Health Transformation Institute (HTI)
Digital, Health and Care Transformation
Joaquim Cardoso MSc
Founder and Chief Researcher, Editor and Advisor
December 13, 2022
Key takeaways :
Heart Disease:
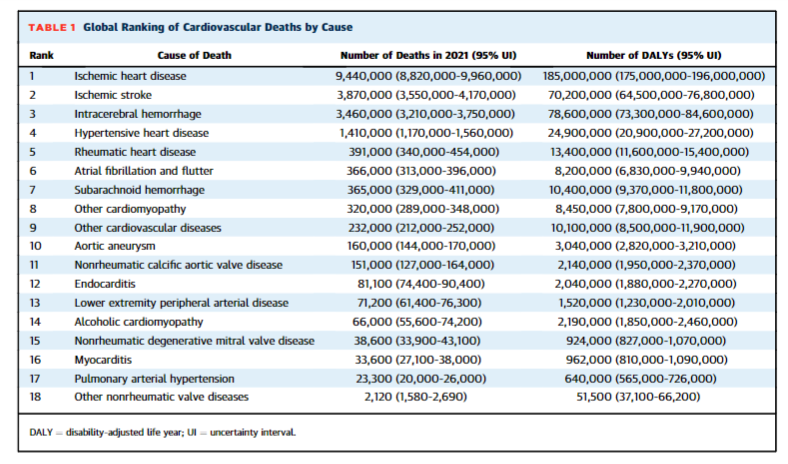
- Ischemic heart disease is the leading cause of cardiovascular death, accounting for 9.44 million deaths in 2021 and 185 million DALYs.
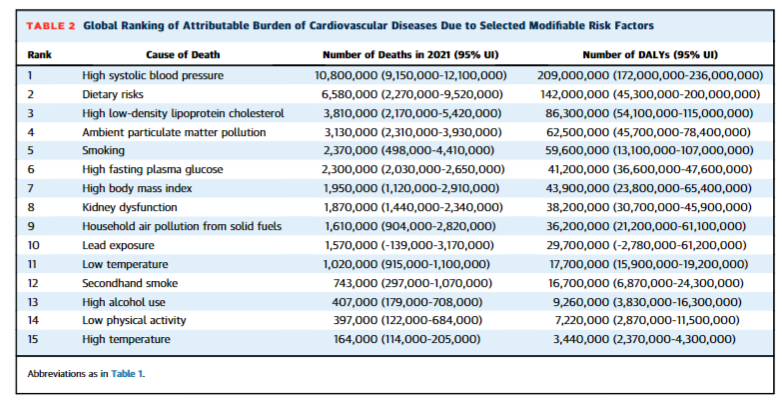
- High systolic blood pressure remains the leading modifiable risk factor for premature cardiovascular deaths, accounting for 10.8 million CV deaths and 11.3 million deaths overall in 2021.
- The all-cause DALYs due to high blood pressure were 2,770 per 100,000 people.
Dietary risks
- Dietary risks accounted for 6.58 million CV deaths and 8 million deaths overall in 2021.
- Dietary risks include food types that are under-consumed globally (fruits, vegetables, legumes, whole grains, nuts and seeds, milk, fiber, calcium, omega-3 fatty acids and poly unsaturated fatty acids) …
- … and over-consumed (red and processed meats, sugar-sweetened beverages, trans-fatty acids and sodium).
- All-cause DALYs due to dietary risks were 2,340 per 100,000 people.
Burden of Disease by Region
- Central Asia, Central Sub-Saharan Africa and Eastern Europe were the regions with the highest rates of CVD burden attributable to elevated systolic blood pressure.
- The regions with the highest rates of CVD burden attributable to dietary risk were Central Asia, Oceania and Eastern Europe.
- Central Asia had the highest age-standardized total CVD mortality at 516.9 deaths per 100,000.
- In contrast, high-income Asia Pacific had the lowest age-standardized total CVD mortality at 76.6 deaths per 100,000 people.
Improvements:
- Since 1990, Australasia had the largest percent reduction (64.2%) in age-standardized CVD per 100,000 out of all other regions.
- This percent decrease was highest in ischemic heart disease at 71.8%.
Infographic
- The GBD study is the ongoing effort of >8,000 collaborators around the world working to comprehensively characterize mortality and other health measures across 204 countries and territories.
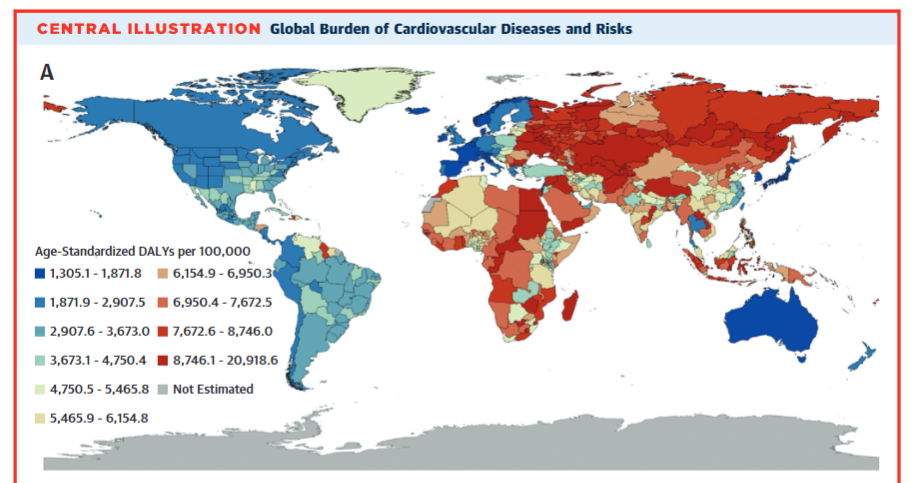
Central Illustration — Global Burden of Cardiovascular Diseases and Risks
ORIGINAL PUBLICATION

