At least 21 million people in the United States don’t have broadband access, which has constrained the use of telehealth.
NEJM
Jorge A. Rodriguez, M.D., Carmel Shachar, J.D., M.P.H., and David W. Bates, M.D.,
March 19, 2022
goodthinsfoundation
Executive Summary
by Joaquim Cardoso MSc.
Chief Editor of the “Modern Health Foundation Blog”
@Digital Health Institute
March 19, 2022
What is the size of the digital divide in the US?
- At least 21 million people in the United States don’t have broadband access, which has constrained the use of telehealth.
- People living in areas with low broadband access are less likely to make use of video visits than people in areas with more widespread access.
What is the importance of digital inclusion?
- As health care has shifted to increasingly rely on digital tools for patient care, digital inclusion has become critical to promoting health care equity.
- With digital health tools such as telehealth and patient portals becoming prominent components of care delivery, the barriers to digital inclusion have grown increasingly apparent.
What is changing in the US?
- The recently enacted Infrastructure Investment and Jobs Act (IIJA) makes investments that could foster sustainable digital inclusion.
- The law includes $65 billion for digital-inclusion initiatives. It earmarks $42.5 billion for investment in broadband infrastructure by means of state deployment grants, promotes broadband affordability.
- Although the law isn’t focused on health care, it addresses long-standing drivers of digital health disparities, presents new opportunities for community-based digital inclusion, and could be a critical lever for improving access to care.
- The IIJA takes much of the responsibility for building digital infrastructure away from individual health care organizations and makes digital inclusion a public concern.
What is the opportunity for Health Care?
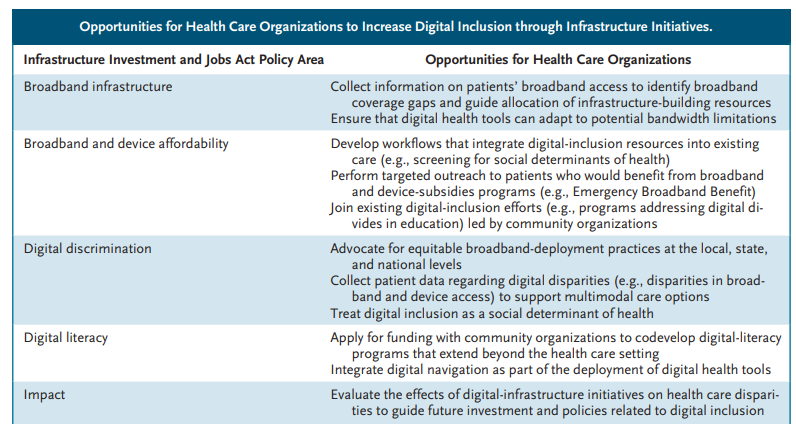
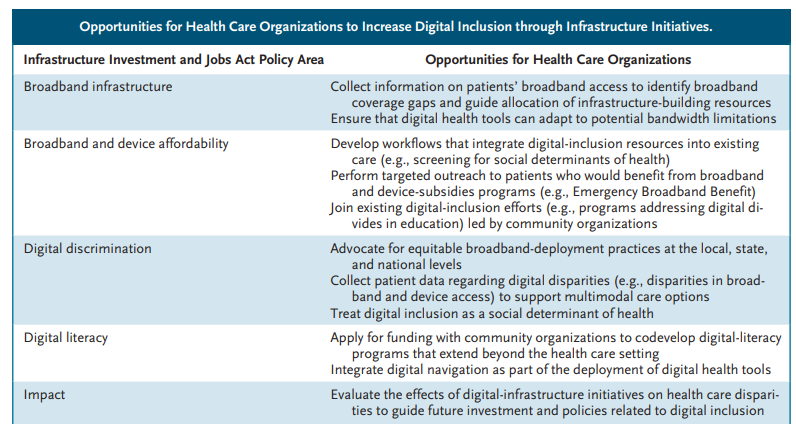
- We believe it’s important for health care organizations to understand the opportunities the law presents, to advocate for its effective and equitable implementation, and to take advantage of improvements to digital infrastructure (see table).
What are some barriers for digital Inclusion?
Structural barriers to digital inclusion, such as digital redlining, have limited the reach of digital health tools. (Digital redlining entails “discrimination by Internet service providers in the deployment, maintenance, or upgrade of infrastructure or delivery of services.”)
