the health strategist
research & strategy institute
Joaquim Cardoso MSc.
Chief Research Officer (CSO), Chief Editor
Chief Strategy Officer (CSO) and Senior Advisor
August 9, 2023
What is the message?
To reduce carbon emissions, heath systems should focus on redesigning delivery systems and investing in prevention efforts.
Health care service redesign can improve patient outcomes and reduce costs and carbon emissions.
Key takeaways:
Climate change events, such as rising temperatures, floods, hurricanes, and wildfires, are not only impacting the environment but also posing significant threats to human health and mental well-being.
- Vulnerable communities are often disproportionately affected by these challenges. This summary, published by The Commonwealth Fund, highlights the intersection of climate change, healthcare emissions, and the imperative to reduce carbon footprints within the healthcare sector.
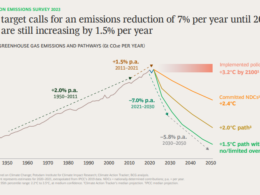
The healthcare industry, while essential for preserving and improving health, is also a notable contributor to global emissions. Emissions generated by healthcare account for up to 4.6 percent of global emissions, with the U.S. healthcare sector’s contribution being notably higher at around 8.5 percent.
Without proactive measures, projections indicate that global healthcare emissions could reach an alarming six gigatons annually by 2050, equivalent to emissions produced by approximately 1.26 billion cars.
- Efforts to mitigate emissions have been primarily focused on sectors such as energy, transportation, waste management, food production, and pharmaceuticals, with support from financial incentives within the Inflation Reduction Act. However, achieving the critical goal of net-zero carbon emissions necessitates transformational changes in healthcare delivery, supply chains, and research and innovation.
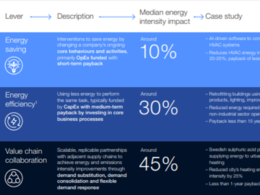
To effectively reduce emissions, healthcare systems can adopt a multifaceted approach:
- Redesigning Care Delivery for Sustainability: The redesign of healthcare services holds the potential to enhance patient outcomes, control costs, and reduce carbon emissions. Shifting care closer to homes in primary care or community settings can lessen the burden on energy-intensive hospital facilities.
- Leveraging Telehealth and Digital Tools: Expanding the use of telehealth and digital solutions empowers patients to access services conveniently, mitigating emissions from travel. Remote monitoring tools enhance continuity of care and early detection, reducing the need for carbon-intensive interventions.
- Prioritizing Lower-Emission Treatments: Embracing lower-emission treatment options that yield equivalent outcomes is vital. While innovative procedures like robot-assisted surgery can offer benefits, their environmental impact should be carefully evaluated.
- Curbing Overtreatment and Unnecessary Care: Addressing overtreatment and unnecessary care reduces waste and excess carbon emissions. In the U.S., substantial savings can be realized by curbing overtreatment, resulting in a more sustainable healthcare system.
- Empowering Prevention: Prevention initiatives, encompassing green space provision, increased physical activity, and healthier diets, not only promote public health but also generate substantial reductions in carbon emissions, air pollution, and toxic exposure.
Healthcare organizations can play a transformative role by acting as community “anchors.” By leveraging their resources and refining business practices, they can contribute to improved local health outcomes and sustainable environmental practices.
- The imperative to reduce carbon emissions and embrace environmental sustainability must be integrated into all aspects of healthcare service redesign. By doing so, healthcare systems can advance patient outcomes, control costs, and protect the environment.
An even broader approach entails a shift from reactive treatment models to proactive health and wellness support, fostering community investment in public health and prevention.
- For healthcare systems, prioritizing both human well-being and the planet’s health is a moral and strategic obligation. Through collaborative efforts, innovative solutions, and conscious decision-making, the healthcare sector can pave the way towards a healthier and more sustainable future for all.