New report tracks latest trends in global cardiovascular health
Cardiovascular disease is leading cause of death worldwide; High blood pressure, high cholesterol, dietary risks and air pollution leading causes of cardiovascular disease worldwide
American Journal of Cardiology
December 12, 2022
Cardiovascular disease (CVD) remains the leading cause of death across the globe, according to a new “almanac”-style special issue of the Journal of the American College of Cardiology (JACC).
The issue looks at 18 specific cardiovascular conditions and 15 risk factors across 21 global regions to provide a broad view of the global burden of cardiovascular disease.
While CVD rates are high globally, Central Asia and Eastern Europe were estimated to have the highest rates of CVD mortality.
High blood pressure, high cholesterol, dietary risks and air pollution were the leading causes of CVD worldwide.
The Global Burden of Cardiovascular Diseases Collaboration is an alliance between JACC, the Institute for Health Metrics and Evaluation, and the National Heart, Lung, and Blood Institute.
Serving as an update to “ The Global Burden of Diseases, Injuries, and Risk Factors Study 2019,” the 2022 publication includes data from 204 countries and territories, highlighting the leading global modifiable cardiovascular risk factors, their contribution to disease burden and recent prevention advancements.
“We need to keep shining a light on the current state of cardiovascular health across the globe.
Cardiovascular health has a major impact on our quality of life and the health care system as a whole,” said Gregory A. Roth, MD, MPH, senior author of the paper and associate professor in the Division of Cardiology and director of the Program in Cardiovascular Health Metrics at the Institute for Health Metrics and Evaluation at the University of Washington. “Over 80% of cardiovascular disease is preventable.
With this update, we are measuring some alarming global trends and reviewing the current interventions that can help countries make good, evidence-based choices for their health systems.”
With this update, we are measuring some alarming global trends and reviewing the current interventions that can help countries make good, evidence-based choices for their health systems.”
This special report assessed deaths using vital and sample registration data and produced estimates for …
- … the 15 leading environmental (air pollution, household air pollution, lead exposure, low temperature, high temperature),
- metabolic (systolic blood pressure, LDL-cholesterol, body mass index, fasting plasma glucose, kidney dysfunction) and
- behavioral (dietary, smoking, secondhand smoke, alcohol use, physical activity) risks for cardiovascular diseases.
The CVD mortality rates are broken down by location, along with age, sex and time categories since 1990.
The report also looked at disability-adjusted life years (DALYs), the years of life lost due to premature mortality (YLLs), and years lived with disability (YLDs).
“It is truly exciting to see this multi-year Global Burden of Cardiovascular Diseases Collaboration culminate into a dedicated issue of the said Valentin Fuster, MD, PhD, an author of the paper, director of Mount Sinai Heart, physician-in-chief of The Mount Sinai Hospital and editor-in-chief of Journal to inform the global cardiovascular community JACC.
“This issue focuses both on the modifiable risk factors, as well as the global cardiovascular disease and death rates in 21 regions across the world.”
“This issue focuses both on the modifiable risk factors, as well as the global cardiovascular disease and death rates in 21 regions across the world.”
“This visual atlas serves as a timely reminder about the importance of modifiable risk factors for heart disease, like high blood pressure,” said George A. Mensah, MD, an author of the paper and director of the Center for Translation Research and Implementation Science at the National Heart, Lung, and Blood Institute.
“Deaths due to hypertension have steadily increased in the U.S. for the past 20 years, which mirrors trends in other regions and leaves researchers eager to find practical and innovative solutions.”
“Of really great concern is the finding that high blood pressure control rates have progressively declined in the U.S. over the last decade,” he added.
Originally published at https://www.healthdata.org on December 12, 2022.
Names mentioned
Gregory A. Roth, MD, MPH, senior author of the paper and associate professor in the Division of Cardiology and director of the Program in Cardiovascular Health Metrics at the Institute for Health Metrics and Evaluation at the University of Washington
Valentin Fuster, MD, PhD, an author of the paper, director of Mount Sinai Heart, physician-in-chief of The Mount Sinai Hospital and editor-in-chief of Journal to inform the global cardiovascular community JACC.
George A. Mensah, MD, an author of the paper and director of the Center for Translation Research and Implementation Science at the National Heart, Lung, and Blood Institute
REFERENCE PUBLICATION
The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health
Journal of American College of Cardiology
Muthiah Vaduganathan , George A. Mensah, Justine Varieur Turco, Valentin Fuster, Gregory A. Roth
December 2022
Introduction
Cardiovascular diseases (CVDs) have collectively remained the leading causes of death worldwide and substantially contribute to loss of health and excess health system costs.1,2
The Global Burden of Diseases, Injuries, and Risk Factors (GBD) Study has tracked trends in death and disability since 1990 and has provided an updated perspective on the status of cardiovascular health globally, regionally, and nationally.
The GBD Study also measures the burden of disease attributable to 88 risk factors for disease.
While understanding the underlying physiologic causes of death is important, rigorously evaluating upstream drivers of disease provides additional strategies to guide public policy.
These “actual causes of death”3,4 reflect modifiable, nongenetic risk factors that cause these diseases.
Their role can be estimated by accounting for risk factor prevalence and exposure, strength of relative risk associations with health outcomes, and cause-specific mortality.
With this awareness at the forefront, the Global Burden of Cardiovascular Diseases Collaboration, an alliance between the Institute for Health Metrics and Evaluation, the National Heart, Lung, and Blood Institute, and the Journal of the American College of Cardiology (JACC), was launched in 2020.
Since then, this collaboration has delivered publications as well as a 5-part region-specific digital series, focused on East Asia, North America, South America, Sub-Saharan Africa, and Western Europe, highlighting their distinct epidemiology.
Knowing that the global cardiovascular clinical and research communities desire these data with more frequency, it is our intent to publish results annually.
In this update, we provide a lens on the global, regional, and national burden of CVDs and risk factors.
This 2022 dedicated issue of JACC highlights 21 global regions, each with 2 pages of data presented in a graphic-rich almanac style.
In this review, we also highlight the leading global modifiable cardiovascular risk factors, their contribution to disease burden, and recent advances related to their control and prevention.
Attention is paid to how these metabolic, behavioral, and environmental risks may be addressed through evidence-based clinical care and health policy.

Global Burden of Disease Study Methods
The GBD study is the ongoing effort of >8,000 collaborators around the world working to comprehensively characterize mortality and other health measures across 204 countries and territories.
As described in-depth separately, GBD deploys a standardized, replicable approach that organizes these data at global, regional, national, and subnational levels stratified by age and sex.
Estimates of several summary epidemiological measures are produced, including composite measures such as disability-adjusted life years (DALYs).
DALYs are the sum of years of life lost due to premature mortality and years lived with disability (based on standardized disability weights for each health state).
Deaths were identified and categorized using vital registration data via International Classification of Disease codes or household mortality surveys. CVD incidence and prevalence were captured with structured clinical case definitions.
Population representative surveys and surveillance data were leveraged to evaluate risk factor exposures.
Population-attributable fractions were calculated for each risk factor and a specific disease outcome by integrating risk exposures, relative risks between a risk factor and outcome (based on meta-analyses), and theoretical minimum risk levels for each risk-outcome pairing.5,6
Statistical methods are applied to improve standardization and comparability of data, and health measure estimates are provided with uncertainty intervals (UIs) for all locations and years.
Detailed methods have been reported separately.7–9 DALY rates are all-ages unless stated otherwise.
All input data sources can also be searched via this database. Reporting is in accordance with Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) guidelines.10
The University of Washington Institutional Review Board Committee approved the Global Burden of Diseases, Injuries, and Risk Factors Study (STUDY00009060).

