Air pollution from fine particulate matter caused 6.4 million premature deaths and 93 billion days lived with illness (2019).
This is an excerpt of the report below.
The Global Health Cost of PM2.5 Air Pollution : A Case for Action Beyond 2021
World Bank
Yewande Awe
Bjorn Larsen
Ernesto Sánchez-Triana
Santiago Enriquez
Shafick Hoossein
2021
Overview
CONFERENCE EDITION FOR PUBLICATION EXPECTED LATER IN 2021.
According to the Global Burden of Disease 2019 study, air pollution from fine particulate matter caused 6.4 million premature deaths and 93 billion days lived with illness in 2019.
Over the past decade, the toll of ambient air pollution has continued to rise. Air pollution’s significant health, social, and economic effects compel the World Bank to support client countries in addressing air pollution as a core development challenge.
This publication estimates that the global cost of health damages associated with exposure to air pollution is $8.1 trillion, equivalent to 6.1 percent of global GDP.
People in low- and middle-income countries are most affected by mortality and morbidity from air pollution. The death rate associated with air pollution is significantly higher in low-and lower-middle income countries than in high-income countries.
This publication further develops the evidence base for air-quality management through up-to-date estimates of air pollution’s global economic costs.
The analyses presented here build on previous cost estimates by the Bank and its partners, as well as on more comprehensive air-quality data from monitoring stations in many cities across the world.
By providing monetary estimates of air pollution’s health damages, this publication aims to support policy makers and decision-makers in client countries in prioritizing air pollution amid competing development challenges.
Its findings build a robust economic case to invest scarce budgetary resources in the design and implementation of policies and interventions for improving air quality.
Such investments will deliver benefits for societies at large, and particularly for vulnerable groups.
This publication builds a strong case for scaling up investments for air pollution control in low-and middle-income countries.
About the authors
This report was prepared by a team led by Yewande Awe with the core team comprising Bjorn Larsen and Ernesto Sánchez-Triana. The task team also included Santiago Enriquez and Shafick Hoossein. This report updates the “2020 Cost of Air Pollution” report by using health data for the Global Burden of Disease study published at the end of 2020.
Yewande Awe
Bjorn Larsen
Ernesto Sánchez-Triana
Santiago Enriquez
Shafick Hoossein
The team would like to acknowledge, with thanks, the valuable advice and inputs of the following colleagues: Stephen Dorey, Fernando Loayza, Helena Naber, Katelijn Van den Berg, and Martin Heger (World Bank); and Maureen Cropper (Professor of Economics, University of Maryland). Editorial support was provided by Stan Wanat.
This report is a product of the Environment, Natural Resources, and Blue Economy Global Practice of the World Bank.
This work was conducted under the supervision of Juergen Voegele (Vice President, GGSVP); Karin Kemper (Global Director, SENDR); Richard Damania (Chief Economist, GGSCE); Iain Shuker (Practice Manager, SAEE2); and Christian Albert Peter (Practice Manager, SENGL).
The Pollution Management and Environmental Health Multi-donor Trust Fund of the World Bank provided financial support for the preparation of this report. That support is gratefully acknowledged.
Citation
“World Bank. 2021. The Global Health Cost of PM2.5 Air Pollution : A Case for Action Beyond 2021. International Development in Focus;. Washington, DC: World Bank. © World Bank.
Originally published at:
https://openknowledge.worldbank.org/handle/10986/36501 License: CC BY 3.0 IGO.”
ORIGINAL PUBLICATION
The Global Health Cost of PM2.5 Air Pollution : A Case for Action Beyond 2021
“World Bank. 2021. The Global Health Cost of PM2.5 Air Pollution : A Case for Action Beyond 2021. International Development in Focus;. Washington, DC: World Bank. © World Bank.
