HealthSystems — transformation institute
for continuous health transformation
Joaquim Cardoso MSc
Chief Researcher, Editor and Strategy Officer (CSO)
November 15, 2022
Source: BMJ Open
Executive Summary:
Objectives
- We aimed to systematically map the extent, range and nature of research activity on value-based healthcare (VBHC), and to identify research gaps.
Design
- A scoping review with an additional cited reference search was conducted, guided by the Joanna Briggs Institute methodology.
Data sources
- The search was undertaken in PubMed, Embase and Web of Science.
Eligibility criteria
- Eligible articles mentioned VBHC or value with reference to the work of Porter or provided a definition of VBHC or value.
Data extraction and synthesis
- Data were independently extracted using a data extraction form. Two independent reviewers double extracted data from 10% of the articles.
- Data of the remaining articles (90%) were extracted by one reviewer and checked by a second.
- The strategic agenda of Porter and Lee was used to categorise the included articles.
Results
- The searches yielded a total of 27,931 articles, of which 1,242 were analysed.
- Most articles were published in North America.
- Most articles described an application of VBHC by measuring outcomes and costs (agenda item 2).
- The other agenda items were far less frequently described or implemented.
- Most of these articles were conceptual, meaning that nothing was actually changed or implemented.
Four main observations on these results are highlighted:
- First, research on VBHC focused primarily on the agenda item ‘measuring outcomes and costs’.
- Second, the current strategic agenda seemed to be incomplete.
- Third, there was a scarcity of articles on implementation of agenda items.
- Finally, it was striking that many of the included articles were focused on surgical specialties.
Conclusion
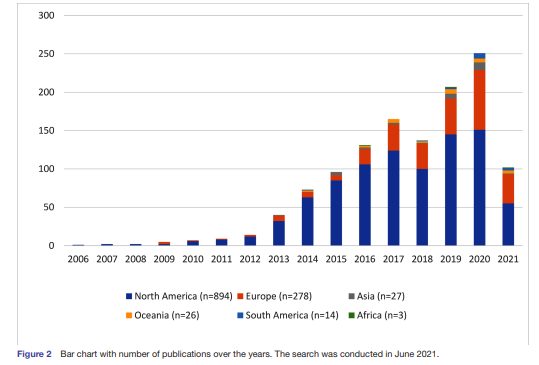
- The number of publications increased steadily after the introduction of VBHC in 2006.
- Almost one-fifth of the articles could not be categorised in one of the items of the strategic agenda, which may lead to the conclusion that the current strategic agenda could be extended.
- In addition, a practical roadmap or guideline to implement VBHC is still lacking.
- Future research could fill this gap by specifically studying the effectiveness of VBHC in day-to-day clinical practice.
Implications for clinical practice and/or research
- With the exception of measuring outcomes and costs, few articles have implemented and researched the implementation of strategic agenda items.
- There is a need for studies that evaluate the implementation of the different strategic agenda items within different medical specialties.
- Insight in practical implementation is needed in order to work towards a roadmap for step-by-step implementation of VBHC.
- It is important to collect evidence from daily practice to serve the evidence-based paradigm of the healthcare sector.
Infographic
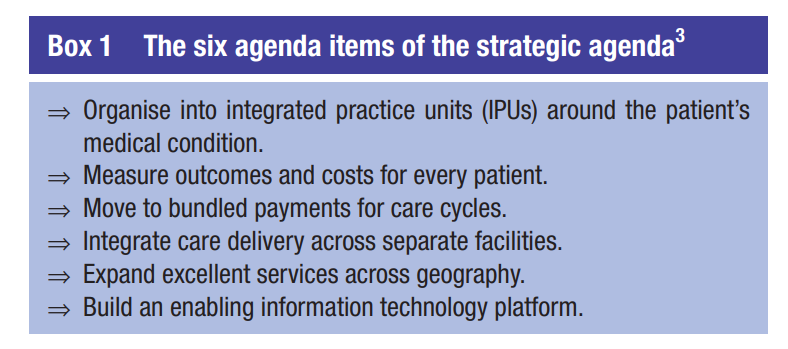
Figure 2 — Bar chart with number of publications over the years. The search was conducted in June 2021
ORIGINAL PUBLICATION (excerpt version)
Mapping the extent, range and nature of research activity on value-based healthcare in the 15 years following its introduction (2006–2021): a scoping review
BMJ Open
Joanna R G Vijverberg ,1,2 Kirsten Daniels ,2,3 Gijs Steinmann ,4 Mirjam M Garvelink,2 Marc B V Rouppe van der Voort,5 Douwe Biesma,6 Willem Jan W Bos,6,7 Frits van Merode ,1 Paul van der Nat2,3
27 July 2022
Introduction
In 2006, value-based healthcare (VBHC) was introduced in the USA as a way to reform healthcare.1
Rising costs, mounting quality issues and an increasing healthcare demand prompted the development of the VBHC concept by Porter and Teisberg.1
According to them, improving value for the patient should be the overarching goal in healthcare.
