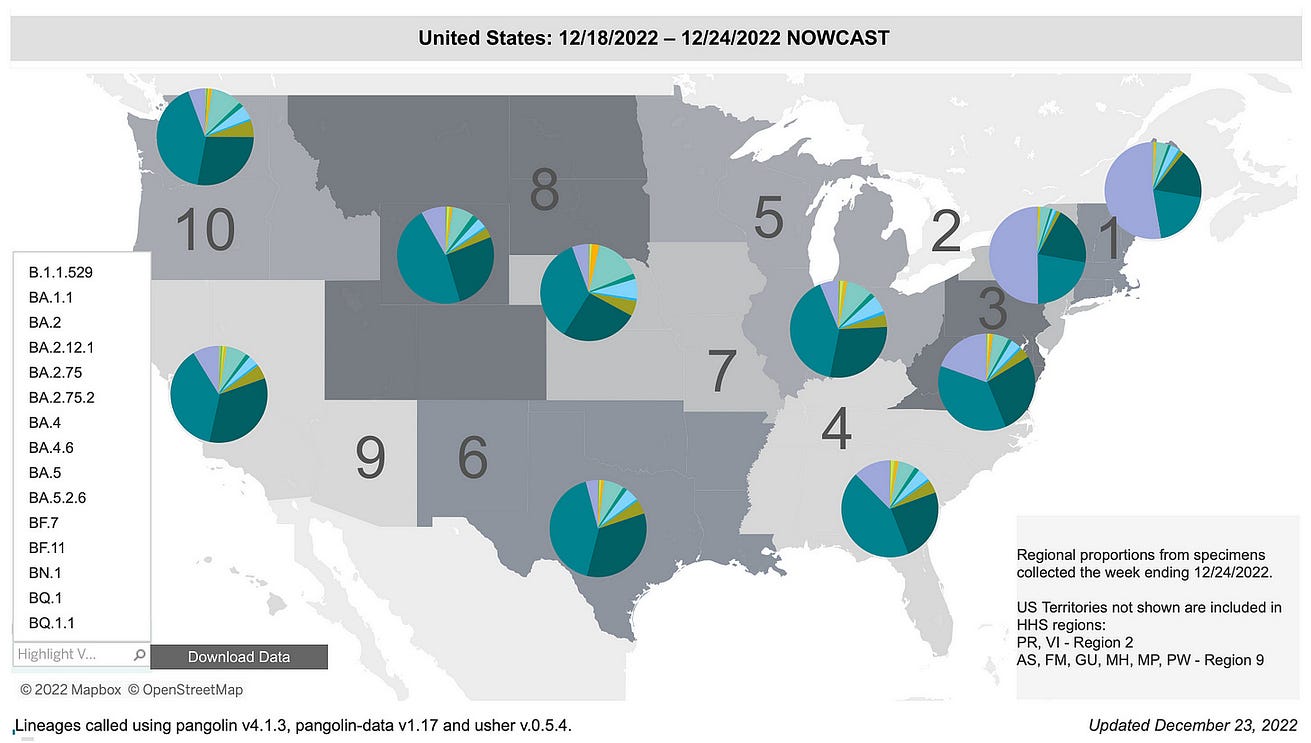
In the new CDC genomic surveillance, you can see the rise of XBB that has now stunted BQ.1’s growth pattern. That is to say that BQ.1’s dominance is static while XBB is on the move.
