Financial Times
Miranda Green
Miranda Green is the FT’s deputy opinion editor
FEBRUARY 25 2022
Key messages
About Cancer Backlog Management and Pandemic Recovery, with inputs for a National Cancer Strategy.
This is a synthesis from a strategic management perspective.
The Editor also sympathizes with the Author´s suffering and respects her personal history.
Summarized by Joaquim Cardoso MSc.
Chief Strategy Officer (CSO) and CEO of
“The Cancer Strategy Institute”
March 5, 2022
The cancer backlog due to pandemic
- There were between 240,000 and 740,000 “missing” urgent GP referrals for suspected cancer during the pandemic, according to the National Audit Office.
- Between 35,000 and 60,000 fewer people started treatment for cancer than expected.
- the UK is now in danger of going backwards in terms of cancer survival for the first time in 40 years.
The backlog of cancer patients caused by the pandemic will haunt the NHS for years.
- This is not unique to the UK; every healthcare system in the world struggled to cope with the impact of Covid.
- A study published in December in the journal Cancer found that new diagnoses in the US fell by up to 23 per cent in 2020, with the authors warning that the country was “yet to enter a ‘catching-up’ period”.
But the NHS went into 2020 particularly underpowered after almost a decade of government austerity, …
- with fewer doctors, nurses and hospital beds than in many comparable countries.
- Only 55 per cent of British cancer cases are diagnosed at stage 1 or 2, early enough to give the best chance of successful treatment.
To get this number up, the NHS desperately requires:
- More CT and MRI machines — at least enough to match OECD levels, according to the Institute for Public Policy Research
- “One stop shops”, such as the one at Ritchie Chalmers’ hospital in Kent, should be rolled out across the country, an NHS-commissioned report by Sir Mike Richards recommended in late 2020, suggesting some could be based in retail parks or high-street shopping centres. A few are already up and running, with health secretary Sajid Javid promising more.
- Staffing is the third priority. One in ten cancer specialist posts remains vacant. Unfortunately, this may be the most difficult problem to fix, given the recruitment problems facing the NHS as a whole.
- Even if you have the machines, you need specialists to interpret the results.
- There are almost 2,000 full-time consultant clinical radiologist posts unfilled in the UK, a shortfall of 33 per cent, according to the Royal College of Radiologists.
- The problem is so acute that last year it emerged that 14 per cent of scans were being outsourced for preliminary analysis to other countries, including Australia and New Zealand.
5. Meanwhile, the number and roles of GP´s needs also to be reevaluated
- The number of family doctors in England has stagnated after years of underfunding, even as demand for their services has risen. The average number of patients each GP is responsible for has increased by about 16 per cent since 2015 — about 300 more people per doctor.Many clinicians argue these overstretched services are delaying cancer diagnoses.
- A 2019 survey by the charity Breast Cancer Now found that a quarter of patients with secondary breast cancer had visited their GP multiple times before being diagnosed.
- Charles Swanton, the chief clinician at Cancer Research UK, said: “The more I look into the current situation in the UK regarding early diagnosis, the more worried I am that we are still not getting the basics right.”
