health transformation institute
the most comprehensive knowledge portal
for continuous health transformation
Joaquim Cardoso MSc*
Chief Strategy Officer (CSO), Chief Researcher and Editor
November 25, 2022
MSc* from London Business School — MIT Sloan Masters Program
Executive Summary
What is the message?
- In a review of 33 cancer screening guidelines, researchers have found that the guidelines don’t adequately capture the potential harms of cancer screening.
- By finding precancerous growths before they turn into cancer or finding cancer at an earlier, more treatable stage, screening tests can reduce deaths from cancer.
- But screening can also cause various harms including physical harm, worry and stress, inaccurate results, and unnecessary follow-up procedures. (See the box below for a list of potential screening harms.)
What are the implications?
- The analysis may allow different guideline bodies to compare themselves and identify areas they hadn’t previously considered,” …
- More research is needed to learn how frequently some screening harms happen, especially in community health care settings
What are the recommendations?
- Based on their findings, the research team suggested two calls to action for guideline developers.
- We’re encouraging [guideline developers] to do deeper dives before they update their guidelines the next time, to make sure that they’re really using the best possible evidence [on screening harms] to make their recommendations,”
- The second is a call for greater transparency about how guideline developers make their recommendations.
BOX: What are the Harms of Cancer Screening?
All screening tests have potential harms.
- Physical harm: Screening tests can cause minor physical harm like bruising or discomfort, as well as serious physical harm like tearing the colon during colon cancer screening.
- Radiation exposure: Some screening tests use low doses of radiation that can damage healthy cells.
- False-negative result: Screening tests sometimes miss an instance of cancer, which could lead people to skip going to the doctor when they have symptoms.
- False-positive result: Screening tests can suggest that cancer is there when it really isn’t. A false-positive result can cause anxiety and is usually followed by more tests and procedures, which also have risks.
- Overdiagnosis: Sometimes screening tests find cancers that are so small and slow-growing that they would never cause any symptoms or become life-threatening. But if people get treatment for these cancers, they are exposed to unnecessary side effects and costs.
- Psychological harm: Many people feel worried and stressed about getting ready for a screening test, waiting for the results, getting follow-up tests, and getting an inaccurate result.
- Incidental findings: Cancer screening tests might find an unrelated medical issue-such as finding an unrelated heart problem-and require follow up tests or procedures which also have risks.
ORIGINAL PUBLICATION (nci)

Comparing the benefits and harms of cancer screening
National Cancer Institute
by Nadia Jaber
November 23, 2022
In a review of 33 cancer screening guidelines, researchers have found that the guidelines don’t adequately capture the potential harms of cancer screening.
Providing information on harms is critical so people can have informed discussions with their health care providers about screening, the researchers noted.
Screening tests, such as mammograms, HPV or Pap tests (also called Pap smears), and colonoscopies, check for cancer or precancerous growths in people who don’t have any symptoms of the disease.
In a review of 33 cancer screening guidelines, researchers have found that the guidelines don’t adequately capture the potential harms of cancer screening.
Screening tests, such as mammograms, HPV or Pap tests (also called Pap smears), and colonoscopies, check for cancer or precancerous growths in people who don’t have any symptoms of the disease.
By finding precancerous growths before they turn into cancer or finding cancer at an earlier, more treatable stage, screening tests can reduce deaths from cancer.
But screening can also cause various harms including physical harm, worry and stress, inaccurate results, and unnecessary follow-up procedures. (See the box below for a list of potential screening harms.)
By finding precancerous growths before they turn into cancer or finding cancer at an earlier, more treatable stage, screening tests can reduce deaths from cancer.
But screening can also cause various harms including physical harm, worry and stress, inaccurate results, and unnecessary follow-up procedures. (See the box below for a list of potential screening harms.)
For those reasons, screening is recommended only when the potential benefits outweigh the potential harms, …
… said Paul Doria-Rose, Ph.D., chief of NCI’s Healthcare Assessment Research Branch.
“If there’s overwhelming evidence of a net benefit of a screening test, we don’t want to scare somebody off” from getting screened, Dr. Doria-Rose said.
“But by the same token, if there’s a risk that [a serious harm] could happen if you have a screening test or a follow-up diagnostic test, then it’s a physician’s obligation to inform patients about what the risks of those procedures are,” he said.