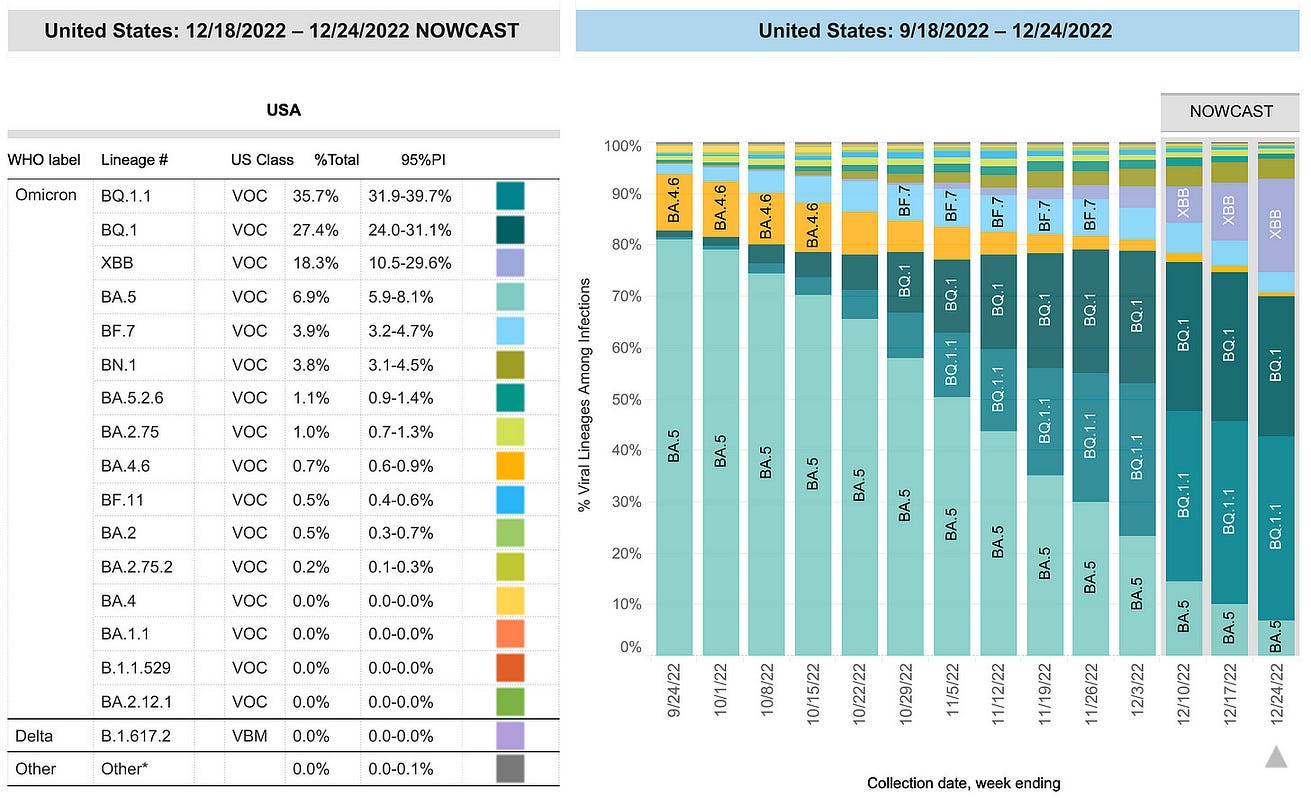
You can see this better in the Northeast regions where XBB has already become dominant (>50%), a jump from ~35% last week.
While we don’t have the sequence data to say it is the XBB.1.5 variant specifically, all indications would suggest that is indeed leading the pack within the XBBs.
If XBB.1.5 has such rapid growth advantage over BQ.1.1, that isn’t a good sign.
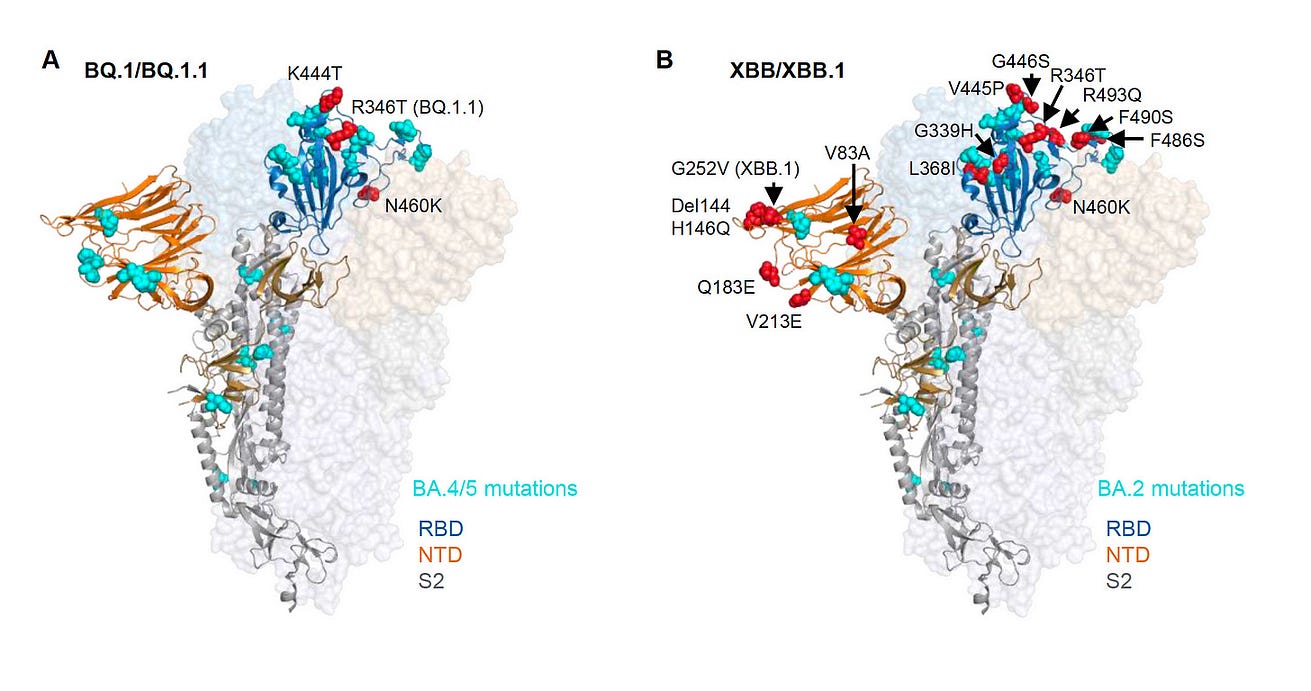
Last week, David Ho’s lab at Columbia University published a paper in Cell entitled “Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants.”
We had known from Yunlong Cao’s lab that XBB and BQ.1.1 were among the most immune evasive variants seen to date, but this new paper established that the immune evasion for XBB.1 is more than BQ.1.1 (and XBB.1.5 hasn’t yet been characterized, likely more than XBB.1).
We had known from Yunlong Cao’s lab that XBB and BQ.1.1 were among the most immune evasive variants seen to date, but this new paper established that the immune evasion for XBB.1 is more than BQ.1.1 (and XBB.1.5 hasn’t yet been characterized, likely more than XBB.1).
This XBB.1.5 variant is yet another stepwise mutations (now 9) from BA.2 with the fusion as noted above, and well seen in this Figure by Rodrigo Quiroga (@rquiroga777), akin to XBB.4