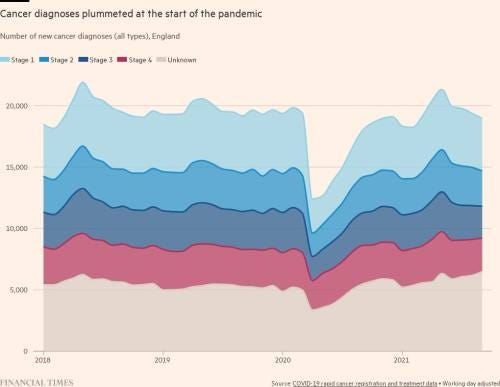
Infographic:
Cancer diagnoses plummeted at the start of the pandemic
ORIGINAL PUBLICATION (long version)

Cancer, Covid and me
Financial Times
Miranda Green
Miranda Green is the FT’s deputy opinion editor
FEBRUARY 25 2022
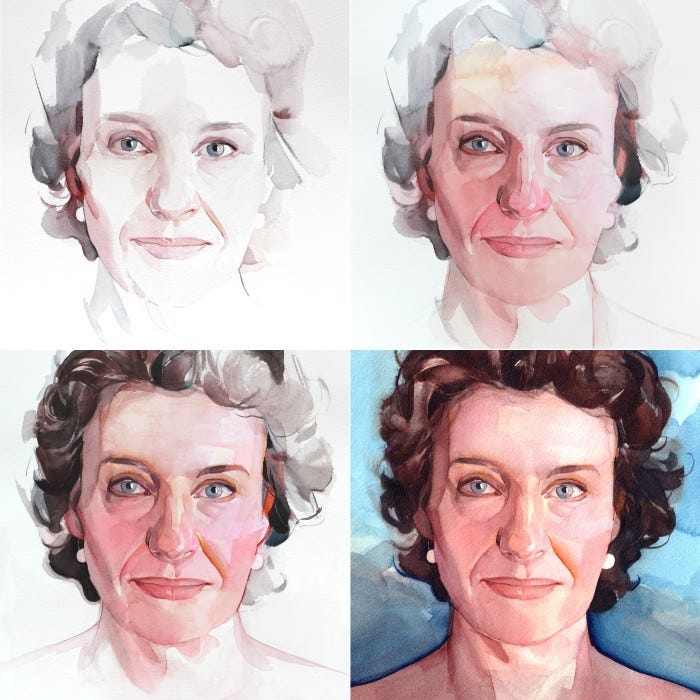
An afternoon in March 2020. I emerged in a daze on to the banal horrors of a London high street. Inside the hospital behind me, a surgeon had explained that not only did I have breast cancer, rather than the harmless cysts that the general practitioner, screening technicians and nurses had assured me were most likely, but the tumour was quite sizeable. It was diffuse, invasive and probably required removal of my right breast.
Normally, this type of hormone-dependent carcinoma would have placed me on a well-trodden treatment path: surgery to remove the tumour followed by endocrine medication. In the UK, this course has excellent results in cases that are identified early. But my case, like tens of thousands of others over the past two years, was not normal. My diagnosis coincided with the start of the Covid emergency and my treatment, postponed and precarious, coincided with the worst health crisis in the country’s modern history. So began the most surreal and extreme period of my life.
Yet I am one of the lucky ones. Some of those whose cancer symptoms began during the pandemic were too afraid to visit their GP or couldn’t get an appointment when they tried. For others, cancelled scans, interrupted chemotherapy and delayed operations tipped the scale away from survival.
For others, cancelled scans, interrupted chemotherapy and delayed operations tipped the scale away from survival.
There were between 240,000 and 740,000 “missing” urgent GP referrals for suspected cancer during the pandemic, according to the National Audit Office. Between 35,000 and 60,000 fewer people started treatment for cancer than expected.
Michelle Mitchell, chief executive of Cancer Research UK, a science and advocacy charity, has warned the UK is now in danger of going backwards in terms of cancer survival for the first time in 40 years.
There were between 240,000 and 740,000 “missing” urgent GP referrals for suspected cancer during the pandemic, according to the National Audit Office. Between 35,000 and 60,000 fewer people started treatment for cancer than expected.
Michelle Mitchell, chief executive of Cancer Research UK, a science and advocacy charity, has warned the UK is now in danger of going backwards in terms of cancer survival for the first time in 40 years.
While the UK’s free-to-use, taxpayer-funded healthcare often tops international league tables for access, it has long underperformed on cancer.
A study of data from 1995 to 2014 showed survival rates trailing other comparable countries, including Australia, Canada and Norway, although the gap was narrowing in the years before 2019.
“Prior to Covid, we were headed in the right direction but not moving fast enough,” says Mitchell. “This has been devastating for cancer services.”
While the UK’s free-to-use, taxpayer-funded healthcare often tops international league tables for access, it has long underperformed on cancer.
Hard-to-treat cancer cases including those that present too late are described as having “negative outcomes”.
What this means, of course, is death. As a patient, medical euphemisms can be a blessing. They draw a veil over the terror. Perhaps the most chilling conversations I had were about percentage chances of survival at five and 10 years. I didn’t always want to hear it in such stark terms. But, as a country, there is no more time for euphemisms. This subject needs to be addressed, honestly and directly.
