Key messages (summarized by the Editor of the blog)
Building a national, regional and local integrated database platform that captures upstream policies, actions and behaviors — and links them to downstream health, economic and social hardship outcomes — will offer a more comprehensive view of the data necessary for decision-makers and citizens to more effectively monitor and mitigate harms caused by the pandemic.
It will also provide researchers a wider lens to observe and evaluate the impact of related natural experiments, policies and leadership efforts.
This will offer a more comprehensive view of the data necessary for decision-makers and citizens
to more effectively and intelligently monitor and mitigate harms caused by the pandemic.
International Journal for Quality in Health Care,
Volume 33, Issue Supplement_2, November 2021, Pages ii78–ii80,
Brant J Oliver, Peter Schmidt, Stephanie Tomlin, Sally A Kraft, Elliott Fisher, Eugene C Nelson
29 November 2021
Abstract
Introduction
The greatest challenge confronting political, public health, business, education and social welfare leaders in the COVID pandemic era is to restore the economy, businesses and schools without further risking public health.
The ‘COVID Compass’ project aims to provide helpful information to guide local decisions by tracking state and local policies over time and their impact on a balanced set of outcomes — health metrics, economic trends and social hardship indicators.
Methods
We selected a parsimonious set of ‘local level’ health, economic and hardship outcomes and linked them to ‘local level’ actions aimed to decrease COVID-19 health effects and to mitigate hardship for people, businesses and the economy.
Data trends will be released frequently (e.g. weekly and monthly) to show changes in health economic and social hardship ‘outcomes’ (based on quantitative data), alongside policy, health care, public health and individual/social ‘actions’ (based on both qualitative and quantitative data).
Results
Work on initial analytic and visualization prototypes of the COVID Compass is currently in progress at national, state and local levels.
Conclusion
Building a national, regional and local integrated database platform that captures upstream policies, actions and behaviors and links them to downstream health, economic and social hardship outcomes will ]
- offer a more comprehensive view of the data necessary for decision-makers and citizens
- to more effectively and intelligently monitor and mitigate harms caused by the pandemic.

Introduction
COVID-19 has wrought havoc worldwide. Many have died. Many more have lost their jobs, suffered financially or endured other hardships. Disparities due to race, ethnicity, income, immigrant status and other social risks have been exacerbated. Epidemiologists predict that COVID-19 will not disappear nor be eradicated by vaccines and will become endemic [ 1, 2].
Science, vested interests and hunches, not comprehensive data
The greatest challenge confronting political, public health, business, education and social welfare leaders is to restore the economy, businesses and schools without further risking public health.
Most are trying to minimize mortality, economic and social problems-based on a mix of public health advice and clinical science, vested interests, and hunches [ 2].
Useful, up-to-date information on COVID-19 case rates and case fatality rates are widely available via ‘trackers’ offered by many prestigious organizations [ 3–8].
However, these focus primarily on creating ‘leader boards’ showing
- COVID-19 case rates and fatality rates and
- do not include key trends in other vital outcomes related to economic vitality or social hardship
- nor do they track the ‘upstream’ policies, actions and behaviors that combine to produce key ‘downstream’ results on lives lost and on livelihoods damaged.
A ‘COVID Compass’ for intelligently navigating the pandemic
The ‘COVID Compass’ project aims to provide information to guide local decisions by tracking state and local policies over time and their impact on a balanced set of
- outcomes-health metrics (e.g. COVID-19 incidence and mortality),
- economic trends (e.g. unemployment rate) and
- social hardship indicators (e.g. food insecurity).
Conceptual framework
We start with a simple proposition-upstream actions taken in specific geographic contexts produce key downstream outcomes, both of which are influenced by local political and social contexts.
Figure 1 illustrates how ‘upstream’ decisions and actions interact to produce ‘downstream’ outcomes.
Our model emphasizes first-order relationships between actions and outcomes.
It attempts to recognize that interrelationships between these factors are complex and may behave in ways characterized by complex adaptive systems [ 9].