Leading Modifiable Global Cardiovascular Risk Factors
The GBD Study has produced estimates for the following leading environmental, metabolic, and behavioral risks for CVDs:
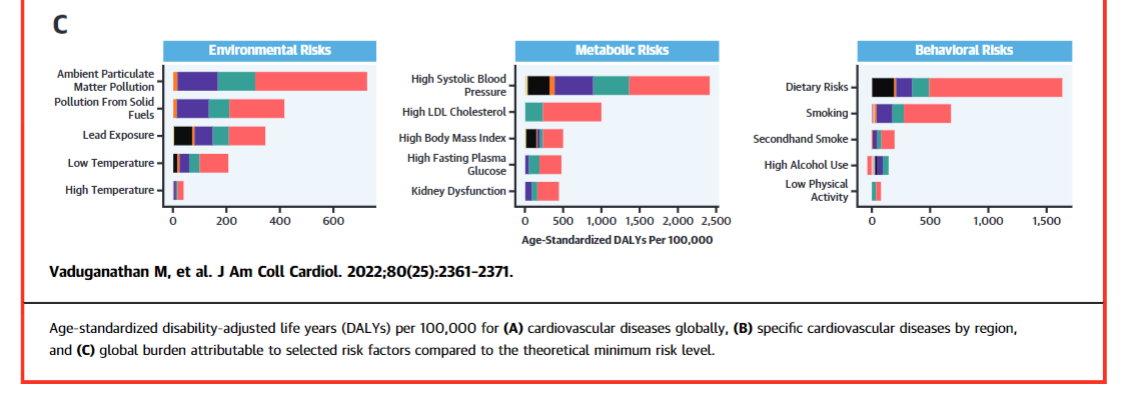
ambient particulate matter air pollution, household air pollution from solid fuels, lead exposure, low or high temperature, high systolic blood pressure, high low-density lipoprotein cholesterol (LDL-C), high body mass index (BMI), high fasting plasma glucose, kidney dysfunction, dietary risks, tobacco smoking, secondhand tobacco smoke, high alcohol use, and low physical activity (Central Illustration).
In this review, we report on the burden due to these risk factors and recent advances in addressing them to help guide the development of research goals and population health strategies.
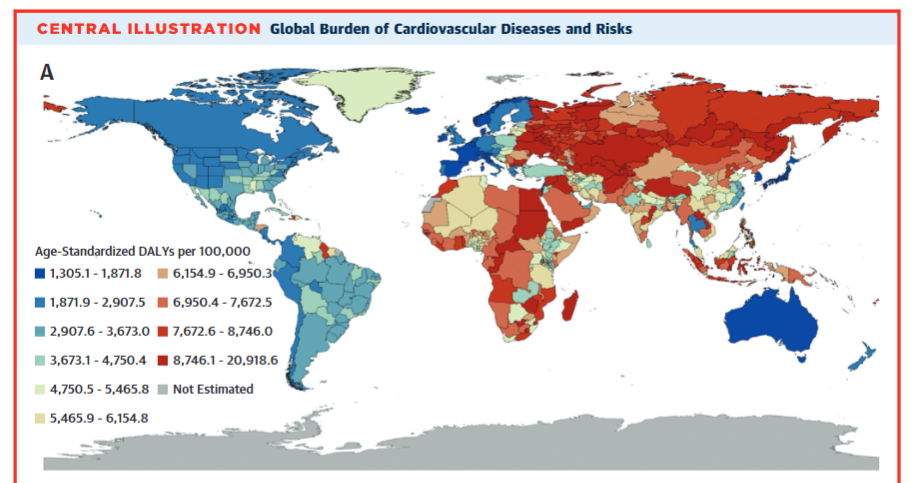
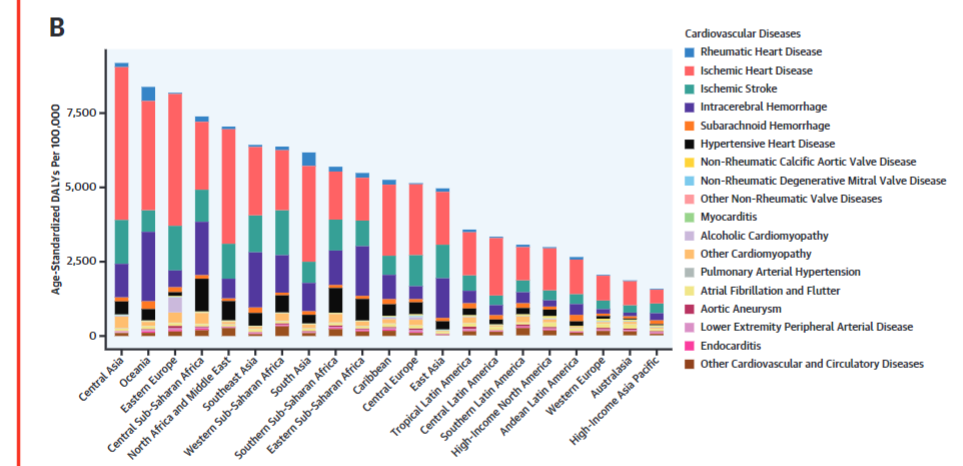
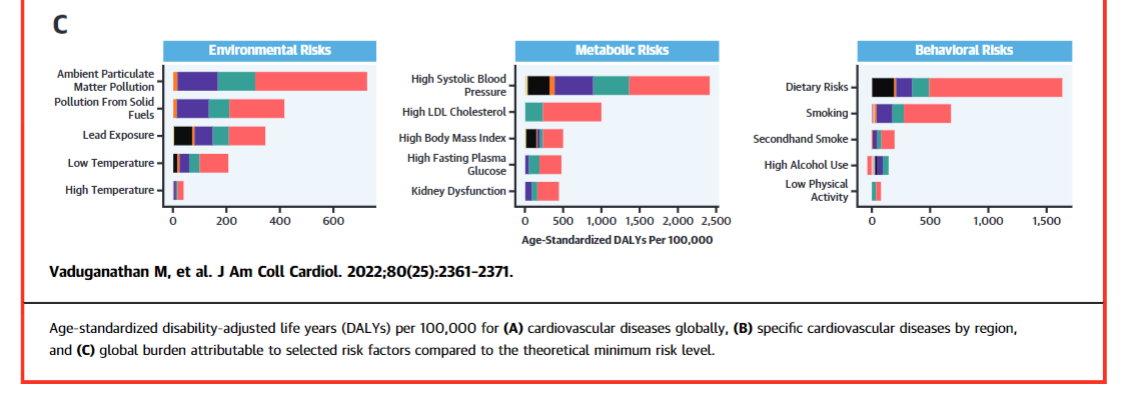
Central Illustration — Global Burden of Cardiovascular Diseases and Risks
Age-standardized disability-adjusted life years (DALYs) per 100,000 for (A) cardiovascular diseases globally, (B) specific cardiovascular diseases by region, and © global burden attributable to selected risk factors compared to the theoretical minimum risk level.
1.High blood pressure
2.Dietary risks
3.High LDL-C
4.Air pollution
5.Tobacco
6.High body mass index
7.High fasting plasma glucose
8.Kidney dysfunction
9.Lead
10.Nonoptimal temperatures
11.Low physical activity
12.High alcohol use