A week after my initial diagnosis I returned for a follow-up appointment. The hospital was already taking overflow Covid cases from another facility in the outer suburbs that was about to declare a critical incident after running out of capacity. As I arrived an elderly Indian man in kurta pyjamas and an overcoat was being given oxygen as paramedics wheeled him in from an ambulance.
After an MRI scan, I met the same gruff surgeon in the same small room. This time he was in scrubs, a face mask, hat and plastic gloves, and he opened the door with his elbows. As he began to speak, the icy cold sensation that had taken residence in my chest from the moment of diagnosis got progressively worse. The MRI showed the tumour in my right breast was much larger than originally thought (the type of breast cancer I had, lobular, is harder to see on scans), and all the breast tissue would have to be removed. But surgery for cases such as mine, the doctor told me, had been suspended.
He could not send me for the standard PET-CT scan to see if it had spread because of the risk of Covid contamination on the machines. I should collect a packet of Tamoxifen, which would, with luck and statistical probability on my side, stop the cancer feeding off my oestrogen. Then I should go home and, well, what exactly?
“Is it safe to wait? Will I be safe?” I asked.
“I can’t tell you that,” he said, avoiding my eyes.
“Is it safe to wait? Will I be safe?” I asked.
“I can’t tell you that,” he said, avoiding my eyes.
Instead, hunched and tense, he launched into a diatribe about the government’s lateness in deciding to lock down, two months after the World Health Organization had declared Covid-19 a public health emergency. My role in that room, before the meeting was cut short so that the rest of the waiting patients could be given their own bad news, felt more like a comforter for this panic-stricken professional than a patient. When he told me, finally, to “just get out of here”, I understood on a rational level that he meant for my own safety. But it felt like an ejection, an abandonment even.
The nurse who had provided expert tea and sympathy a week earlier led me into another room. “Blood on their hands,” she said, referring to the laggardly ministers. She emphasised that time was short. They were getting patients in and out fast, amid fear of contagion. Her eyes welled up. “This isn’t the care we are used to offering”. Tamoxifen was very good, she assured me; it was my best bet to keep the tumour at bay for now although, she told me, they usually only used it before surgery in postmenopausal women.
At least I saw her.
At the peak of the UK’s first wave, 400 specialist cancer staff working for Macmillan, the cancer care charity, were redeployed to the Covid response.
The surgeon had warned me the department might not be there a few months later. He was expecting to be pulled in to work in an intensive care unit along with other medics.
Months later, one of my surgeons and a senior oncologist separately told me they believed too many cancer services were stopped during the first wave.
At the peak of the UK’s first wave, 400 specialist cancer staff working for Macmillan, the cancer care charity, were redeployed to the Covid response.
Cancer diagnoses plummeted at the start of the pandemic
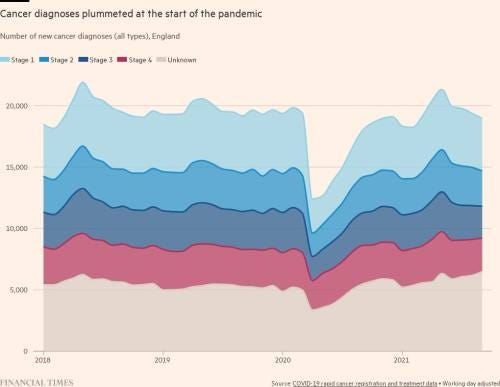
Macmillan concluded the same, arguing in October 2020 that there should never again be “blanket” suspensions of tests and treatment.
But the decisions were being taken in a vacuum of knowledge about this novel virus and its dangers. “No one really knew what we were dealing with,” one surgeon told me months later, “or how bad the transmission within hospitals would be.”
Even as I walked away from the hospital, I was trying to make sense of the drama in which I found myself. It felt like I’d wandered into a disaster movie about a mysterious global virus in which a main cast of medics and scientists were racing against time to treat patients and create a vaccine. Somewhere way down the publicity poster, and a good minute into the trailer, there would be a minor character diagnosed with stage-2 cancer, curable, that couldn’t be operated on because of the pandemic. The writers would probably sacrifice her half way through, I thought. Somehow this role had fallen to me.