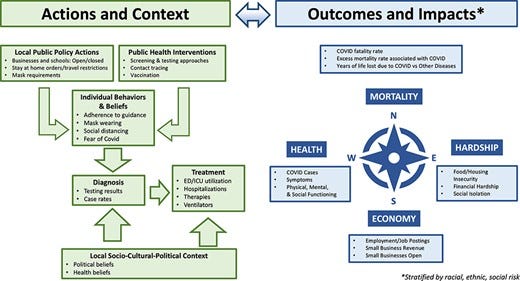
We assume that policy decisions, coupled with the specific actions and behaviors of individuals, families and health professionals (to prevent, detect, diagnose and care for people with COVID-19), will result in key outcomes. Using a balanced scorecard approach [ 10], we organized key outcomes into four major categories:
(i) mortality,
(ii) health,
(iii) economic and
(iv) hardship.
Analysis and sources
Analysis begins by focusing on a parsimonious set of local level health, economic and hardship outcomes and linking them to local-level actions aimed to decrease COVID-19 health effects and mitigate hardship to businesses and the economy.
Data trends will be released rapidly and frequently (e.g. weekly or monthly), including health, economic and social hardship outcomes (based on quantitative data) and actions (based on qualitative and quantitative data).
Our work uses US data from best available public sources such as The New York Times, Dartmouth Atlas, Johns Hopkins, National Bureau of Economic Research and U.S. Centers for Disease Control and Prevention (CDC).
The Opportunity Insights Economic Tracker published by Harvard University [ 11] provides economic data and COVID-related metrics at the zip code level to meet the immediate needs of federal, state, and local policymakers and other community leaders.
This could expand to provide a global view of the COVID Compass using tracker data from Oxford University, World Health Organization and the Gates Foundation.
Initial projects
We will initiate our analyses using data from the state of North Carolina, which is one of the most diverse and impoverished rural regions in the USA.
The Brody School of Medicine at East Carolina University has been tracking COVID-19 trends to inform policy and to support local decision-makers for the eastern region of North Carolina.
Leveraging the partnership between the Dartmouth Atlas, Dartmouth-Hitchcock, East Carolina University and others, we will build upon this work by developing a ‘case’ analysis that will focus on diverse small geographic areas or states that have taken different approaches to COVID-19.
Subsequent analyses may include similar rural regions, such as New Hampshire and Vermont, providing a foundation for evaluating disparities.
We plan to conduct studies of countries that have taken different approaches to addressing COVID-19.
Developing international opportunities includes
- a comparative study of a region of Sweden (Jonkoping)
- versus a region in Switzerland (Lausanne) and
- a partnership with BroadReach, Inc., a non-governmental organization with programs in low- and middle-income countries in Africa.
Conclusion
Building a national, regional and local integrated database platform that captures upstream policies, actions and behaviors and links them to downstream health, economic and social hardship outcomes will offer a more comprehensive view of the data necessary for decision-makers and citizens to more effectively monitor and mitigate harms caused by the pandemic.
It will also provide researchers a wider lens to observe and evaluate the impact of related natural experiments, policies and leadership efforts.
Acknowledgements
The authors wish to thank Professor Jon Skinner at the Dartmouth Institute for thoughtful reviews and advisement on this manuscript.
Funding
This work is supported by a grant provided by the State of North Carolina, USA.
About the authors
BRANT J. OLIVER1,2,3 , PETER SCHMIDT4 , STEPHANIE TOMLIN3 , SALLY A. KRAFT3,5 , ELLIOTT FISHER3 , and EUGENE C. NELSON3
1Departments of Community & Family Medicine and Psychiatry, Dartmouth-Hitchcock Health and Geisel School of Medicine at Dartmouth, Hanover, NH 03755, USA,
2Department of Veterans Affairs, White River Junction, VAQS and HPEER Advanced Fellowship Programs, Debakey VA Medical Center. 2002 Holcombe Blvd., Houston, TX 77030, USA,
3 The Dartmouth Institute for Health Policy & Clinical Practice, Geisel School of Medicine at Dartmouth, Hanover, NH 03755, USA,
4Brody School of Medicine, East Carolina University, 600 Moye Blvd, Greenville, NC 27834, USA, and
5 Center for Population Health, Dartmouth-Hitchcock Health, Lebanon, NH 03756, USA
References
See the original publication
Originally published at https://academic.oup.com./