What does all this mean?
The United States is the first country to have a XBB.x (subvariant) become dominant regionally following Singapore’s XBB.
Singapore had a significant wave in October as shown here for cases and deaths.
Fortunately, there was some uncoupling of the case-to-death ratio from its previous waves. It should also be noted that Singapore has one of the highest vaccination and booster rates in the world (compared with the United States below).
New York is the bellwether for what is happening with XBB.1.5 and it doesn’t look good with a marked rise in hospitalizations, especially among seniors, in recent weeks as this variant has been taking hold.
Of course, other factors are likely contributing such as waning of immunity, indoor/holiday gatherings, cold weather, lack of mitigation.
But it is noteworthy that New York’s Covid hospital admission rate is the highest since late January (and also exceeds the summer 2021 Delta wave, but with some ambiguity as to how hospitalization were categorized then and now).
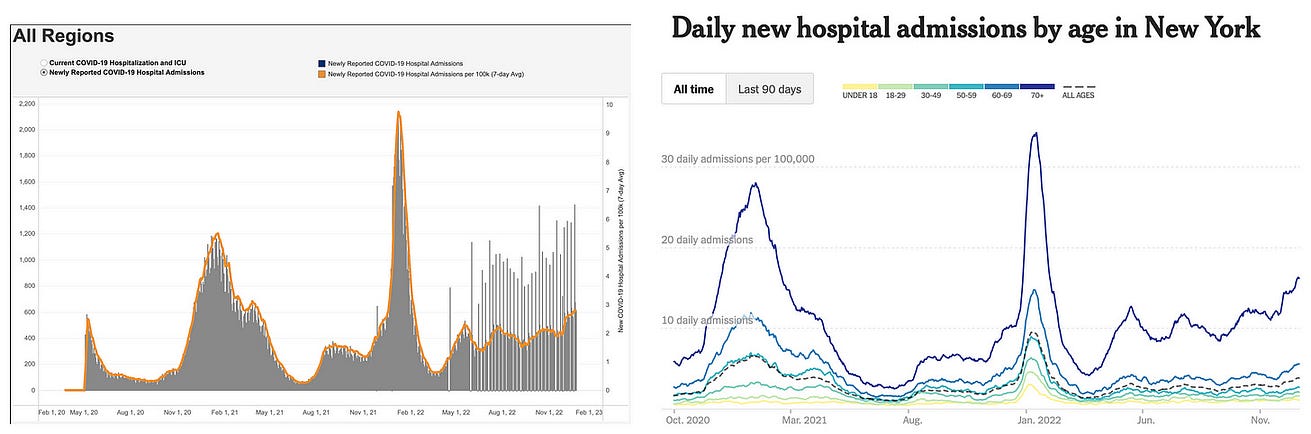
So we don’t know for sure how much of this is being driven by XBB.1.5, but it doesn’t look favorable.