1.High blood pressure
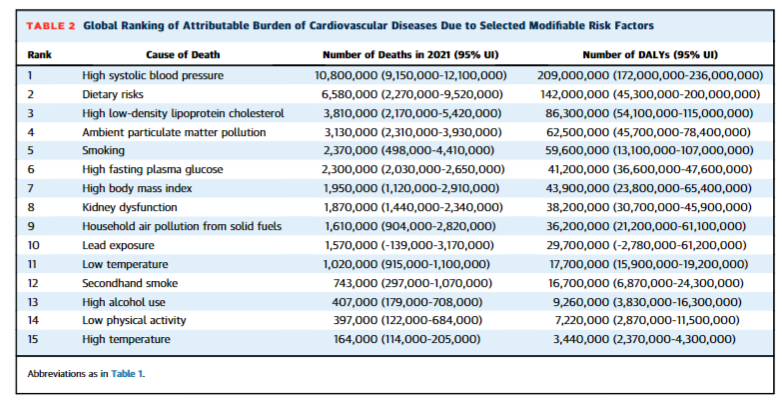
High systolic blood pressure remains the leading modifiable risk factor globally for attributable premature cardiovascular deaths, accounting for 10.8 million (95% CI: 9.15–12.1 million) cardiovascular deaths and 11.3 million (95% CI: 9.59–12.7 million) deaths overall in 2021, and has been particularly linked to ischemic heart disease and stroke-related deaths6 (Tables 1 and 2).
In 2021, the all-cause DALYs due to high blood pressure were 2,770 per 100,000 (95% CI: 2,310–3,160 per 100,000).
Randomized clinical trials have established that more intensive blood pressure targets reduced cardiovascular events compared with more conventional or standard blood pressure control in middle-aged and older adults.11–13
More modest blood pressure control is incrementally beneficial even among adults aged ≥80 years.14
Blood pressure lowering appears to be a particularly important strategy to delay progression to incident heart failure in at-risk individuals.
Intensive blood pressure control is projected to extend life expectancy by up to 3 years when initiated in middle age,15 and antihypertensive treatment optimization appears cost effective at common willing-to-pay thresholds.16
Taken together, these data underscore the importance of public health strategies to promote early screening, detection, and treatment of hypertension.
Taken together, these data underscore the importance of public health strategies to promote early screening, detection, and treatment of hypertension.
Even after diagnosis, traditional step-wise sequencing of prescribing pharmacotherapies may lead to treatment inertia and slow early effective blood pressure control.
Even after diagnosis, traditional step-wise sequencing of prescribing pharmacotherapies may lead to treatment inertia and slow early effective blood pressure control.
Upfront combination of 4 drugs as a single pill at fixed ultra-low doses (irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, and bisoprolol 2.5 mg) was shown to achieve earlier and sustained blood pressure lowering compared with starting with 1 drug (a common current practice).17
Upfront combination of 4 drugs as a single pill at fixed ultra-low doses (irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, and bisoprolol 2.5 mg) was shown to achieve earlier and sustained blood pressure lowering compared with starting with 1 drug (a common current practice
Simplification of strategies of blood pressure control may improve its implementation in practice and facilitate generalizability across settings.
In light of existing inequities and unequal access to care, alongside pharmacological approaches, public health measures may be needed to affect population-level blood pressure control.
Community-based interventions, including pharmacist-led management and health promotion delivered at barbershops and beauty salons, represent successful18,19 and highly cost-effective strategies20 to address health inequities in blood pressure control.
Community-based interventions, including pharmacist-led management and health promotion delivered at barbershops and beauty salons, represent successful18,19 and highly cost-effective strategies20 to address health inequities in blood pressure control.
With an aging and expanding global population, the number of people living with suboptimal blood pressure control is increasing.
Multilevel pharmacological and nonpharmacological interventions are needed to address the risks of high blood pressure on health.
With an aging and expanding global population, the number of people living with suboptimal blood pressure control is increasing.
Multilevel pharmacological and nonpharmacological interventions are needed to address the risks of high blood pressure on health.
Table 1Global Ranking of Cardiovascular Deaths by Cause
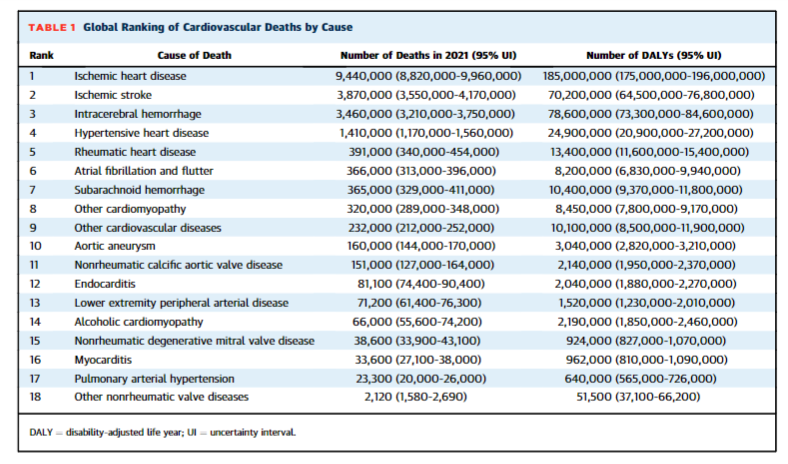
Table 2Global Ranking of Attributable Burden of Cardiovascular Diseases Due to Selected Modifiable Risk Factors

2.Dietary risks
Dietary risks accounted for 6.58 million (95% CI: 2.27–9.52 million) cardiovascular deaths and 8 million (95% CI: 3.03–11.8 million) deaths overall in 2021.
This estimate included food types that are underconsumed globally (fruits, vegetables, legumes, whole grains, nuts and seeds, milk, fiber, calcium, omega-3 fatty acids from seafood, and polyunsaturated fatty acids) …
… or overconsumed (red meat, processed meat, sugar-sweetened beverages, trans-fatty acids, and sodium).
In 2021, the all-cause DALYs due to dietary risks were 2,340 per 100,000 (95% CI: 836–3,380 per 100,000).
Excess dietary sodium is a major driver of hypertension in many countries, and modest dietary sodium restriction by 3 grams/day has been projected to avert cardiovascular events and reduce deaths in a cost-saving manner, with benefits projected in all population segments.21
A report from the Health and Medicine Division of National Academies of Sciences, Engineering, and Medicine identified that reductions in lowering of sodium content in the food supply was a critical step to reaching dietary intake goals.22
… reductions in lowering of sodium content in the food supply was a critical step to reaching dietary intake goals
The U.S. Food and Drug Administration (FDA) has recently announced voluntary sodium reduction goals for average as well as upper bounds for commercially processed, packaged, and prepared foods.23
In a recent cluster-randomized trial of >20,000 high-risk Chinese adults across 600 rural villages in China, the use of a salt substitute (with lower sodium levels and higher potassium levels) reduced stroke, major adverse cardiovascular events, and death.24
In a recent cluster-randomized trial of >20,000 high-risk Chinese adults across 600 rural villages in China, the use of a salt substitute (with lower sodium levels and higher potassium levels) reduced stroke, major adverse cardiovascular events, and death.
The PREDIMED (Prevención con Dieta Mediterránea) trial remains one of the few high-quality trials of dietary interventions that established the role of the Mediterranean diet (supplementing with extra-virgin olive oil or nuts) in reducing major adverse cardiovascular events among individuals at high cardiovascular risk in Spain.25
Unfortunately, diets like the Mediterranean diet inclusive of moderate intakes of fish and poultry may be expensive or unavailable to much of the global population.
Multifaceted programs including focused media campaigns may promote consumption of healthier foods.26
Unfortunately, diets like the Mediterranean diet inclusive of moderate intakes of fish and poultry may be expensive or unavailable to much of the global population.
Multifaceted programs including focused media campaigns may promote consumption of healthier foods.26
Consumption of sugar-sweetened beverages has been rapidly increasing in recent years, and has been closely linked with adverse weight trajectories, poor nutrition, and higher risks of cardiometabolic illness.27
Sugar-sweetened beverages are directly marketed toward children and adolescents, and are consumed in high density in areas of poverty and greater food insecurity.
Taxation of sugared beverages has been proposed and implemented in various countries, which has been projected to reduce calorie consumption and body weight.28
Taxation of sugared beverages has been proposed and implemented in various countries, which has been projected to reduce calorie consumption and body weight
In 2014, Mexico implemented an excise tax (1 peso per liter) on sugar-sweetened beverages, which subsequently increased prices of these products.
Observational studies demonstrated that there was a modest early and sustained decline in purchases of these taxed beverages with substitution for other untaxed beverages.29,30
The FDA in 2015 determined that partially hydrogenated oils (a major source of trans-fats) are no longer “generally recognized as safe,” which greatly reduced artificial trans-fats in the food supply.
These examples suggest that public policy, when implemented, has the potential to influence population-level diet quality.

