the health strategist
institute for continuous health transformation
& digital health
Joaquim Cardoso MSc
Chief Researcher, Editor and Senior Advisor
January 4, 2023
Executive Summary
- Paxlovid, an antiviral drug developed by Pfizer, was hailed as a “game-changer” for its ability to reduce the risk of severe COVID-19 by almost 90%.
- However, uptake of the drug has been slow, with only around 0.5% of new COVID-19 cases in the UK and 13% in the US receiving prescriptions for the drug, according to health analytics firm Airfinity.
- Concerns about “rebound” (the return of symptoms or detectable virus after a person begins to feel better) and side effects, …
- … as well as the high price of the drug and the need for it to be taken soon after infection, have contributed to the slow uptake.
- Some argue that symptom rebound tends to be very mild, and is still far preferable to hospitalization or death.
- In addition, declining concern about the risk of COVID-19 and inadequate funding for distribution have also played a role.
- Despite being one of the only tools available to prevent death in high-risk individuals, sentiment against Paxlovid has persisted.
- Paxlovid could soon have competition:
(1) in November, Japan authorized ensitrelvir, a once-daily antiviral …
(2) … In July, China authorized the use of an HIV drug to treat COVID-19, but detailed data from a large clinical trial have not been released.
DEEP DIVE
COVID drug Paxlovid was hailed as a game-changer. What happened?
Insufficient investment and fears about rebound and side effects are driving down use of a lifesaving antiviral.
Nature
Max Kozlov
January 3, 2023
When clinical trial data for the antiviral drug Paxlovid emerged in late 2021, physicians hailed its astonishing efficacy — a reduction of nearly 90% in the risk of severe COVID-19.
But more than a year later, COVID-19 remains a leading cause of death in many countries, and not only in low-income nations where the drug is in short supply. In the United States, for example, hundreds of people still die from COVID-19 each day.
Researchers say that the drug’s rollout has been hampered by worries about ‘rebound’ (the mysterious return of symptoms or detectable virus days after a person starts to feel better) and side effects — as well as by declining concern about the risk of COVID-19.
Inadequate funding for distribution, the drug’s high price tag and the need for it be taken soon after infection have also slowed its uptake.
As a result, physicians have prescribed the drug in only about 0.5% of new COVID-19 cases in the United Kingdom, and in about 13% in the United States, according to a report by the health-analytics firm Airfinity, based in London, UK. Even doctors have reported serious difficulties in helping their family members to obtain Paxlovid.
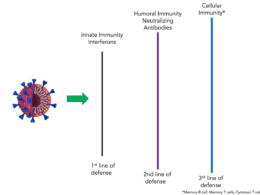
Sentiment against the drug has persisted even as regulators globally have rescinded authorizations for monoclonal antibodies against COVID-19, leaving Paxlovid as one of the only tools to prevent death in high-risk individuals, says Davey Smith, an infectious-disease physician at the University of California, San Diego.
“It’s a game-changer drug that has good efficacy, even in the setting of Omicron,” says Smith. “But rebound has been tagged as a reason not to take the drug, which is a shame.”
Premium protection
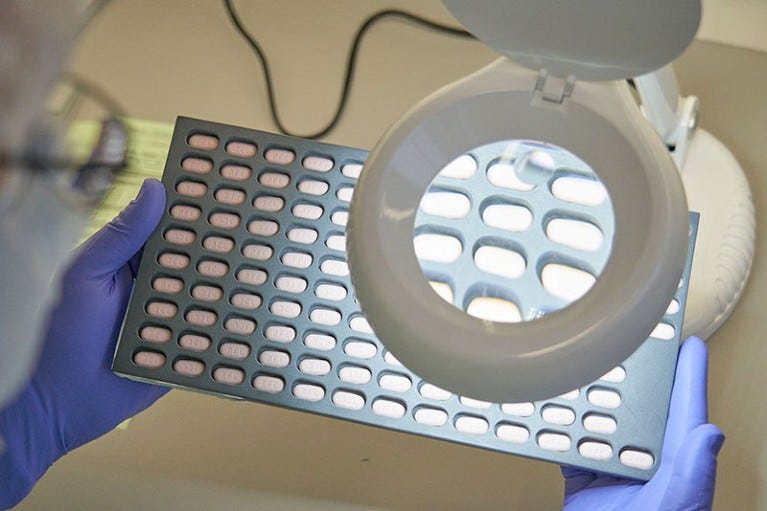
Paxlovid is a combination of the oral antiviral drugs nirmatrelvir and ritonavir.
It reduced the risk of hospitalization or death by 89% in high-risk individuals who took the drug within three days of experiencing symptoms, according to a clinical trial sponsored by pharmaceutical company Pfizer, which produces the drug and is based in New York City.