Somewhere way down the publicity poster, and a good minute into the trailer, there would be a minor character diagnosed with stage-2 cancer, curable, that couldn’t be operated on because of the pandemic.
I collected the pills, avoiding a man in the pharmacy who was coughing and spluttering, walked a few blocks and bought a frozen lasagna. Whatever crisis hits, you still have to feed the children. Then I hailed a taxi and, for almost the first time in my life, didn’t chat to the driver.
Early diagnosis is one of the key determinants of survival when it comes to cancer.
The first time I sensed something was wrong was many months before my diagnosis. I had asked the GP, who was treating my crushing bouts of fatigue with iron, about a weirdly swollen, uncomfortable breast. Keep an eye on it, he said, and I wrote “boob” on my to-do list.
Months later I went in again. The discomfort had become focused on an area of definite thickening. A different GP told me that “it all gets a bit lumpy and bumpy at your age”.
But after examining me, she referred me for a mammogram and ultrasound.
Early diagnosis is one of the key determinants of survival when it comes to cancer.
The first time I sensed something was wrong was many months before my diagnosis.
In the UK, the GP is the gatekeeper to almost all healthcare other than emergencies. They order tests and scans, prescribe medication and refer to specialists when needed. The strength of the system, in theory, is the relationship formed between a GP and their patients, and in the continuity they offer, sometimes over decades.
In the UK, the GP is the gatekeeper to almost all healthcare other than emergencies.
But the number of family doctors in England has stagnated after years of underfunding, even as demand for their services has risen. The average number of patients each GP is responsible for has increased by about 16 per cent since 2015 — about 300 more people per doctor.
But the number of family doctors in England has stagnated after years of underfunding, even as demand for their services has risen.
The average number of patients each GP is responsible for has increased by about 16 per cent since 2015 — about 300 more people per doctor.
Many clinicians argue these overstretched services are delaying cancer diagnoses.
- A 2019 survey by the charity Breast Cancer Now found that a quarter of patients with secondary breast cancer had visited their GP multiple times before being diagnosed.
- Charles Swanton, the chief clinician at Cancer Research UK, told me: “The more I look into the current situation in the UK regarding early diagnosis, the more worried I am that we are still not getting the basics right.”
… a quarter of patients with secondary breast cancer had visited their GP multiple times before being diagnosed.
Last summer, I spoke over Zoom to Ritchie Chalmers, a leading breast cancer surgeon in Kent. She believed the reliance on GPs to spot possible cancer cases was problematic, even before Covid hit.
“We are stuck with a legacy of how we used to do things,” she said. “Putting everyone through the same funnel doesn’t work. It needs specialist triage. GPs are always going to refer someone with a red flag symptom. Why are we wasting their time seeing people who they would refer anyway?” In her NHS hospital, a new diagnostics hub offers fast access to investigations. A range of tests can be taken in one visit, scans and results given on the same day.
Ritchie Chalmers, a leading breast cancer surgeon in Kent, believes that …the reliance on GPs to spot possible cancer cases was problematic, even before Covid hit.
Chalmers’ centre is well resourced, which isn’t the case everywhere.
- While Australia has 70 CT scanners per million residents, the UK has nine.
- Against the same population measure, Australia has twice as many MRI machines as the UK.
- A Channel 4 investigation last year revealed that almost a third of England’s NHS trusts were using CT scanners that were 10 years old or more.
The UK has one of the lowest numbers of CT and MRI machines per head of population in the OECD
Per million inhabitants, OECD countries (latest)
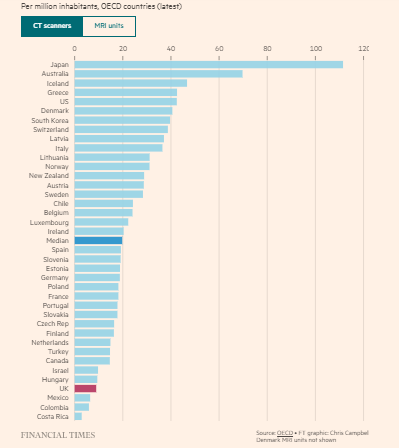
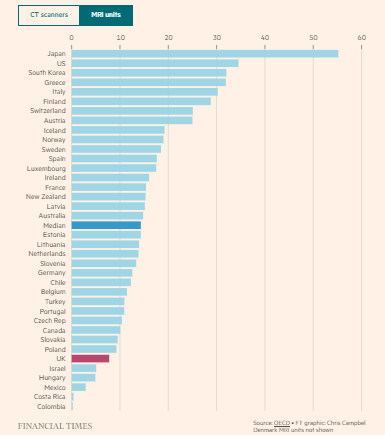
The UK has one of the lowest numbers of CT and MRI machines per head of population in the OECD
Even if you have the machines, you need specialists to interpret the results.