In healthcare, there are different approaches of defining and measuring value.
In VBHC, value is defined as the health outcomes achieved per dollar spent.1
To improve patient value, healthcare delivery should be organised around medical conditions over the full cycle of care. Universal measurement of value (outcomes and costs) is an important element in monitoring improvement.2
In VBHC, value is defined as the health outcomes achieved per dollar spent.1
To improve patient value, healthcare delivery should be organised around medical conditions over the full cycle of care. Universal measurement of value (outcomes and costs) is an important element in monitoring improvement.2

Strategic agenda for value transformation
In 2013, a strategic agenda was published, consisting of six agenda items for implementing a high-value healthcare delivery system ( box 1). 3
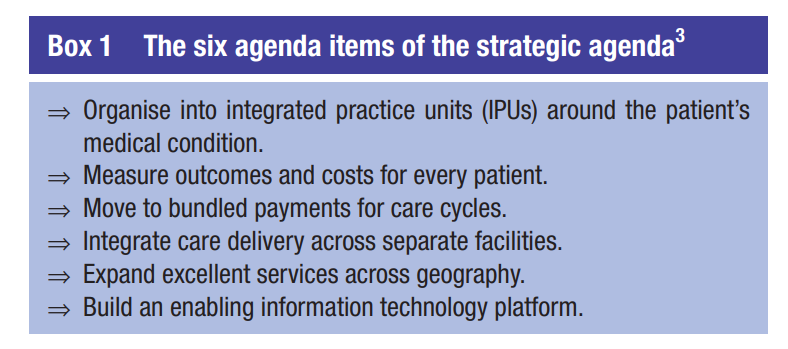
The agenda items were intended to support healthcare providers in the transition from a focus on volume, that is, being organised around functionally organised departments and specialties, to a focus on value, that is, being organised around what matters to patients with a specific medical condition.
Implementation of VBHC
The implementation of VBHC requires a major transition at both the level of healthcare providers as well as at the level of (national) healthcare systems.
Healthcare providers, such as hospitals, are typically (vertically) organised around functional departments and specialties.
Transitioning towards an organisation that is based on medical condition (horizontal) (agenda item 1) requires a fundamental reorganisation of hospitals and their collaborating care chain partners (agenda item 4).
Measuring outcomes over the full cycle of care for a certain medical condition (agenda item 2) also requires further major change.
When VBHC was introduced in 2006, healthcare quality systems were aimed at monitoring providers’ compliance to (international) quality guidelines and norms.
At the time, quality indicators were primarily focused on process optimisation and safety.
Health outcomes were hardly available and not measured at the level of medical conditions.
Moreover, costs should be measured over the full cycle of care taking the true costs of care delivery into account.
This requires a different approach for most healthcare providers (agenda item 2).
The reimbursement of healthcare providers should move to payment for value, which requires major changes for healthcare providers, and for health insurance companies and healthcare industry, such as pharmaceutical companies (agenda item 3).
The expansion of excellent care across geography (agenda item 5) is challenging, because it arises from the progress on the other agenda items.
Finally, building an enabling information technology (IT) platform (agenda item 6) is essential for the value transition.
The availability of high-quality data and IT infrastructure is named one of the main cornerstones to move forward with VBHC. 4

The maturity of VBHC
VBHC has become a popular vision for healthcare organisations.
Since the introduction of VBHC in the USA, the concept has spread around the world, and an increasing number of healthcare providers are adopting VBHC principles in order to continuously improve care.
The article ‘What is value in health care?’ 5 has since been cited over 4500 times. 6
However, few details have been published on how to practically implement VBHC.