Preface
In 2020, as cities around the world went into COVID-19-induced lockdowns, people took notice of the surprisingly blue skies above them. By painfully grinding economic and social activities to a halt, lockdowns resulted in rapid reductions of air pollutants. However, in most cities, air pollution returned to its pre-pandemic levels almost as soon as restrictions were eased. This was a stark reminder of the need to strengthen efforts to tackle air pollution and to integrate air-pollution reductions into countries’ recovery efforts.
According to the Global Burden of Disease 2019[1], PM2.5 (fine particulate matter) air pollution — in both outdoor environments and inside households that use solid fuels for cooking and heating — caused 6.4 million deaths and 93 billion days lived with illness in 2019. While the toll of various risks, including household air pollution, has fallen over time, that of ambient air pollution has continued to rise over the last decade.
The significant health, social, and economic effects of air pollution compel us to support client countries in addressing air pollution as a core development challenge. To this end, the Bank is committed to continue strengthening the evidence base that can inform effective and efficient air-quality interventions. Recent groundbreaking research advanced by the Bank has made substantial contributions to this evidence base in areas that include (a) the importance of prioritizing efforts to reduce air-pollution emissions from coal-fired power plants and diesel-fueled vehicles because the particles in those emissions are more damaging to health than particles from most other air-pollution sources (Thurston, Awe, Ostro and Sánchez-Triana 2021)[2]; (b) demonstrating that particulate matter from dust should continue to be factored into global estimates of the burden of disease of air pollution given the substantial health impact of dust (Ostro, Awe, and Sánchez-Triana 2021)[3]; and © building a strong case for scaling up efforts to establish ground-level networks for monitoring air quality in low-and middle-income countries by demonstrating that satellite-based air-quality estimates are not a sufficiently accurate substitute for ground-level data (World Bank 2021)[4].
This publication aims to further contribute to the evidence base on air-quality management by providing up-to-date estimates of the global economic costs of air pollution. The analysis builds on previous estimates by the Bank and its partners and is based on cutting-edge scientific findings of the health effects of air pollution, as well as more comprehensive air-quality data from monitoring stations in a large number of cities across the world.
By providing monetary estimates of the health damage of air pollution, this publication aims to support policy makers and decision-makers in client countries to prioritize air pollution amid competing development challenges. Its findings build a strong economic case to invest scarce budgetary resources in the design and implementation of policies and interventions to improve air quality that will deliver benefits for societies at large, and particularly for vulnerable groups.
Executive Summary
INTRODUCTION
Air pollution is a major cause of disease and death. “Ambient air pollution” refers to air pollution in the outdoor air; “household air pollution” refers to air pollution originating in the household environment.
Air pollution is the world’s leading environmental risk to health and the cause of morbidity and mortality from diseases such as ischemic heart disease, stroke, lung cancer, chronic obstructive pulmonary disease, pneumonia, type 2 diabetes, and neonatal disorders.
Most deaths related to air pollution are caused by human exposure to fine inhalable particles or fine particulate matter, also known as PM2.5.
Billions of people in developing countries live in places where the ambient and indoor concentrations of PM2.5 are multiple times higher than the health-based guideline values for air quality established by the World Health Organization (WHO).
- An estimated 6.4 million people died prematurely worldwide in 2019 due to exposure to PM2.5 air pollution.
- About 95 percent of those deaths occurred in low- and middle-income countries (LMICs) (GBD 2019 study)[1].
- Seventy percent of the deaths occurred in East Asia and the Pacific, and South Asia. China and India accounted for 52 percent of global deaths from PM2.5.
- There were six countries with more than 100,000 deaths from PM2.5, and nine countries with 50,000–100,000 deaths.
Besides being a health problem, air pollution contributes to less-livable conditions and hinders economic competitiveness.
Poor people are more likely to live in a polluted environment and suffer the adverse impacts of air pollution.
In addition, people who are sick as a result of exposure to air pollution are more likely to take days off work and suffer reduced productivity, which in turn undermines their contributions to economic growth.
Air pollution could also hinder cities’ ability to attract talented workers, thereby reducing competitiveness.