- There are almost 2,000 full-time consultant clinical radiologist posts unfilled in the UK, a shortfall of 33 per cent, according to the Royal College of Radiologists.
- The problem is so acute that last year it emerged that 14 per cent of scans were being outsourced for preliminary analysis to other countries, including Australia and New Zealand.
Even if you have the machines, you need specialists to interpret the results — what is not the case.
(1) There are almost 2,000 full-time consultant clinical radiologist posts unfilled in the UK, a shortfall of 33 per cent,
(2) last year it emerged that 14 per cent of scans were being outsourced for preliminary analysis to other countries, including Australia and New Zealand.
Once I knew the surgery I needed would be delayed for months, and after a frantic round of calls with friends and colleagues, I got a second opinion privately via the FT’s employee healthcare plan. But the private medical team was not able to operate any more than the NHS doctors. The data coming in from China and Italy as Covid had surged through their hospitals suggested it was just too dangerous. Patient mortality rates were way higher than normal, my surgeon told me. All the oncologist could do was recommend escalated hormonal treatment — monthly injections — which I began immediately at my GP surgery.
Once I knew the surgery I needed would be delayed for months, and after a frantic round of calls with friends and colleagues, I got a second opinion privately …
All the oncologist could do was recommend escalated hormonal treatment — monthly injections — which I began immediately at my GP surgery.
And so the blazing hot spring and early summer of 2020 became a horrible wait. I kept the cancer secret from my children and my mum until I had an operation date, wanting to shield them from an additional pandemic fear: that my illness might become deadly before surgery could restart. I kept reliving the initial diagnosis, feeling my body react to the shock all over again. I worked remotely, along with everyone else, and did industrial amounts of Zoom yoga. But the terror gave a hallucinatory sheen to life. I handled the boxes of Tamoxifen reverently. I took cold showers to boost my immune system. I cuddled the kids and, as advised, stayed away from all booze.
In June, falling Covid cases allowed a gradual opening-up in the UK. It was finally possible to meet my new private surgeon in person and have a follow-up ultrasound. The five-centimetre tumour was found to have not only stopped growing but was slightly in retreat.
In June, falling Covid cases allowed a gradual opening-up in the UK. It was finally possible to meet my new private surgeon in person and have a follow-up ultrasound.
The long-delayed CT scan revealed no “distant disease”, meaning the cancer had not spread elsewhere. I staged a tiny one-person party in my garden, allowing myself a glass of champagne.
In July, I was offered various routes to breast reconstruction and told to prepare for a two-week quarantine before and after an operation to remove the tumour the following month.
In July, I was offered various routes to breast reconstruction and told to prepare for a two-week quarantine before and after an operation to remove the tumour the following month.
Who else was getting operations during this time?
A friend in the north-west of England managed to get a lumpectomy that Easter just as the UK was locking down because she had an aggressive tumour that was not controllable with hormone suppressants.
Other breast cancer sufferers had mastectomies but were not offered reconstructive surgery.
The regional variations were making already unequal access to cancer treatment worse, with some hospitals more overwhelmed by the virus than others.
Forty-eight hours before my operation, as London sweltered, I went for a Covid swab. Every night of the quarantine fortnight before, I had lain in bed, sweating from a hellish combination of summer heat, hormonal lows and pure fear, going through all the ways the pandemic might yet, at the last minute, interfere with the doctors getting that goddamn thing out of me. But the test came back negative. Through shielding I had avoided the virus, and the operation went ahead.
I woke up to less positive news. Despite nothing showing up on the scans, the surgeons had found cancer in my lymph nodes, so the whole lymph system in my right arm had been removed. Some patients don’t give consent to this, preferring a separate operation so that they can be “in control”. The doctors and I agreed that 2020 was not a year for illusions of control.