It is at the very least contributing-too much of a coincidence to see such a striking rise of the variant along with New York’s data.
But only time will tell in the weeks ahead in contiguous states with XBB dominance how this will play out.
What can be done about it?
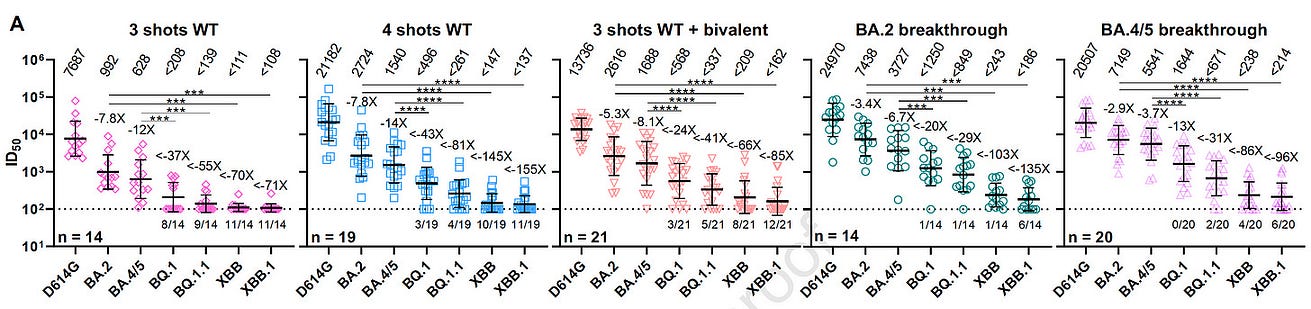
This week in NEJM, the Emory group published the data on the bivalent BA.5 booster and how it helped against XBB:
“Persons who received the BA.5-containing bivalent booster had better neutralizing activity against all Omicron subvariants (especially against BA.2.75.2, BQ.1.1 and XBB) than those who received 1 or 2 monovalent [original] boosters.”
“Persons who received the BA.5-containing bivalent booster had better neutralizing activity against all Omicron subvariants (especially against BA.2.75.2, BQ.1.1 and XBB) than those who received 1 or 2 monovalent [original] boosters.”
This finding of some cross-immunity protection has been backed up by live virus lab studies by 3 other groups.
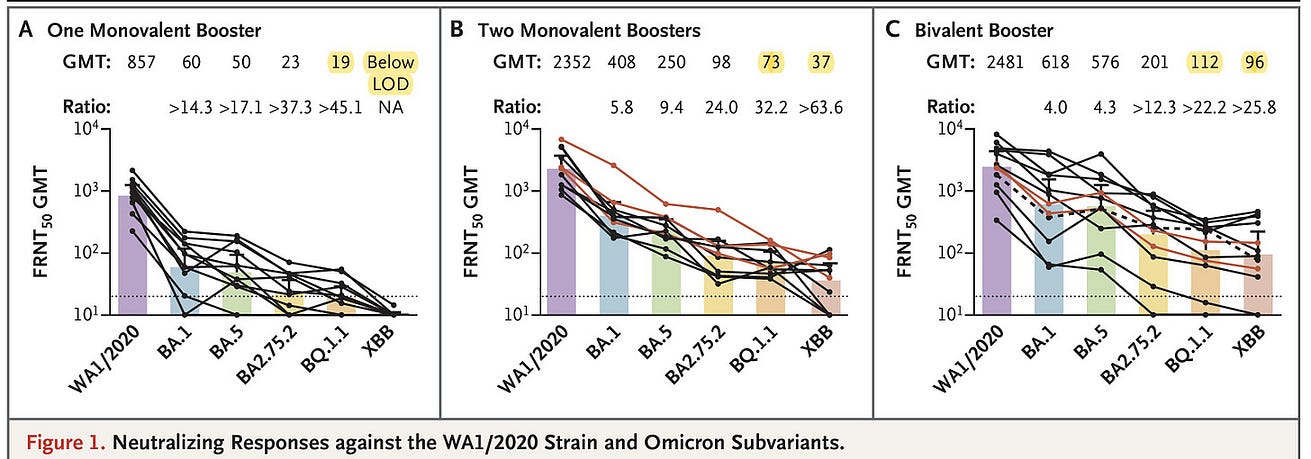
Although we don’t know how well the bivalent booster does against XBB.1.5 yet, there’s no reason to think it would not be helpful added antibody protection compared with not getting the booster.