Furthermore, air pollution imposes a heavy economic burden both on the economies of individual LMICs and on the global economy as a result of illness, premature death, lost earnings, and increased health-care expenditures — all of which constrain productivity and economic growth.
Poor people who have the least means to address the health damage of air pollution often disproportionately carry the economic burden.
Air pollution is also associated with many detrimental, but less researched, health impacts and conditions (Sánchez-Triana et al. 2015)[2], such as
- infant mortality (Heft-Neal et al. 2018)[3],
- low birth weight (Ezziane 2013)[4],
- pre-term delivery (Bowe et al. 2018)[5],
- mental health conditions (Shin Park, and Choi 2018)[6],
- and neurological impairment (Xu, Ha, and Basnet 2016[7]; Zhang, Chen, and Zhang 2018[8]) including dementia in later life (Carey et al. 2018)[9].
As the evidence base for these and other conditions becomes stronger, it is envisaged that exposure-response functions can be developed to obtain global estimates of the health burden of air pollution.
Some air pollutants, notably short-lived climate pollutants, such as black carbon, have climate-warming properties (Shindell et al. 2012)[10].
In addition, air pollution (particularly linked to sulfur dioxide) adversely affects the environment, resulting in acid rain and associated land and water pollution.
Air pollution also has aesthetic impacts, such as reduced visibility. However, economic valuation of these impacts can be done only at local and regional levels. Further research is needed to determine how to effectively conduct economic valuation of these impacts at the global level.
Air pollution’s various adverse impacts on multiple facets of the society and economy, particularly of LMICs, squarely place air pollution as a core development challenge. This makes reducing air pollution in developing countries central to achieving poverty reduction and equitable prosperity objectives in those countries.
Global health crises further highlight the need for continued action in addressing a global and cross-cutting challenge such as air pollution. The current global COVID-19 pandemic, caused by the novel coronavirus, SARS-CoV-2, underscores the importance of reducing air pollution through preventive and abatement measures.
People who contract COVID-19 and have underlying medical problems such as heart disease, lung disease, and cancer are at a higher risk of developing serious illnesses that could lead to death. It is noteworthy that air pollution is a cause of the aforementioned diseases.
Ongoing research is finding relationships between air pollution and the incidence of illness and death due to COVID-19. Such research suggests that PM2.5 air pollution plays an important role in increased COVID-19 incidence and death rates.
One such study reported that PM2.5 is a highly significant predictor of the number of confirmed cases of COVID-19 and related hospital admissions (Andrée 2020)[11].
MOTIVATION
This report provides an estimate of the global, regional, and national costs of health damage — that is, premature mortality and morbidity — from exposure to PM2.5 air pollution in 2019.
While recognizing the various costs of air pollution to society, this report focuses on the cost of premature mortality and morbidity of health effects estimated by the GBD 2019 study.
Estimating the health damage of air pollution in monetary terms provides a suitable metric for policy makers and decision makers in developing countries to prioritize the design and implementation of policies and interventions for controlling air pollution amid competing development challenges and budgetary and other resource constraints.
An earlier study by the World Bank and IHME (2016)[12] estimated the cost of premature mortality from ambient air pollution and household air pollution combined in 2013.
The present report estimates the cost of health damages using the estimates of mortality and morbidity from PM2.5 air pollution published in the Global Burden of Disease (GBD) 2019[13] study.
The GBD assesses mortality and disability from numerous diseases, injuries, and risk factors, including air pollution.
Air pollution has long been recognized as a significant environmental health risk.
GBD estimates of the global, regional, and national health burden attributable to air pollution, based on nationwide exposures to ambient PM2.5 as well as household use of solid fuels, were published for the first time in the GBD 2010 study, followed by GBD 2013[14], 2015[15], 2016[16], 2017[17], and 2019[18].