I would need chemo, five months of it. The drugs they had been too concerned to prescribe to some cancer patients during the first wave — because they weaken your immune system substantially — were necessary to hunt down any lingering cancer cells that might have migrated from my original tumour.
I would need chemo, five months of it.
I cried a bit and, for the next few days, lay in the hospital bed listening to Joni Mitchell on my smartphone, warbling along through an opioid fog. No visitors were allowed. The fear of catching Covid affected everything. We sent the kids to the seaside to stay with family for a few days after I arrived home; when they got back I couldn’t hug them for a week in case they had the virus. As I staggered around nursing my post-operative wounds, my partner stoically injected me with the nightly anticoagulant and made us TV dinners. “Don’t lift anything heavier than a tea bag,” the nurse had said.
At this point, something happens to your mindset. You become a patient for the long haul. I kept up a cheerful patter with my mum, but I’d seen the look on the surgeons’ faces in the latest meetings. I knew I had to get myself ready for the next chapter of the ordeal — an autumn and winter of intensive chemotherapy with no Covid vaccine in sight. Then, after a recuperation break, three weeks of daily radiotherapy. (The hormone treatment will go on for several years.)
At this point, something happens to your mindset. You become a patient for the long haul.
… then, after a recuperation break, three weeks of daily radiotherapy. (The hormone treatment will go on for several years.)
A friend who has been through chemotherapy more than once told me to think of it as a “cell spa”, a clear out of nasties, as the drugs flood your system while you sit back and think of the medical miracle working to improve your future chances. A hairdresser who gave my hair a wonderful makeover just before it all started to fall out advised me to take Valium before the first session and play very loud rock music, as he had done during his own chemo infusions. “I used to get through the whole of Bat Out of Hell,” he told me. I didn’t do either, but we giggled about making a mixtape for patients: Now That’s What I Call Chemo.
Jokes help. As does communication, however remote, with other members of this peculiar club. Cancer is a common condition and becoming more so as the population ages. In The Emperor of All Maladies, oncologist Siddhartha Mukherjee writes that cancer is “stitched into our genome”. There was no particular reason I had become the one in eight British women who develops breast cancer. My favourite nurse shrugged after I pursued this line of questioning with her for the umpteenth time. “I’m afraid,” she said, “you’re just there to make up the numbers.”
My weekly visits to the clinic were a social occasion amid the enforced isolation of the pandemic. The steroids made me feel loopy. One of the chemo drugs, derived from the toxin of the yew tree, makes you so intoxicated you can’t drive. Public transport and cabs were forbidden, so two friends gave me lifts to the clinic. I sat in the back, masked up and with all the windows open. After treatment, my partner and daughters would collect me as I tottered out, high as a kite and ready to go home and party before the side effects kicked in.
One of the chemo drugs, derived from the toxin of the yew tree, makes you so intoxicated you can’t drive.
But as the second lockdown was imposed in October 2020, with restrictions toughened further that December, the world around our family bubble became increasingly scary again. The clinic staff started to wear extra protective equipment over Christmas. As the UK death toll rose sharply, the atmosphere became tense. A few patients and staff had been on the priority list for the BioNTech/Pfizer jab, but the rest of us were still waiting. At every step I was assured that, unlike for some patients during the first wave, my chemotherapy and radiotherapy would not be stopped unless I tested positive. This added hugely to my fear of contracting the virus.
I hit my low point on January 20 2021 during a chemotherapy infusion. That day, 1,820 people were reported to have died from Covid in the UK, in what would turn out to be the peak of daily deaths recorded during the pandemic. The Sun ran a huge headline, “Hope and a prayer” over a picture of people waiting for their first vaccine, while the Guardian had a story about London buses being turned into makeshift ambulances to relieve pressure on the capital’s emergency services. Rather than continue to become physically weaker against such a horrifying backdrop, and with the cumulative side effects starting to defeat me, I decided to stop the chemo a fortnight early.
I hit my low point on January 20 2021 during a chemotherapy infusion.

The backlog of cancer patients caused by the pandemic will haunt the NHS for years.
This is not unique to the UK; every healthcare system in the world struggled to cope with the impact of Covid.