3.High LDL-C
Elevated LDL-C has persisted as a leading modifiable risk factor and is one of the most closely linked markers of atherosclerotic CVD.
In 2021, 3.81 million (95% CI: 2.17–5.42 million) cardiovascular deaths and 3.81 million (95% CI: 2.17–5.42 million) deaths overall were attributed to elevated LDL-C levels.
In 2021, the all-cause DALYs due to high LDL-C were 1,090 per 100,000 (95% CI: 685–1,460 per 100,000).
Exposure to lower cumulative LDL-C levels in young and middle-aged adults has been associated with reduced long-term cardiovascular risk,31 bringing “cholesterol-years” as a marker of atherosclerotic burden into focus as a target for cardiovascular prevention.32
Exposure to lower cumulative LDL-C levels in young and middle-aged adults has been associated with reduced long-term cardiovascular risk,31 bringing “cholesterol-years” as a marker of atherosclerotic burden into focus as a target for cardiovascular prevention.32
Statins have represented the cornerstone of primary and secondary prevention of CVDs.
Statins have represented the cornerstone of primary and secondary prevention of CVDs.
Sequential advances in discovery science have identified other effective classes of lipid-lowering therapies that lower LDL-C and positively affect cardiovascular health (ezetimibe and proprotein convertase subtilisin/kexin type 9 [PCSK9] serine protease inhibitors).
The incremental efficacy of use of powerful lipid-lowering strategies without apparent safety signals even at very low LDL-C has created a “race to the bottom.”33
There is increasing interest in early combination lipid-lowering management approaches among very–high-risk patients.34
The recognition of incomplete adherence and longitudinal lifetime risk faced among those with inadequate LDL-C control have prompted the development of more durable, long-term solutions to lipid management.
Inclisiran, a small interfering ribonucleic acid, inhibits the translation of PCSK9, durably lowers LDL-C, and can be administered via subcutaneous injection every 6 months. Inclisiran is now approved by the FDA and the European Medicines Agency, and is being tested to lower cardiovascular risk in primary and secondary prevention settings.
Early phase data in primates have demonstrated that in vivo clustered regularly interspaced short palindromic repeats (CRISPR) base editing of PCSK9 may lower cholesterol levels long term, potentially even over a lifetime.35
This “vaccine” approach to atherosclerosis promises to circumvent adherence challenges in clinical practice.
In a pioneering agreement between Novartis and England’s National Health Service, ∼300,000 high-risk patients with established CVD are expected to be treated with inclisiran under a population health management approach.36
In a pioneering agreement between Novartis and England’s National Health Service, ∼300,000 high-risk patients with established CVD are expected to be treated with inclisiran under a population health management approach.36
Similar disruptive and innovative health system–wide implementation approaches may lead to improved lipid management globally; however, newer lipid-lowering strategies will remain expensive and inaccessible in the near-term while statin pharmacotherapy remains cost-effective and widely available.37
Similar disruptive and innovative health system–wide implementation approaches may lead to improved lipid management globally; however, newer lipid-lowering strategies will remain expensive and inaccessible in the near-term while statin pharmacotherapy remains cost-effective and widely available.37

4.Air pollution
Air pollution in the forms of ambient particulate matter with an aerodynamic diameter smaller than 2.5 μm (PM2.5) and household air pollution (HAP) from cooking fuels represents the leading environmental risk factor for premature CVD and mortality.
In 2021, 4.75 million (95% CI: 3.76–5.58 million) cardiovascular deaths and 8.54 million (95% CI: 7.35–9.71 million) deaths overall were attributable to air pollution.
In 2021, 4.75 million (95% CI: 3.76–5.58 million) cardiovascular deaths and 8.54 million (95% CI: 7.35–9.71 million) deaths overall were attributable to air pollution.
In 2021, the all-cause DALYs due to air pollution were 2,990 per 100,000 (95% CI: 2,510–3,500 per 100,000).
Heavy PM2.5 pollution events have been closely linked with near-term risks of acute cardiovascular hospitalizations in a dose-dependent and duration-dependent manner.38
This attendant cardiovascular risk appears to extend even to very low levels, even below standards set by the World Health Organization (WHO).39
Some progress has been observed in reductions in ambient PM2.5 concentrations in North America and Europe related to effective air quality management and regulation, and this has in turn been linked to favorable health benefits.40
However, levels remain above the WHO’s Annual Air Quality Guideline for PM2.5 for >90% of the world’s population.41,42
Broad coalitions between governmental entities and environmental agencies are needed to promote awareness of the adverse health consequences of air pollution and to facilitate effective solutions.
Broad coalitions between governmental entities and environmental agencies are needed to promote awareness of the adverse health consequences of air pollution and to facilitate effective solutions.
There is no currently accepted global standard to communicate risk associated with various air pollution levels.
With increased access to high-quality air pollution monitoring data with greater resolution, there is an unmet need for a harmonized global platform to standardize reporting, alerts, and mitigation strategies.
In parallel, as summarized by a recent American Heart Association scientific statement, practical personalized approaches to attenuate the health consequences of PM2.5 can be considered.43
HAP, driven by use of nonrenewable solid fuels in traditional household stoves, represents an important contributor to adverse air quality worldwide.
In Rwanda, a pellet and fan micro-gasification cooking system was introduced by a for-profit social benefit company that represents a test case for innovative solutions in improving the supply of sustainable clean fuels even in low-resource settings.44
In Rwanda, a pellet and fan micro-gasification cooking system was introduced by a for-profit social benefit company that represents a test case for innovative solutions in improving the supply of sustainable clean fuels even in low-resource settings
Improving access to clean energy with lesser emissions and more efficient cooking approaches remain key global priorities to tackling air pollution.
Improving access to clean energy with lesser emissions and more efficient cooking approaches remain key global priorities to tackling air pollution.
The coronavirus disease-2019 (COVID-19) pandemic resulted in global reductions of air pollution secondary to reductions in road traffic and air travel.45
While challenging to replicate as a public health strategy, this experience has reinforced the feasibility of large-scale actions to combat adverse health consequences of air pollution.
The coronavirus disease-2019 (COVID-19) pandemic resulted in global reductions of air pollution secondary to reductions in road traffic and air travel.
While challenging to replicate as a public health strategy, this experience has reinforced the feasibility of large-scale actions to combat adverse health consequences of air pollution.