METHODOLOGY
See the original publication
KEY FINDINGS
- The global health cost of mortality and morbidity caused by exposure to PM2.5 air pollution in 2019 was $8.1 trillion, equivalent to 6.1 percent of global gross domestic product (GDP).
The cost ranged from an equivalent of 1.7 percent of GDP in North America, to 9.3 percent in East Asia and Pacific, and 10.3 percent in South Asia (figure ES.1).
The cost was equivalent to 5.9 percent of GDP in low-income countries and rose to 8.9–9.0 percent in lower- and upper-middle-income countries (figure ES.2).
The cost was equivalent to 10.6–12.9 percent of GDP in China and India.
- Globally, 64 percent of total deaths from PM2.5 was due to ambient air pollution and 36 percent due to household air pollution from the use of solid fuels.
However, the cost of household air pollution constituted the largest share in Sub-Saharan Africa and low-income countries, a substantial share in South Asia and lower-middle-income countries, and a moderate share in East Asia and Pacific, Latin America and Caribbean, and upper-middle-income countries.
- Of the estimated total global health cost of PM2.5 air pollution, about 85 percent is due to premature mortality and 15 percent to morbidity.
- The estimated global cost of PM2.5 air pollution in 2019 is 40 percent higher than the estimate for 2013 in World Bank and IHME (2016)[22] in real terms.
The higher cost estimate in this report is related to three sets of factors:
– Improved methodology: This report uses updated exposure-response functions from the GBD 2019[23], which quantitatively relate exposure levels of PM2.5 to the risk of a health damage (chronic obstructive pulmonary disease, stroke, ischemic heart disease, lower respiratory infection, lung cancer, and type 2 diabetes). The GBD 2019[24] also includes neonatal health effects of PM2.5 exposure. Type 2 diabetes and neonatal health effects were not included in the GBD 2013[25].
– Increased availability of data: Ground-level ambient PM measurements utilized by the GBD 2019[26] study came from the updated World Health Organization (WHO) Global Ambient Air Quality Database released in 2018, as well as additional data mainly from Bangladesh, Canada, China, the European Union, the United States, and PM measurement data from US embassies and consulates. Thus, measurement data from 10,408 ground monitors from 116 countries were utilized by the GBD 2019[27]. — Inclusion of an estimate of the cost of morbidity, which was not provided in World Bank and IHME (2016)[28].
· Observations about the reasons for variations between GBD mortality estimates for different years were noted in Ostro et al. (2018)[29], which examined estimates provided in GBD 2010[30], GBD 2013[31], and GBD 2015[32] of mortality related to air pollution. Methodological and technological improvements and demographic changes were found to account for the observed variations in the mortality estimates. Ostro et al. (2018)[33] also noted the need to strengthen ground-level air-quality monitoring and epidemiological studies to improve estimates of PM2.5 exposure and mortality in LMICs that are related to air pollution.
- Although the global availability of exposure data in GBD 2019 increased due to increased ground-level monitoring data, there remains a great need to increase ground-level air-quality measurements in LMICs in order to reduce uncertainties regarding PM2.5 exposure estimates in countries that have limited or no ground-level measurements, particularly of PM2.5.
Analysis of the WHO Global Ambient Air Quality Database 2018 version reveals that there was only one PM2.5 ground-level monitor per 65 million people in low-income countries, and one monitor per 28 million people in Sub-Saharan Africa, in contrast to one monitor per 370,000 people in high-income countries.