A study published in December in the journal Cancer found that new diagnoses in the US fell by up to 23 per cent in 2020, with the authors warning that the country was “yet to enter a ‘catching-up’ period”.
The backlog of cancer patients caused by the pandemic will haunt the NHS for years
But the NHS went into 2020 particularly underpowered after almost a decade of government austerity, with fewer doctors, nurses and hospital beds than in many comparable countries.
Only 55 per cent of British cancer cases are diagnosed at stage 1 or 2, early enough to give the best chance of successful treatment.
To get this number up, the NHS desperately requires more CT and MRI machines — at least enough to match OECD levels, according to the Institute for Public Policy Research.
“One stop shops”, such as the one at Ritchie Chalmers’ hospital in Kent, should be rolled out across the country, an NHS-commissioned report by Sir Mike Richards recommended in late 2020, suggesting some could be based in retail parks or high-street shopping centres. A few are already up and running, with health secretary Sajid Javid promising more.
Staffing is the third priority. One in ten cancer specialist posts remains vacant, says Cancer Research UK’s Mitchell. Unfortunately, this may be the most difficult problem to fix, given the recruitment problems facing the NHS as a whole. But, as Mitchell notes, “None of us want to live in a country where cancer survival is going backwards. I do think there is a significant political dimension to this.”
The NHS desperately requires:
(1) more CT and MRI machines ; (2) “One stop shops”, such as the one at Ritchie Chalmers’ hospital in Kent, should be rolled out across the country; and (3) Staffing is the third priority.
None of us want to live in a country where cancer survival is going backwards. I do think there is a significant political dimension to this.”
Next month I will have survived two years since my diagnosis and the start of the pandemic.
The experience has left me with recurring bouts of anxiety, a partially reconstructed breast built from belly fat (a modern miracle), a brutally accelerated menopause and, of course, a whole lot less hair.
So far, the serenity I thought might be the upside is proving elusive. I can feel my breath becoming shallow even as I write this. The fight-or-flight response is stuck and the traumatic moments haven’t been “filed” as historical yet, says my counsellor.
A very experienced breast care nurse once told me: “Some people end up defined by their cancer afterwards, some put it right behind them. You have to live your life. There aren’t many in between.” I’m not sure yet which I am. And how to live has always seemed a puzzle, cancer or not.
But of course I’m lucky to face such a dilemma. I think back to that original waiting room, watching other patients being called in to the surgeon, some emerging pale and shattered. What happened to the very thin woman, shoulder blades jutting up through her jacket, who was there with a sister, both crying? What about the woman I recognised from the local nail bar? I had access to private medical care, an alternative route that kept me on track to recovery. That comes with a dose of survivor’s guilt. I’m back in the original hospital for follow-up infusions to prevent anything bad turning up in my bones, and I’m grateful that the NHS, post-initial crisis, has eased me back into the system, helping with complications and the ongoing hormonal medication.
I had access to private medical care, an alternative route that kept me on track to recovery. That comes with a dose of survivor’s guilt.
I’m back in the original hospital for follow-up infusions to prevent anything bad turning up in my bones, and I’m grateful that the NHS, post-initial crisis, has eased me back into the system, helping with complications and the ongoing hormonal medication.
But then I remember the nurse left to comfort desperately frightened patients in a hospital department rushing towards lockdown around her, unable to offer the care or reassurance she was used to providing. And I become distressed again. For myself, for the medics and scientists who know we can do better, and for those who slip through the cracks.
And I become distressed again. For myself, for the medics and scientists who know we can do better, and for those who slip through the cracks.
About the author
Miranda Green is the FT’s deputy opinion editor
Originally published at https://www.ft.com on February 25, 2022.
Names cited
Michelle Mitchell, chief executive of Cancer Research UK, a science and advocacy charity,
Charles Swanton, the chief clinician at Cancer Research UK,
Ritchie Chalmers, a leading breast cancer surgeon in Kent.
Siddhartha Mukherjee ,oncologist, author of In The Emperor of All Maladies,
Sajid Javid , UK health secretary
TAGS: Pandemic Impact; Pandemic Recovery, Backlog Management; Cancer Services; Health issues; Cancer Strategy