5.Tobacco
Tobacco is the fifth leading actual cause of cardiovascular death, and in 2021, 3.01 million (95% CI: 1.24–4.96 million) cardiovascular deaths and 7.61 million (95% CI: 3.5–11.7 million) deaths overall were attributable to tobacco use.
Tobacco is the fifth leading actual cause of cardiovascular death, and in 2021, 3.01 million (95% CI: 1.24–4.96 million) cardiovascular deaths and 7.61 million (95% CI: 3.5–11.7 million) deaths overall were attributable to tobacco use.
In 2021, the all-cause DALYs due to tobacco were 2,460 per 100,000 (95% CI: 1,140–3,760 per 100,000).
The WHO target has been set to reduce the prevalence of tobacco smoking by one-third by 2025, and its achievement is projected to prevent a significant number of attributable and preventable deaths to tobacco.46
The WHO target has been set to reduce the prevalence of tobacco smoking by one-third by 2025, and its achievement is projected to prevent a significant number of attributable and preventable deaths to tobacco
Implementation of the WHO MPOWER program, a suite of 6 data-driven strategies (monitoring use, protecting people, offering help, warning, enforcing bans, and raising taxes), has empirically been associated with lower tobacco use.
For instance, in Turkey, after initial adoption in 2008 and high degree of achievement of all MPOWER measures, smoking and smoking-related illnesses have declined.47 Comprehensive tobacco control programs have been implemented worldwide incorporating price and nonprice interventions that have successfully promoted smoking cessation, reduced per-person consumption, and reduced new initiation.48
Systematic reviews of taxation approaches have shown consistent inverse associations between tobacco taxes and consumption.49
Systematic reviews of taxation approaches have shown consistent inverse associations between tobacco taxes and consumption.
Other strategies that have proven effective include restricting or banning tobacco-related advertising via the media or in public places (as is the case in many countries worldwide).
Other strategies that have proven effective include restricting or banning tobacco-related advertising via the media or in public places (as is the case in many countries worldwide).
In 2011, Australia further required all brand imagery to be excluded from packaging of tobacco products in favor of plain labels.
This strategy appeared successful at reducing consumption50 and has since been adopted in other countries.
Mobile health technologies may also play a role in limiting risks of global tobacco burden.
Mobile health technologies may also play a role in limiting risks of global tobacco burden.
India launched a text-based mCessation program delivered in >10 different languages connecting specialists with people seeking to quit. Many countries have integrated national quit lines available for individuals seeking counseling.
In the Republic of Korea, quit lines have been covered by the National Health Insurance Service, smoking cessation initiatives were extended to include a “quit bus” to help marginalized individuals quit, and regional smoking cessation centers were established. Improved primary care–driven counseling has also been a priority.
In Ecuador, primary care physicians were trained to integrate brief tobacco interventions into routine practice.
Harm reduction strategies, including the use of electronic cigarettes, have been highly contentious.
Harm reduction strategies, including the use of electronic cigarettes, have been highly contentious.
The FDA has authorized the first electronic cigarettes, recognizing that aerosol composition may be less toxic than regular cigarettes, with a hope that this may provide an alternative to allow current cigarette smokers to curb or substitute use.
The health impact of this authorization is as yet uncertain, but the FDA has imposed media restrictions on advertising of these products to limit excess exposure of these products to youth.

6.High body mass index
Obesity is highly prevalent worldwide, closely associated with multiple health risks, and directly contributes to the pathogenesis and progression of CVD.51
In 2021, 1.95 million (95% CI: 1.12–2.91 million) cardiovascular deaths and 3.7 million (95% CI: 1.97–5.49 million) deaths overall were attributable to elevated BMI.
In 2021, 1.95 million cardiovascular deaths and 3.7 million deaths overall were attributable to elevated BMI.
In 2021, the all-cause DALYs due to high BMI were 1,560 per 100,000 (95% CI: 711–2,380 per 100,000).
Medical weight loss therapies have evolved in recent years.
Glucagon-like peptide-1 receptor agonists and dual incretin agonists represent safe and effective options to reduce body weight and potentially protect the cardiovascular system, a hypothesis that is currently being tested.
Metabolic surgery has similarly matured to afford substantial weight loss that is durable over time and may have ancillary health benefits including improved glycemic control and remission of diabetes in some.52
Medical weight loss therapies have evolved in recent years.
Yet, in most global settings, the prevention and treatment of obesity centers on lifestyle modification, dietary interventions, and improvements in physical activity.
Yet, in most global settings, the prevention and treatment of obesity centers on lifestyle modification, dietary interventions, and improvements in physical activity.
Large-scale population-based prevention efforts are needed to construct an environment conducive to healthy behaviors, as has been done previously in the Finnish North Karelia Project.53
Similarly, community-based health promotion and intensive lifestyle management interventions may have durable impact on cardiometabolic health long-term; for instance, the Diabetes Prevention Program has been shown to have “legacy” effects in preventing diabetes even after 20 years.54
Early, comprehensive programs, such as the SI! Program,55 that can be embedded in schools, have been demonstrated to influence childhood behaviors and cardiovascular health trajectories.56
Early, comprehensive programs, such as the SI! Program,55 that can be embedded in schools, have been demonstrated to influence childhood behaviors and cardiovascular health trajectories.56