DEEP DIVE
Lowering Carbon Emissions Through Redesigned Health Care
Emily Hough
August 8, 2023
Climate change events — rising temperatures, floods, hurricanes, wildfires — have an impact on health and mental health, with vulnerable communities often disproportionately affected. Emissions from health care account for as much as 4.6 percent of emissions globally, but the U.S. health care contribution is much higher, closer to 8.5 percent. Without action, there are predictions that global emissions from health care will reach six gigatons a year by 2050, equivalent to emissions from approximately 1.26 billion cars.
Ongoing efforts to reduce emissions in energy, transportation, waste, food, and some medicines are supported by financial incentives in the Inflation Reduction Act. But closing the gap to net-zero carbon emissions requires making changes in care delivery, the supply chain, and research and innovation.
Reducing Emissions Through Delivery System Reform
Redesigning health care can improve outcomes and reduce costs; there are now calls for redesign to help reduce carbon emissions. Strategies include:
- Providing care closer to home in primary care or community settings to deliver better patient outcomes and experiences, reduce the cost of care, and reduce emissions by shifting care from the most energy intensive buildings (i.e., hospitals).
- Increasing use of telehealth and digital tools can offer patients greater choice in how and when they access services and reduce emissions from travel. Digital tools for remote monitoring can improve continuity of care and provide early warning of deterioration, which can prevent future hospitalizations. NHS Virtual Wards, which use digital tools to provide remote monitoring for patients at home, have demonstrated a reduction in carbon emissions and cost savings.
- Shifting to lower-emission treatments that deliver the same outcomes. Emissions vary across treatments and procedures. Innovative technologies like robot-assisted surgery can improve outcomes for patients and reduce lengths of stay. However, they may also be carbon intensive. A 2015 life cycle assessment of four surgical approaches for hysterectomy (abdominal, vaginal, laparoscopic, and robotic) found the robot-assisted approach to have the largest environmental footprint and higher costs.
- Ensuring appropriate use of care by reducing overtreatment or unnecessary care. In the U.S., estimates suggest spending on Medicare overuse may be as high as 29 percent of total spending, with two out of three prescribed medications going unused. This waste costs the system more than $2.4 billion per year.
- Early detection and diagnosis can help lower emissions, reducing the need for more complex carbon-intensive care later. Effective secondary prevention and ongoing management of long-term conditions can also reduce emissions.
- Long term care management can reduce complications and therefore the need for future complex treatments and their associated emissions. For example, people with diabetes who manage their blood sugar levels through glucose-lowering treatment generate fewer emissions than those with untreated diabetes.
Reducing Emissions Through Prevention
Preventing the need for services in the first place delivers an even bigger reduction in emissions than service redesign. Public health and prevention initiatives — including provision of more green spaces, increasing physical activity, encouraging a healthier diet — reduce the burden from noncommunicable diseases and deliver additional climate benefits through reduced carbon emissions, air pollution, and toxic exposures.
Some health care organizations are contributing to these efforts and acting as “anchors” in their community by using their resources and managing their business practices in ways that contribute to improving local health outcomes.
Conclusion
Reducing carbon emissions and other environmental impacts should be considered as part of all health care service redesign, as a benefit alongside patient outcomes and cost factors. Health systems wanting to take further action to reduce their contributions to climate change may also wish to consider how they can not only redesign their care, but switch from a focus on treating sickness to supporting health and wellness, including increasing their investment in public health and prevention for local communities.
Click here to access a table with examples of shifting to lower-emissions treatments
The Author
Emily Hough is a 2021–22 U.K. Harkness Fellow in Health Care Policy and Practice. At the time of her fellowship, she was Director of the Acute Provider Alliance for the NHS in North East London, where she supported collaboration across three NHS Trusts working to improve quality and access to care, with a focus on COVID-19 recovery.
Hough previously spent three years as Director of Strategy at NHS England and NHS Improvement, where she led a strategy team helping to solve some of the most complex problems facing the English healthcare system.
Originally published at https://www.commonwealthfund.org/blog/2023