The strategic agenda proposed the major themes that need to be addressed in healthcare, but how to actually implement these items is hardly described.
VBHC has been introduced as a strong vision for healthcare, but a practical guideline or scientific proof for the success of the proposed strategic agenda is lacking.
As a result, various aspects of VBHC are only superficially understood and interpreted in different ways. 7
Scientific output on VBHC is important since the healthcare sector, perhaps more than in economics or management, uses an evidence-based paradigm.
Healthcare professionals are used to consider the scientific evidence before implementing an organisational reform such as VBHC.
In order to support organisations in the implementation of VBHC, it is important to understand how the VBHC concept and strategic agenda have been used in different contexts and have evolved over time.
Therefore, the aim of this scoping review was to systematically map the extent, range and nature of research activity on VBHC over the last 15 years, and to identify potential research gaps.
As this is a scoping review, the quality of the included articles was not assessed.
Methods and other Sections
See the original publication (this is an excerpt version only)
Review findings
Main findings
This review showed that the extent, range and nature of VBHC research are large and still increasing; over the last 15 years more than 1200 articles reported on VBHC.
They described (the implementation of) the strategic agenda items within various specialties.
The number of published articles increased each year, especially since 2013, with the exception of 2018.
Most articles were published in the USA/North America, followed by Europe.
The majority of articles described the measurement of outcomes and costs. Other agenda items were far less frequently described or implemented.
Most of the articles were conceptual, meaning that nothing was actually changed or implemented.
When looking at the role that VBHC played in the articles, almost half of the articles discussed or implemented one or more agenda items; only five articles described or implemented all agenda items.
Most articles were published from surgical specialties.
When looking at the role that VBHC played in the articles, almost half of the articles discussed or implemented one or more agenda items; only five articles described or implemented all agenda items.
Four main observations on these results are highlighted in the following paragraphs.
- First, research on VBHC focused primarily on the agenda item ‘measuring outcomes and costs’.
- Second, the current strategic agenda seemed to be incomplete.
- Third, there was a scarcity of articles on implementation of agenda items.
- Finally, it was striking that many of the included articles were focused on surgical specialties.
First, research on VBHC focused primarily on the agenda item ‘measuring outcomes and costs’.
Furthermore, this agenda item had a relatively high ratio (52%) of application articles, meaning that outcomes and costs were actually measured.
All other agenda items were reported on in a more conceptual way, without actually implementing or applying anything.
The predominant focus on outcomes and costs might be explained by the formulation of the value definition, in which outcomes and costs are both specifically mentioned.
Furthermore, it seems relatively difficult to implement other agenda items such as bundled payments of IPUs without measuring outcomes and costs (value).
The importance of measuring outcomes and costs has also been recognised in other quality of care concepts such as the Donabedian model. 18
Another explanation for the popularity of measuring outcomes and costs could be the clarity of this agenda item; this item is the least susceptible to interpretation differences.
Additionally, Porter stated that measuring outcomes is the most import step and he dedicated a practical article on standard outcome sets, 5 which further facilitates the focus on measuring outcomes and costs.
The types of outcomes and costs that were measured differed between continents.
North America more often measured costs than Europe.
Moreover, in the USA, VBHC was often used in the context of healthcare funding laws that place emphasis on curbing cost growth such as the Affordable Care Act (ACA).
One of the goals of ACA was to expand healthcare coverage and to make healthcare affordable to more citizens. 19
This focus on costs and payment methods might explain the higher number of articles measuring costs in North America.
Second, the current strategic agenda seemed to be incomplete.
In 18% of the included articles, none of the current agenda items were discussed.
Based on the issues that were addressed in these articles, we proposed four new agenda items: ‘quality improvement’, ‘VBHC culture’, ‘shared decision making’ and ‘education’.
These four agenda items matched the new agenda items that were recently suggested. 20
It is important to note that some of the new agenda items, such as shared decision making, were discussed in many of the included articles.
However, in our methods, a new agenda item was only suggested by the reviewers when none of the current agenda items were checked in the data extraction form.
Thus, the number of articles with new agenda items was under-reported.
Third, there was a scarcity of articles on implementation of agenda items.
Only a quarter of the included articles described an implementation.
The majority of these articles focused on one agenda item. Few articles described implementation of multiple agenda items.