7.High fasting plasma glucose
High fasting glucose tracks closely with high burden of prediabetes, diabetes, and obesity worldwide.
In 2021, 2.30 million (95% CI: 2.03–2.65 million) cardiovascular deaths and 5.4 million (95% CI: 4.6–6.11 million) deaths overall were attributable to elevated fasting plasma glucose.
In 2021, 2.30 million cardiovascular deaths and 5.4 million deaths overall were attributable to elevated fasting plasma glucose.
In 2021, the all-cause DALYs due to high fasting plasma glucose were 1,910 per 100,000 (95% CI: 1,620–2,200 per 100,000).
Population strategies to improve glycemic risk overlap substantially with approaches to other primary ris
Population strategies to improve glycemic risk overlap substantially with approaches to other primary risk factors including low physical activity and adverse dietary profiles.
Scientific progress over the last decade has identified 2 disease-modifying therapeutic classes (the sodium-glucose co-transporter-2 [SGLT-2] inhibitors and the glucagon-like peptide-1 receptor agonists) that prevent cardiovascular complications and kidney disease progression in patients with diabetes.
In addition, continuous glucose monitoring has been introduced to minimize glycemic excursions and improve precision of glycemic control.
Dissemination and integration of these tools and therapies have been misaligned with risk, giving rise to a “treatment-risk paradox” in which high-risk older persons, Black individuals, or those who are uninsured or underinsured are less likely to be treated with evidence-based therapies.57
In addition, continuous glucose monitoring has been introduced to minimize glycemic excursions and improve precision of glycemic control.
Dissemination and integration of these tools and therapies have been misaligned with risk …
Furthermore, 100 years after the discovery of insulin, this essential treatment for many living with diabetes is inaccessible or unaffordable.58
Furthermore, 100 years after the discovery of insulin, this essential treatment for many living with diabetes is inaccessible or unaffordable.
Recently, the SGLT-2 inhibitors and long-acting insulin analogues were added to the WHO Essential Medicines Lists.
As the SGLT-2 inhibitors lack generic options in many countries, it has been recommended that the WHO work with the Medicines Patent Pool to facilitate access to these therapies in low- and middle-income countries by encouraging generic manufacturing and new formulations. 59
As the SGLT-2 inhibitors lack generic options in many countries, it has been recommended that the WHO work with the Medicines Patent Pool to facilitate access to these therapies in low- and middle-income countries by encouraging generic manufacturing and new formulations.
Microsimulation analyses have supported reasonable price targets to pursue during negotiations for incorporation in national formularies of low- and middle-income countries.60
However, even beyond expanding evidence-based care to those with known diabetes, increased efforts are needed to reach the large population with undiagnosed diabetes, which is estimated to be especially high in low- and middle-income countries.61

8.Kidney dysfunction
In 2021, 1.87 million (95% CI: 1.44–2.34 million) cardiovascular deaths and 3.47 million (95% CI: 2.93–4.00 million) deaths overall were attributable to reduced kidney function.
In 2021, 1.87 million cardiovascular deaths and 3.47 million deaths overall were attributable to reduced kidney function.
In 2021, the all-cause DALYs due to kidney dysfunction were 1,040 per 100,000 (95% CI: 935–1,180 per 100,000).
Patients who ultimately progress to end-stage kidney disease requiring dialysis face reduced health-related quality of life and heightened risk of death while contributing substantially to increased health system costs.
Unfortunately, a large number of people do not have access to necessary renal replacement therapy, with amplified treatment gaps in low- and middle-income countries.62
Unfortunately, a large number of people do not have access to necessary renal replacement therapy, with amplified treatment gaps in low- and middle-income countries
CVD is the most frequent mode of death, even in the large proportion of patients with earlier stages of chronic kidney disease (CKD).
CVD is the most frequent mode of death, even in the large proportion of patients with earlier stages of chronic kidney disease (CKD).
In those with established CKD especially in the presence of proteinuria, the use of renin-angiotensin system inhibitors, SGLT-2 inhibitors, and the nonsteroidal mineralocorticoid receptor agonist finerenone has been shown to not only reduce risk of kidney disease progression but also lower rates of cardiovascular events in this population.
The SGLT-2 inhibitor dapagliflozin was shown to be the first therapy to reduce risk of death in patients living with CKD.63
The SGLT-2 inhibitor dapagliflozin was shown to be the first therapy to reduce risk of death in patients living with CKD.63
Expanding global access to highly effective pharmacotherapies for CKD remains a substantial challenge.
Due to incomplete screening and diagnosis, CKD is largely undetected worldwide.
Population-level screening for CKD is estimated to be cost-effective in countries to allow early initiation of risk-reduction strategies.64
Global surveillance programs for CKD are needed to improve mapping of disease burden to better target efforts.
Global surveillance programs for CKD are needed to improve mapping of disease burden to better target efforts.
In recent years, cases of “CKD of unknown cause” have increased among agricultural workers in some regions of the world, notably in parts of Latin America.
The exact mechanism underlying this illness is uncertain but is thought to potentially be related to toxins (such as pesticide exposure), heat exposure, or potential infectious agents.65
In recent years, cases of “CKD of unknown cause” have increased among agricultural workers in some regions of the world, notably in parts of Latin America.
The exact mechanism underlying this illness is uncertain but is thought to potentially be related to toxins (such as pesticide exposure), heat exposure, or potential infectious agents.

9.Lead
Lead exposure remains a silent but major contributor to CVD mortality and health loss.66
Lead is an underrecognized environmental factor that is linked with hypertension, stroke, coronary artery disease, peripheral artery disease, and other CVDs.
In 2021, 1.57 million (95% CI: –0.139 to 3.17 million) cardiovascular deaths and 1.64 million (95% CI: –0.144 to 3.32 million) deaths overall were attributed to environmental lead exposure.
In 2021, 1.57 million (95% CI: –0.139 to 3.17 million) cardiovascular deaths and 1.64 million (95% CI: –0.144 to 3.32 million) deaths overall were attributed to environmental lead exposure.
In 2021, the all-cause DALYs due to other environmental risks were 451 per 100,000 (95% CI: –3.86 to 875 per 100,000).
Consistent with these findings, Brown et al67 estimated that substantial decreases in environmental lead exposure may result in large population health benefits in adults.
In fact, they estimated that as much as 6% to 46% of the decreased CVD-related mortality rate from 1999 to 2014 could be attributable to reductions in blood lead levels.67
There is biological plausibility for the association of lead exposure, blood lead levels, and adverse CVD outcomes.
Underlying mechanisms may include derangements in blood pressure and lipid levels, and telomere shortening, even at low blood levels of lead.68
Comprehensive programs to reduce the adverse risks associated with lead exposure have been projected to avert CVDs.69
Comprehensive programs to reduce the adverse risks associated with lead exposure have been projected to avert CVDs

10.Nonoptimal temperatures
Nonoptimal ambient temperatures are important contributors to global, regional, and national mortality burdens.
Although widespread attention is often paid to the mortality burden of extreme cold or hot temperatures, milder but nonoptimal ambient temperatures account for far greater mortality burden.70
Although widespread attention is often paid to the mortality burden of extreme cold or hot temperatures, milder but nonoptimal ambient temperatures account for far greater mortality burden.
Exposure to nonoptimal temperatures has been linked to cardiovascular deaths.
In 2021, 1.17 million (95% CI: 1.07–1.29 million) cardiovascular deaths and 1.81 million (95% CI: 1.65–1.97 million) deaths overall were estimated as attributable to nonoptimal temperatures.
In 2021, 1.17 million cardiovascular deaths and 1.81 million deaths overall were estimated as attributable to nonoptimal temperatures.
In 2021, the all-cause DALYs due to nonoptimal temperatures were 420 per 100,000 (95% CI: 383–461 per 100,000).
Heat-related excess deaths are especially seen in Eastern Europe, while Sub-Saharan Africa had the highest estimates of cold-related excess deaths.71
Heat-related excess deaths are especially seen in Eastern Europe, while Sub-Saharan Africa had the highest estimates of cold-related excess deaths
Global preparedness initiatives are needed to buffer the cardiovascular effects of weather-related temperature extremes.
Global preparedness initiatives are needed to buffer the cardiovascular effects of weather-related temperature extremes.
Increased public health attention is needed on nonoptimal temperatures, especially on moderately hot and moderately cold temperatures, in addition to attention on the effects of extreme temperatures.
Additionally, continued research is warranted on the mechanisms underlying the regional variation, population susceptibility, and the effect of acclimatization to nonoptimal temperatures and CVD.72