FIGURE ES.1 Cost of health damage from PM2.5 exposure in 2019 by region, percent equivalent of GDP (PPP)
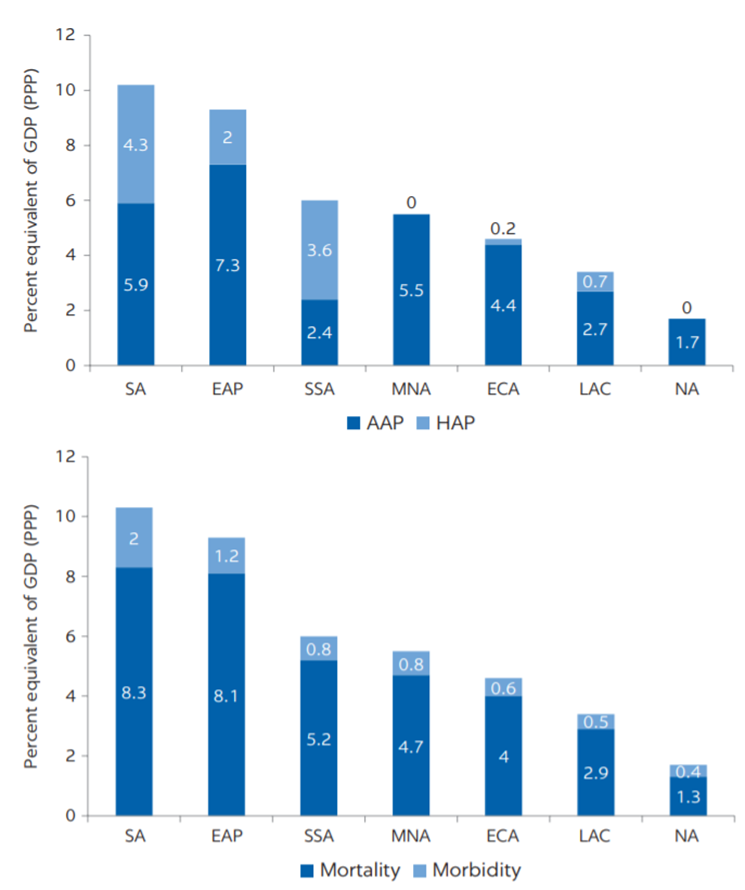
Note: EAP = East Asia and Pacific; ECA = Europe and Central Asia; LAC = Latin America and Caribbean; MNA = Middle East and North Africa, NA = North America; SA = South Asia; SSA = Sub-Saharan Africa. Numbers may not add up due to rounding.
FIGURE ES.2 Annual cost of health damage from PM2.5 exposure, as a share of GDP by income group, 2019
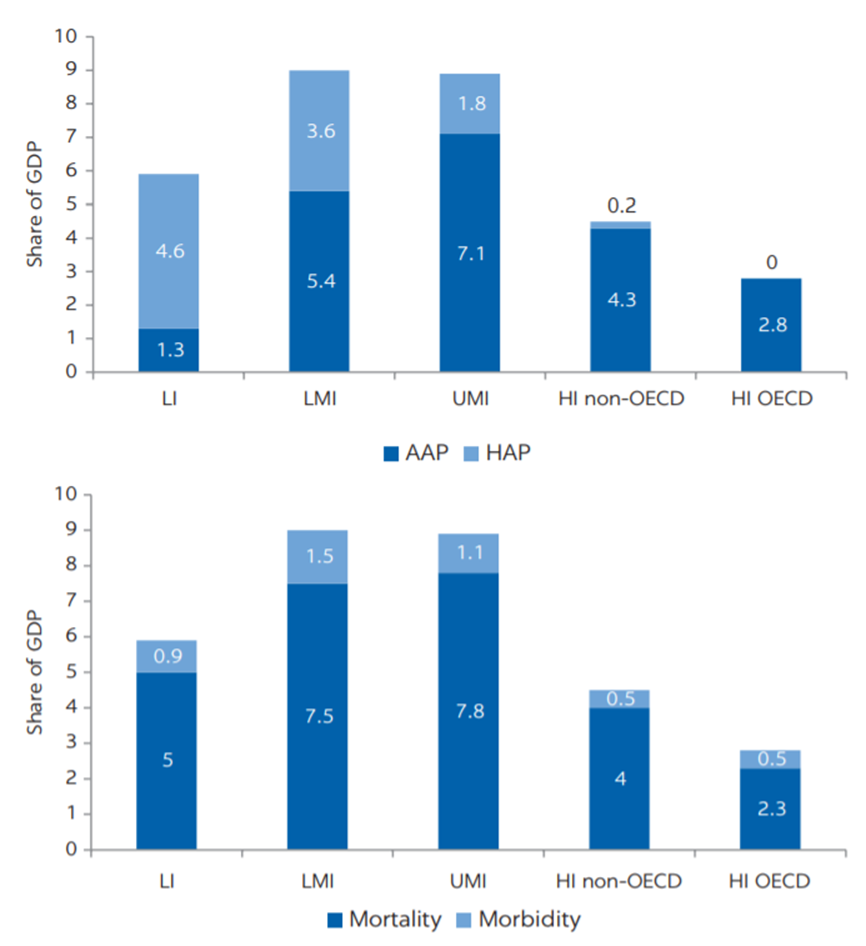
Note: LI = low-income countries; LMI = lower-middle-income countries; UMI = upper-middle-income countries; and HI = high-income countries. PM2.5 = fine particulate matter. OECD = Organisaton for Economic Co-operation and Development. Assignment of countries to categories based on World Bank income classification. Numbers may not add up due to rounding.
Recommendations for policy action
The significant health and economic burdens of PM2.5 air pollution call for urgent action from policy makers in LMICs to reduce air pollution and the resulting disease and deaths.
Some key areas for action include the following:
- Improve ground-level air-quality monitoring.
- Ensure public access to information on air quality.
- Harness innovation to drive air-quality improvements.
- Establish solid technical units with a clear mandate for air-quality management.
- Adopt regional approaches to address air pollution across boundaries.
- Prioritize key sources of PM2.5 air pollution, notably fossil-fuel combustion, such as sulfur-emitting coal-fired power plants and diesel-fueled traffic.
- Engage a wide range of instruments that are suited to effectively and efficiently reduce air pollution and ensure that their use is enforced.
- Promote the use of clean cooking fuels to combat the health effects of household air pollution from solid fuels.
- Improve ground-level air-quality monitoring.
Properly operated and maintained ground-level monitoring networks for air quality provide data on the severity of air pollution, a fundamental input for effective air-quality management. Data for networks that monitor air quality are also useful for identifying the key sources that contribute to ambient air pollution. Such networks for air-quality monitoring must be subject to rigorous quality-assurance and