US regulators first authorized Paxlovid in December 2021, and have since loosened restrictions on who can prescribe it in an effort to make it more broadly available.
But health officials lament that the drug has not been deployed to the extent they had expected: about 10 million Paxlovid courses have been delivered to the United States, but only about 6.7 million have been used.
But health officials lament that the drug has not been deployed to the extent they had expected: about 10 million Paxlovid courses have been delivered to the United States, but only about 6.7 million have been used.
This underuse stems in part from misinformation and misconceptions about the drug, says Daniel Griffin, an infectious-disease physician at Columbia University in New York City.
For example, people perceive COVID-19 as less risky than they did earlier in the pandemic, Griffin says, making them less likely to seek treatment and physicians less likely to prescribe medications promptly.
Paxlovid works by inhibiting viral replication, which mostly occurs early in the disease course.
This means that the drug must be taken within the first five days of symptom onset, leaving a narrow window of time for people to receive treatment.
That does not mesh well with “this mentality of ‘Let’s wait and see how you do’,” among doctors treating people with COVID-19, says Griffin.
To add to the confusion, worries have swirled about post-Paxlovid ‘rebound’, fuelled by high-profile cases in figures such as US President Joe Biden and and former US infectious-disease chief Anthony Fauci.
Such publicity has had a chilling effect on the number of people seeking Paxlovid, says Smith.
But researchers have found that rebound often occurs even in people who don’t take Paxlovid.
Precise estimates for rebound incidence vary, depending on the population studied and the definition of ‘rebound’.
But regardless of whether people take Paxlovid, Smith says, it’s common for them to experience either viral rebound — in which people test positive again — or symptom rebound, but not both at the same time.
Smith says that symptom rebound tends to be very mild, and is still far preferable to hospitalization or death.
Smith says that symptom rebound tends to be very mild, and is still far preferable to hospitalization or death.
A bitter pill
In addition, Paxlovid can’t be taken with many other drugs and, in some people, makes certain foods taste bitter or metallic, both of which reinforce the perception that it’s toxic, Smith says.
Treatment requires taking several pills twice a day for five consecutive days — which isn’t the easiest regimen to adhere to, Smith adds.
In addition, Paxlovid can’t be taken with many other drugs and, in some people, makes certain foods taste bitter or metallic, both of which reinforce the perception that it’s toxic, Smith says.
Such concerns have led health officials to point to hesitancy to explain why use of the drug has fallen short.
But there are also systemic reasons, says Anne Sosin, a public-health-policy specialist at Dartmouth College in Hanover, New Hampshire.
Paxlovid relies on a robust COVID-19 testing infrastructure and access to primary-care physicians and pharmacies, she notes.
This amplifies pre-existing disparities resulting from race and income.
For example, Black and Hispanic populations were about 36% and 30% less likely to be prescribed Paxlovid, respectively, compared with white populations, according to an analysis of almost 700,000 people who sought COVID-19 care across 30 US sites.
Fears about hesitancy, says Sosin, provide an excuse to blame individuals rather than policymakers and to deflect “attention away from the system that needs to be in place to deliver the drugs”.

To remedy these disparities, she says she would like to see health officials mount an ‘all hands on deck’ approach to ensure that everybody has equal access to the drug by engaging local communities and expanding access to testing centres.
For example, health officials have successfully narrowed similar disparities in the number of people who received their primary COVID-19 vaccination series by bringing vaccines “to people in the areas they live, work and play”.
COVID-19 isn’t going away, says Smith, so it’s important to develop other antiviral drugs.
Paxlovid could soon have competition: in November, Japan authorized ensitrelvir, a once-daily antiviral made by the Japanese pharmaceutical company Shionogi, based in Osaka and Hokkaido University in Japan.
In July, China authorized the use of an HIV drug to treat COVID-19, but detailed data from a large clinical trial have not been released.
COVID-19 isn’t going away, says Smith, so it’s important to develop other antiviral drugs.
Paxlovid could soon have competition:
in November, Japan authorized ensitrelvir, a once-daily antiviral …
… In July, China authorized the use of an HIV drug to treat COVID-19, but detailed data from a large clinical trial have not been released.
Originally published at https://www.nature.com on January 3, 2023.
People mentioned
Davey Smith is an infectious-disease physician at the University of California, San Diego.
Daniel Griffin is an infectious-disease physician at Columbia University in New York City.
US infectious-disease chief Anthony Fauci
Anne Sosin, a public-health-policy specialist at Dartmouth College in Hanover, New Hampshire.
Japanese pharmaceutical company Shionogi,