“If there’s overwhelming evidence of a net benefit of a screening test, we don’t want to scare somebody off” from getting screened, …
“But by the same token, if there’s a risk that [a serious harm] could happen if you have a screening test or a follow-up diagnostic test, then it’s a physician’s obligation to inform patients about what the risks of those procedures are,”
In the NCI-funded study, Dr. Doria-Rose and his colleagues looked at commonly used guidelines for breast, cervical, colorectal, lung, and prostate cancer screening to see whether various harms were mentioned and, if so, if they were described briefly or in detail.
Information on screening harms in those guidelines often fell short, the researchers found.
For example, some harms were not mentioned at all, while others were mentioned only briefly.
….the study looked at commonly used guidelines for breast, cervical, colorectal, lung, and prostate cancer screening to see whether various harms were mentioned and, if so, if they were described briefly or in detail.
Information on screening harms in those guidelines often fell short, the researchers found. For example, some harms were not mentioned at all, while others were mentioned only briefly.
The study was published September 27 in Annals of Internal Medicine.
The study results “bring attention to the inconsistency across guidelines,” said Louise Davies, M.D., a thyroid cancer surgeon at The Dartmouth Institute for Health Policy & Clinical Practice and Veterans Affairs Medical Center in White River Junction, Vermont.
“The analysis may allow different guideline bodies to compare themselves and identify areas they hadn’t previously considered,” said Dr. Davies, who wasn’t involved in the study.
“The analysis may allow different guideline bodies to compare themselves and identify areas they hadn’t previously considered,”…
Outline of the publication:
- Comparing the benefits and harms of cancer screening
- Evaluating US screening guidelines
- How often do screening harms happen?
- A need for greater transparency

To create a cancer screening guideline, a medical organization convenes a panel of experts to compare the benefits of a screening test with the harms.
The benefits tend to be narrowly defined as either preventing death from cancer or preventing a precursor (like a polyp in the colon) from turning into cancer, Dr. Doria-Rose explained.
But the potential harms of cancer screening are more complex and harder to measure, he said.
They run the gamut of physical, psychological, emotional, and financial effects. Plus, those harms can come not just from the screening tests themselves, but also from follow-up tests and treatments.
Some harms are more serious than others and might carry more weight in the comparison, Dr. Doria-Rose continued.
For instance, serious bleeding following a colonoscopy would be weighted more than the pinch of a blood draw for a PSA test.
Also, as many screening experts stress, most harms tend to occur during or soon after a person gets screened, while the benefits don’t show up until many years later.
So, when guideline developers compare the potential benefits of a screening test with its potential harms, “obviously it’s not an apples-to-apples kind of comparison,” he said.

Evaluating US screening guidelines
The researchers evaluated cancer screening guidelines from more than 10 medical organizations, including the US Preventive Services Task Force, the American Cancer Society, and National Comprehensive Cancer Network (NCCN).
They found that none of the guidelines had complete information on the potential harms of screening. Guidelines for prostate cancer screening were the most complete, whereas those for colorectal cancer screening were the least complete.
“
Certainly, a lack of high-quality research on the harms of screening contributes to this variation,” Russell Harris, M.D., M.P.H., and Linda Kinsinger, M.D., M.P.H., wrote in an editorial on the study.
Certainly, a lack of high-quality research on the harms of screening contributes to this variation,”
But the study also showed that reporting of harms was inconsistent even between guidelines for the same type of cancer.
For instance, some cervical cancer guidelines mentioned the potential for unnecessary diagnostic tests while others didn’t.
“We worry about a tendency [for guideline developers] to underrecognize the importance of harms,” Drs. Harris and Kinsinger wrote.
But the study also showed that reporting of harms was inconsistent even between guidelines for the same type of cancer. For instance, some cervical cancer guidelines mentioned the potential for unnecessary diagnostic tests while others didn’t.

How often do screening harms happen?
In agreement with earlier studies, the researchers also found that very few of the guidelines gave a clear idea of how many people typically experience each harm associated with a particular screening test.
Providing the frequency of a harm makes it easier for people to compare harms and benefits and make an informed decision, Dr. Doria-Rose explained.
In agreement with earlier studies, the researchers also found that very few of the guidelines gave a clear idea of how many people typically experience each harm associated with a particular screening test.