So if you haven’t had a booster in the past 4+ months, this would be well advised. Other than the bivalent booster, it’s the usual stuff of high quality masks, ventilation, air filtration, testing, etc.
So if you haven’t had a booster in the past 4+ months, this would be well advised. Other than the bivalent booster, it’s the usual stuff of high quality masks, ventilation, air filtration, testing, etc.
XBB.1.5 is not a welcome addition to the holiday season, to say the least.
The purpose of this post is to raise awareness of its existence and trajectory, and to keep your guard up.
As the editorial in Nature published today was titled: “There is no room for COVID complacency in 2023.”
The purpose of this post is to raise awareness of its existence and trajectory, and to keep your guard up.
As the editorial in Nature published today was titled: “There is no room for COVID complacency in 2023.”
While there’s still much to learn about this variant, it doesn’t have the look of a “scariant” (a term I coined in the pandemic for variants that have no functional significance but scare us).
I hope you find this information and perspective is helpful.
Wishing you and yours a happy holiday season and the best for 2023
Originally published at https://erictopol.substack.com on December 23, 2022.
Names mentioned
Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants
Qian Wang, Sho Iketani, Zhiteng Li, Liyuan Liu, Yicheng Guo, Yiming Huang, Anthony D. Bowen, Michael Liu, Maple Wang, Jian Yu, Riccardo Valdez, Adam S. Lauring, Zizhang Sheng, Harris H. Wang, Aubree Gordon, Lihong Liu, David D. Ho
Imprinted SARS-CoV-2 humoral immunity induces convergent Omicron RBD evolution
Yunlong Cao, Fanchong Jian, Jing Wang, Yuanling Yu, Weiliang Song, Ayijiang Yisimayi, Jing Wang, Ran An, Xiaosu Chen, Na Zhang, Yao Wang, Peng Wang, Lijuan Zhao, Haiyan Sun, Lingling Yu, Sijie Yang, Xiao Niu, Tianhe Xiao, Qingqing Gu, Fei Shao, Xiaohua Hao, Yanli Xu, Ronghua Jin, Zhongyang Shen, Youchun Wang & Xiaoliang Sunney Xie
Neutralization against BA.2.75.2, BQ.1.1, and XBB from mRNA Bivalent Booster
Meredith E. Davis‑Gardner, Ph.D.
Lilin Lai, M.D.
Bushra Wali, Ph.D.
Hady Samaha, M.D.
Emory University School of Medicine
Atlanta, GA
Daniel Solis, B.S.
Stanford University School of Medicine Stanford,
CA Matthew Lee, M.S.
Andrea Porter‑Morrison, B.S.
Ian T. Hentenaar, M.S.
Emory University School of Medicine Atlanta, GA
Fumiko Yamamoto, Ph.D.
Stanford University School of Medicine Stanford, CA
Sucheta Godbole, M.S.
National Institute of Allergy and Infectious Diseases Bethesda, MD
Yuan Liu, Ph.D.
Emory University School of Medicine Atlanta, GA
Daniel C. Douek, M.D., Ph.D.
National Institute of Allergy and Infectious Diseases Bethesda, MD
Frances Eun‑Hyung Lee, M.D. Nadine Rouphael, M.D. Alberto Moreno, M.D.
Emory University School of Medicine Atlanta, GA