11.Low physical activity
Low physical activity levels represent an important threat to cardiovascular health.
In 2021, 0.397 million (95% CI: 0.122–0.684 million) cardiovascular deaths and 0.686 million (95% CI: 0.269–1.09 million) deaths overall were estimated as being attributable to inadequate physical activity.
In 2021, 0.397 million cardiovascular deaths and 0.686 million deaths overall were estimated as being attributable to inadequate physical activity.
In 2021, the all-cause DALYs due to low physical activity were 193.0 per 100,000 (95% CI: 82.9–293.0 per 100,000).
The WHO Global Action Plan for Physical Activity put forth a comprehensive set of approaches, together with evaluative and monitoring frameworks to improve physical activity.
The WHO Global Action Plan for Physical Activity put forth a comprehensive set of approaches, together with evaluative and monitoring frameworks to improve physical activity.
Mobile health technologies have been effectively harnessed to promote physical activity and minimize sedentary time.
Mobile health technologies have been effectively harnessed to promote physical activity and minimize sedentary time.
In parallel to these individual changes, structural and environmental changes are needed to facilitate greater physical activity in the workplace and during leisure time.
In parallel to these individual changes, structural and environmental changes are needed to facilitate greater physical activity in the workplace and during leisure time.
Prior experiences in urban settings such as Bogotá, Colombia have shown that creating dedicated bicycle paths and temporarily closing streets to motorized vehicles help promote physical activity.73

12.High alcohol use
There is clear evidence of substantial years of life lost and reduction in life expectancy with heavy alcohol use, especially as alcohol consumption exceeds 100 g weekly.74
While data regarding the cardiovascular health effects of low-level or moderate alcohol consumption have been mixed, cardiovascular risks associated with increased blood pressure and arrhythmias are seen with higher alcohol use, and dangerous or binge alcohol use remains common.
While data regarding the cardiovascular health effects of low-level or moderate alcohol consumption have been mixed, cardiovascular risks associated with increased blood pressure and arrhythmias are seen with higher alcohol use, and dangerous or binge alcohol use remains common.
In 2021, 0.407 million (95% CI: 0.179–0.708 million) cardiovascular deaths and 1.88 million (95% CI: 1.49–2.39 million) deaths overall were due to high alcohol use.
In 2021, 0.407 million cardiovascular deaths and 1.88 million deaths overall were due to high alcohol use.
In 2021, the all-cause DALYs due to high alcohol use were 915 per 100,000 (95% CI: 767–1,130 per 100,000).
DALYs per 100,000 attributable to high alcohol use were highest in Eastern Europe and lowest in North Africa and the Middle East.
The underlying drivers of marked regional and national-level variability in high alcohol use remain incompletely understood.
In the United States, the National Institutes of Health has several research initiatives at the basic, clinical, and population-science levels to address the adverse impact of misuse of alcohol across the lifespan.75
Unfortunately, implementation of established interventions targeting excess alcohol intake has declined globally in recent years.76
Unfortunately, implementation of established interventions targeting excess alcohol intake has declined globally in recent years

Evolving research on COVID-19 and cardiovascular population health
The COVID-19 pandemic has had a profound impact on health worldwide.
Patients with CVDs faced among the highest risks of mortality and complications when infected by COVID-19.77
Patients with CVDs faced among the highest risks of mortality and complications when infected by COVID-19.77
COVID-19 may trigger acute cardiovascular events, such as myocardial infarctions or strokes,78 and the longer-term cardiovascular health implications of COVID-19 infection are increasingly recognized.79
Cardiovascular hospitalizations temporarily declined early during the COVID-19 pandemic in response to public lockdowns and physical distancing measures, raising concerns regarding missed acute cardiovascular pathologies,80 and chronic disease management and preventative care may have been delayed or deferred.81,82
Cardiovascular hospitalizations temporarily declined early during the COVID-19 pandemic in response to public lockdowns and physical distancing measures, …
… raising concerns regarding missed acute cardiovascular pathologies,80 and chronic disease management and preventative care may have been delayed or deferred.81,82
COVID-19 has magnified preexisting disparities in the delivery of healthcare for diverse populations.
Collectively, these direct and indirect health consequences of the COVID-19 pandemic may have led to increased population-level CVD burden in some locations.83,84
Collectively, these direct and indirect health consequences of the COVID-19 pandemic may have led to increased population-level CVD burden in some locations.83,84

Conclusions
The Global Burden of Cardiovascular Diseases Collaboration is an ongoing effort to increase the quality and availability of evidence for health decisions.
The accompanying almanac of data on regional and national CVD and risk-related burden may serve as a new resource for those developing effective strategies for disease prevention.
Updated estimates on CVD burden and risk factors can guide allocation and prioritization of resources for research, health care, and public health.
Funding Support and Author Disclosures
Funding for the Global Burden of Disease Study was provided by the Bill and Melinda Gates Foundation. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References & additional information
See the original publication (this is an excerpt version)
About the authors & affiliations
Muthiah Vaduganathan, MD, MPH, a
George A. Mensah, MD, b
Justine Varieur Turco, MA, c
Valentin Fuster, MD, PHD, d
Gregory A. Roth, MD, MPH
a Division of Cardiovascular Medicine, Brigham and Women’sHospital and Harvard Medical School, Boston, Massachusetts, USA;
b Center for Translation Research and Implementation Science, NationalHeart, Lung, and Blood Institute, National Institutes of Health, Bethesda,Maryland, USA;
c American College of Cardiology, Washington, DC, USA;
d Cardiovascular Institute, Icahn School of Medicine at Mount Sinai, NewYork, New York, USA; and the
e Division of Cardiology, Department ofMedicine, University of Washington, Seattle, Washington, USA.
Names mentioned
Gregory A. Roth, MD, MPH, senior author of the paper and associate professor in the Division of Cardiology and director of the Program in Cardiovascular Health Metrics at the Institute for Health Metrics and Evaluation at the University of Washington
Valentin Fuster, MD, PhD, an author of the paper, director of Mount Sinai Heart, physician-in-chief of The Mount Sinai Hospital and editor-in-chief of Journal to inform the global cardiovascular community JACC.
George A. Mensah, MD, an author of the paper and director of the Center for Translation Research and Implementation Science at the National Heart, Lung, and Blood Institute
With this awareness at the forefront, the
Global Burden of Cardiovascular Diseases Collaboration, an alliance between the
Institute for Health Metrics and Evaluation, the
National Heart, Lung, and Blood Institute, and the
Journal of the American College of Cardiology (JACC), was launched in 2020.
Bill and Melinda Gates Foundation.