The lack of implementation articles was in line with other research in hospital settings; Reitblat et al concluded that the implementation and investigation of the strategic agenda in urology was limited 21 and another scoping review specifically focusing on VBHC implementation in hospital settings showed the same scarcity. 22
One reason for the lack of implementation articles might be the absence of a practical implementation guide for VBHC.
The need for a roadmap that addresses the required steps for organisational changes has been acknowledged before. 10
Currently, this roadmap with practical steps is still missing and the available VBHC theory is interpreted in various ways. 23
This could lead to an inadequate implementation, as an ill-defined management intervention is often implemented in different ways. 24
Furthermore, it was argued that a low level of understanding might result in a dilution of the concept. 7
Therefore, it seems especially important to describe and observe different implementation initiatives around the world to ultimately create a guideline for each healthcare context.
Finally, it was striking that many of the included articles were focused on surgical specialties.
A possible explanation is that these specialties have a longer history of quality registries (including outcome measures) and generally perform intervention-driven studies.
Intervention-driven studies often compare health outcomes between interventions or patient groups.
As a result, surgical articles focused more on health outcomes and linked this to the VBHC concept and the definition of value; outcomes compared with costs.
Another reason could be that VBHC principles are easier to implement in surgery as there is a more direct relation between intervention and outcomes.

Strengths and limitations
Some limitations need to be considered when interpreting the results of this study.
First, the search strategy did not specifically include search terms for each agenda item, which could have resulted in selection bias.
Second, using the article ‘What is value in health care?’ 5 for the cited reference search might have resulted in the over-representation of articles focusing on measuring value, outcomes or costs. However, the representation of ‘What is value in health care’ and other references to Porter found in our study is similar to the representation found in PubMed.
Third, the focus of this study was on scientific peer-reviewed articles. As a result, VBHC implementation initiatives published in ‘gray literature’ or published as non-peer-reviewed articles have not been included in this study. This might have led to an under-representation of the actual number of VBHC implementations in practice.
Finally, inherent to the design of a scoping review, the included articles were not assessed for their research quality.
A major strength of this review is its broad scope.
The present study provides a comprehensive overview including items such as medical specialties, countries and all strategic agenda items (including potential new ones) ( online supplemental file 2).
In addition, the study’s exclusion criteria deliberately generated a broad picture of the current state of research on VBHC.
This has resulted in a complete picture of the current state of research on VBHC. The broad scope of this study was especially important in light of the different interpretations of the VBHC concept.
Finally, to date, hardly any reviews on VBHC have been published, and existing reviews focusing on, for example, articles with an implementation of VBHC. 22

Implications for clinical practice and/or research
With the exception of measuring outcomes and costs, few articles have implemented and researched the implementation of strategic agenda items.
There is a need for studies that evaluate the implementation of the different strategic agenda items within different medical specialties.
Insight in practical implementation is needed in order to work towards a roadmap for step-by-step implementation of VBHC.
It is important to collect evidence from daily practice to serve the evidence-based paradigm of the healthcare sector.
To contribute to more evidence, our database ( online supplemental file 2) can be used for in-depth systematic reviews to further explore what is known within each of the agenda items.
Originally published at https://bmjopen.bmj.com on August 1, 2022.
About the authors & affiliations
Joanna R G Vijverberg ,1,2 Kirsten Daniels ,2,3 Gijs Steinmann ,4 Mirjam M Garvelink,2 Marc B V Rouppe van der Voort,5 Douwe Biesma,6 Willem Jan W Bos,6,7 Frits van Merode ,1 Paul van der Nat2,3
1 Department of Health Services Research, Maastricht University Medical Centre+, Maastricht, Netherlands
2 Department of Value-Based Healthcare, Sint Antonius Hospital, Nieuwegein, Netherlands
3 Scientific Center for Quality of Healthcare (IQ healthcare), Radboud Institute for Health Sciences, Radboudumc, Nijmegen, Netherlands
4 Health Care Governance, Erasmus School of Health Policy and Management, Erasmus Universiteit, Rotterdam, Netherlands
5 Department of Juiste zorg, Juiste plaats, Juiste kosten, Sint Antonius Hospital, Nieuwegein, Netherlands
6 Department of Internal Medicine, Leiden University Medical Center, Leiden, Netherlands
7 Department of Internal Medicine, Sint Antonius Hospital, Nieuwegein, Netherlands