For example, according to one analysis, screening 10,000 women for breast cancer every year for 10 years starting at age 60 will prevent 43 deaths from breast cancer (88 women will still die from breast cancer despite getting screened).
It will also result in nearly 5,000 false positives that lead to nearly 1,000 unnecessary biopsies.
For example, according to one analysis, screening 10,000 women for breast cancer every year for 10 years starting at age 60 will prevent 43 deaths from breast cancer (88 women will still die from breast cancer despite getting screened).
It will also result in nearly 5,000 false positives that lead to nearly 1,000 unnecessary biopsies.
More research is needed to learn how frequently some screening harms happen, especially in community health care settings, Dr. Doria-Rose noted. That’s one area of focus for NCI’s PROSPR network, he added.
More research is needed to learn how frequently some screening harms happen, especially in community health care settings …
Finally, the researchers noted that while the benefits of screening were often calculated for multiple rounds of screening over many years, the guidelines almost never considered the harms of screening in the same cumulative way.
That makes the task of comparing benefits and harms like “comparing apple slices to [whole] oranges. We only have a piece of the picture,” Dr. Doria-Rose said.
Finally, the researchers noted that while the benefits of screening were often calculated for multiple rounds of screening over many years, the guidelines almost never considered the harms of screening in the same cumulative way.
There’s currently not enough research on the cumulative harms of cancer screening, Dr. Davies said.
More studies in this area would be “very important because it would provide balanced information for patients to make informed decisions,” she added.
There’s currently not enough research on the cumulative harms of cancer screening, Dr. Davies said.

A need for greater transparency
Based on their findings, the research team suggested two calls to action for guideline developers.
- “We’re encouraging [guideline developers] to do deeper dives before they update their guidelines the next time, to make sure that they’re really using the best possible evidence [on screening harms] to make their recommendations,” Dr. Doria-Rose said.
- The second is a call for greater transparency about how guideline developers make their recommendations.
“Be open about what harms you’re considering and what harms you’re not considering, and what benefits you’re considering and not considering, so that at least we know what the screening recommendations are based on,” he said.
Drs. Harris and Kinsinger also advocate for greater transparency. “Whose values does the panel use to balance benefits and harms?” they wrote.
For example, are the lives saved by screening valued more than preventing unnecessary biopsies?
Each guideline likely reflects “what the [panel of] clinicians values most from their own experience in treating the cancers in their field,” Dr. Davies noted.
But guidelines should also consider the values of the people who are getting screened, she said.
“I think there’s a role for improved representation by stakeholders who are not clinicians-patients, family members, people who’ve had both positive and negative screening experiences,” Dr. Davies continued.
Ultimately, many experts believe it’s important for each person to decide what matters most to them when considering getting screened.
Every individual should be able to “choose to follow those [guidelines] that apply values most similar to their own,” Drs. Harris and Kinsinger wrote.

BOX: Harms of Cancer Screening
All screening tests have potential harms. For more information, visit our Cancer Screening Overview page.
- Physical harm: Screening tests can cause minor physical harm like bruising or discomfort, as well as serious physical harm like tearing the colon during colon cancer screening.
- Radiation exposure: Some screening tests use low doses of radiation that can damage healthy cells.
- False-negative result: Screening tests sometimes miss an instance of cancer, which could lead people to skip going to the doctor when they have symptoms.
- False-positive result: Screening tests can suggest that cancer is there when it really isn’t. A false-positive result can cause anxiety and is usually followed by more tests and procedures, which also have risks.
- Overdiagnosis: Sometimes screening tests find cancers that are so small and slow-growing that they would never cause any symptoms or become life-threatening. But if people get treatment for these cancers, they are exposed to unnecessary side effects and costs.
- Psychological harm: Many people feel worried and stressed about getting ready for a screening test, waiting for the results, getting follow-up tests, and getting an inaccurate result.
- Incidental findings: Cancer screening tests might find an unrelated medical issue-such as finding an unrelated heart problem-and require follow up tests or procedures which also have risks.
Originally published at https://www.cancer.gov on November 23, 2022.
Names mentioned
Paul Doria-Rose, Ph.D., chief of NCI’s Healthcare Assessment Research Branch.
Louise Davies, M.D., a thyroid cancer surgeon at The Dartmouth Institute for Health Policy & Clinical Practice and Veterans Affairs Medical Center in White River Junction, Vermont.