quality-control regimes in order to ensure that the air-quality measurements generated are reliable for informing the design and implementation of interventions to reduce air pollution and protect public health. Thus, high-quality, routine air-quality monitoring, first and foremost, underpins programs for effective air-quality management that would also include (a) comprehensive emission inventories; (b) application of models to understand the transport and fate of air pollutants; © assessment of costs and of health and other benefits; and (d) public outreach and stakeholder engagement. It is pertinent to note that beyond initial investments in networks for air-quality monitoring, governments need to ensure effective funding for sustained operation and maintenance of programs for air-quality monitoring in the long term.
- Ensure public access to information on air quality.
To reinforce the impact of networks for air-quality monitoring, air-quality management efforts should include a robust system for public dissemination of air-quality data in formats that are widely understood and easily accessible to members of the public. Public dissemination of air-quality data allows members of the public to take adequate measures to reduce their exposure to air pollution and thus provides an important social safety net for the public — particularly for vulnerable groups such as young children, the elderly, and people with health conditions that can be exacerbated by poor air quality.
- Harness innovation to drive air-quality improvements.
Technological developments can support more-targeted interventions for air-quality management while providing new avenues to engage local communities in their implementation. For instance, the Environmental Defense Fund and partners such as Google are piloting the use of low-cost sensing technologies and data analytics to provide air-quality data with a significantly higher frequency (every minute or few minutes) and resolution (for example, city block by city block). These hyperlocal monitoring networks can identify areas of poor air quality that a sparse network of traditional monitors often misses, help to better estimate actual exposure to air pollution, and even provide real-time data to help vulnerable populations make decisions that will protect their health.