Russell Harris, M.D., M.P.H., and Linda Kinsinger, M.D., M.P.H
REFERENCE PUBLICATION
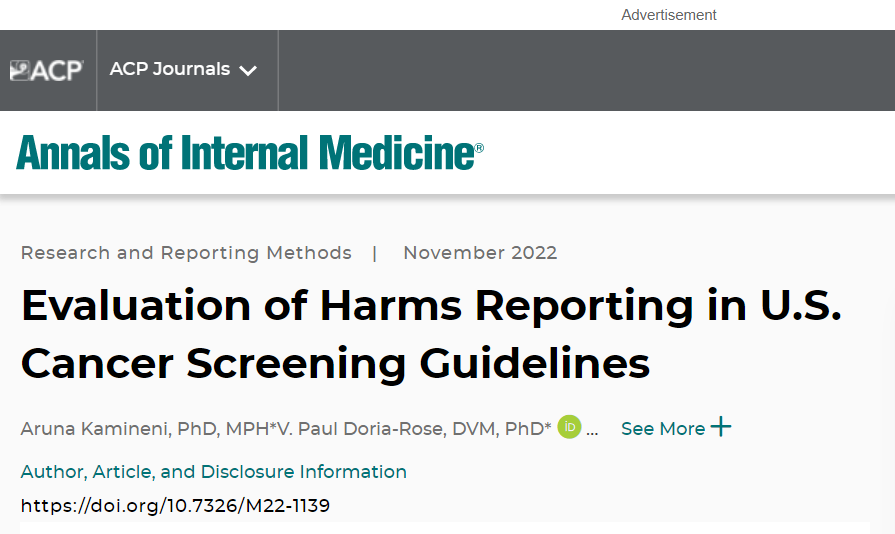
Annals of Internal Medicine
Aruna Kamineni, PhD, MPH*, V. Paul Doria-Rose, DVM, PhD*, Jessica Chubak, PhD, John M. Inadomi, MD, Douglas A. Corley, MD, PhD, Jennifer S. Haas, MD, MSc, Sarah C. Kobrin, PhD, MPH, Rachel L. Winer, PhD, Jennifer Elston Lafata, PhD, Elisabeth F. Beaber, PhD, MPH, Joshua S. Yudkin, MPH, Yingye Zheng, PhD, Celette Sugg Skinner, PhD, Joanne E. Schottinger, MD, Debra P. Ritzwoller, PhD, Jennifer M. Croswell, MD, MPH, and Andrea N. Burnett-Hartman, PhD, MPH
Background:
- Cancer screening should be recommended only when the balance between benefits and harms is favorable.
- This review evaluated how U.S. cancer screening guidelines reported harms, within and across organ-specific processes to screen for cancer.
Objective:
- To describe current reporting practices and identify opportunities for improvement.
Design:
- Review of guidelines.
Setting:
- United States.
Patients:
- Patients eligible for screening for breast, cervical, colorectal, lung, or prostate cancer according to U.S. guidelines.
Measurements:
- Information was abstracted on reporting of patient-level harms associated with screening, diagnostic follow-up, and treatment.
- The authors classified harms reporting as not mentioned, conceptual, qualitative, or quantitative and noted whether literature was cited when harms were described.
- Frequency of harms reporting was summarized by organ type.
Results:
- Harms reporting was inconsistent across organ types and at each step of the cancer screening process.
- Guidelines did not report all harms for any specific organ type or for any category of harm across organ types.
- The most complete harms reporting was for prostate cancer screening guidelines and the least complete for colorectal cancer screening guidelines.
- Conceptualization of harms and use of quantitative evidence also differed by organ type.
Limitations:
- This review considers only patient-level harms.
- The authors did not verify accuracy of harms information presented in the guidelines.
Conclusion:
- The review identified opportunities for improving conceptualization, assessment, and reporting of screening process–related harms in guidelines.
- Future work should consider nuances associated with each organ-specific process to screen for cancer, including which harms are most salient and where evidence gaps exist, and explicitly explore how to optimally weigh available evidence in determining net screening benefit.
- Improved harms reporting could aid informed decision making, ultimately improving cancer screening delivery.
Primary Funding Source:
- National Cancer Institute.