- Establish solid technical units with a clear mandate for air-quality management.
Technical units, staffed with specialists who can carry out a range of actions, including monitoring, enforcement, and planning, are indispensable to improve air quality. Such units should have clear responsibilities for designing air-quality interventions that can be endorsed by decision-makers and other stakeholders, as well as for conducting regular evaluations to assess the efficiency and effectiveness of supported interventions, identify opportunities for improvement, and incorporate new scientific evidence or emerging technologies that can drive air-quality improvements. Providing technical units with the mandate to work across sectors is paramount, given that air pollution originates from a wide range of sectors, including energy, transportation, industry, and agriculture, among others.
- Adopt regional approaches to address air pollution across boundaries.
Air pollution typically cuts across boundaries of individual cities or countries. As a result, regional airshed approaches to addressing PM2.5 air pollution may be called for, which require federal and international collaboration of governments across multiple administrative jurisdictions and geographical boundaries to ensure effective air-quality management.
- Prioritize key sources of PM2.5 air pollution, notably fossil-fuel combustion, such as sulfur-emitting coal-fired power plants and diesel-fueled traffic.
Efforts to control air pollution that prioritize fossil-fuel combustion sources are most likely to return greater health benefits than broad efforts that do not consider the source and composition of PM2.5. Sulfate — a chemical constituent of PM2.5 from coal burning — is one of the greatest contributors to PM2.5 toxicity and has one of the strongest associations with cardiovascular disease among the chemical constituents of PM2.5 from fossil-fuel combustion. Reductions in PM2.5 emissions from fossil-fuel combustion, such as sulfur-emitting coal-fired power plants and diesel vehicles, can be expected to produce the most-significant health benefits per unit of PM2.5 reduced. Given that these sources are also key contributors to climate warming, air-pollution efforts that target these sources will also provide benefits to mitigating climate change. Notably, reducing PM2.5 also means reducing black carbon, a component of PM2.5 and short-lived climate pollutant.
- Engage a wide range of instruments that are suited to effectively and efficiently reduce air pollution and ensure that their use is enforced.
In order to reduce air pollution, governments need to apply the instruments and approaches that are most effective for reducing air pollution. Command-and-control instruments (such as standards for ambient air quality and emission standards for vehicles and stationary sources, and vehicle inspection and maintenance programs) are well established and applied in many countries. Additional command-and-control instruments include regulations to improve fuel quality by, for example, decreasing the sulfur content of fuels. Economic instruments (such as air-pollution charges and repurposing of fossil-fuel subsidies) reduce air and climate pollutants while also augmenting the amount of government revenues that can be allocated to education, healthcare, renewable energy, and interventions to control air pollution. In addition, policies to promote conversion of vehicles from diesel to gas or to discourage the use of nitrogen-based fertilizers (which release ammonia — a precursor of secondary PM2.5 formation) may also be used to reduce air pollution. It is important to note that effective application of the various instruments for air-quality management requires that governments put in place adequate enforcement mechanisms that also include incentives to reduce polluting behaviors.
- Promote the use of clean cooking fuels to combat the health effects of household air pollution from solid fuels.
The populations in low- and middle-income countries using traditional cook-stoves with solid fuels for cooking and other domestic purposes are exposed to PM2.5 concentrations that are several times higher than ambient PM2.5. Improved cook-stoves, often 40–60 percent more energy efficient than traditional stoves, have been found to reduce exposure by around 50 percent. This reduction, however, reduces health effects by as little as 11–12 percent, based on analysis of the exposure-response functions from the GBD 2019[34]. Effectively combating the health effects requires clean cooking fuels and technologies, such as LPG or electricity. Some low- and middle-income countries have already achieved a high prevalence rate of the population using clean fuels and technologies, demonstrating this possibility even at moderate GDP per capita levels.
References
See the original publication