- Communities affected by digital redlining are generally the same ones that already have poor health outcomes.
- Health care systems have, by necessity, implemented digital tools in communities affected by digital redlining to reach underserved patients and combat health disparities.
Beyond digital redlining, other factors have made deploying digital health tools difficult, such as:
- limited broadband infrastructure,
- high prices for broadband service, and
- lack of access to Internet-enabled devices
The digital health expansion fueled by the Covid-19 pandemic has also made evident the importance of digital literacy for empowering patients to engage with this new care model.
What is the role of health care organizations in addressing the digital divide?
- In this new digital care environment, health care organizations are playing an important role in addressing digital divides. Several initiatives are being pursued.
- Although health care organizations have begun screening for digital needs, resources for addressing identified needs have been limited or underused. For example, the Covid-related Emergency Broadband Benefit, which provides subsidies for Internet and device purchases, hasn’t been widely adopted.4
- Moving forward, health care organizations, particularly those in underserved communities, could not only refer people to digital-inclusion programs, but also serve as active stakeholders in targeted outreach initiatives.
- By capitalizing on new policies, health care organizations could become a critical part of an environment of community-based players working toward digital inclusion.
- In this way, digital inclusion could be framed as a social determinant of health, and supporting digital inclusion could have positive effects on other social determinants, including education, employment, civic engagement, and housing.5
What is the final message?
Although passage of the IIJA represents an exciting step toward digital inclusion, we believe health care organizations must address additional barriers to create an inclusive system. Topics in this area include: adequate funding, adequate broadband speeds, necessary changes to the design of digital health platforms, assessment of the effects of digital tools to avoid exacerbating disparities, and provision of multimodal care options.
The future of digital health care relies not only on digital inclusion but also on the extension of policies enacted during the Covid-19 public health emergency that align with value-based care and equity.
- Patients will benefit from digital tools only if health care systems advocate for digital-inclusion policies.
As health care increasingly moves to a “digital first” approach, digital inclusion is becoming intertwined with health care equity.
- Health care organizations should therefore engage with digital-policy initiatives, including the IIJA, and providers should be prepared to capitalize on the opportunities afforded by such policies.
ORIGINAL PUBLICATION (full version)

Digital Inclusion as Health Care — Supporting Health Care Equity with Digital-Infrastructure Initiatives
NEJM
Jorge A. Rodriguez, M.D., Carmel Shachar, J.D., M.P.H., and David W. Bates, M.D.,
March 19, 2022
goodthinsfoundation
As health care has shifted to increasingly rely on digital tools for patient care, digital inclusion has become critical to promoting health care equity.
The recently enacted Infrastructure Investment and Jobs Act (IIJA) makes investments that could foster sustainable digital inclusion.
Although the law isn’t focused on health care, it addresses long-standing drivers of digital health disparities, presents new opportunities for community-based digital inclusion, and could be a critical lever for improving access to care.
The recently enacted Infrastructure Investment and Jobs Act (IIJA) makes investments that could foster sustainable digital inclusion.
Although the law isn’t focused on health care, it addresses long-standing drivers of digital health disparities, presents new opportunities for community-based digital inclusion, and could be a critical lever for improving access to care.
We believe it’s important for health care organizations to understand the opportunities the law presents, to advocate for its effective and equitable implementation, and to take advantage of improvements to digital infrastructure (see table).
With digital health tools such as telehealth and patient portals becoming prominent components of care delivery, the barriers to digital inclusion have grown increasingly apparent.1
For example, more than 100 studies have revealed disparities in portal use based on age, race, socioeconomic status, English-language proficiency, and other factors.2
Digital inclusion refers to “the activities necessary to ensure that all individuals and communities, including the most disadvantaged, have access to and use of [digital tools].”3
Structural barriers to digital inclusion, such as digital redlining, have limited the reach of digital health tools.
Digital redlining entails “discrimination by Internet service providers in the deployment, maintenance, or upgrade of infrastructure or delivery of services.”3
Communities affected by digital redlining are generally the same ones that already have poor health outcomes.
Health care systems have, by necessity, implemented digital tools in communities affected by digital redlining to reach underserved patients and combat health disparities.
With digital health tools such as telehealth and patient portals becoming prominent components of care delivery, the barriers to digital inclusion have grown increasingly apparent
Structural barriers to digital inclusion, such as digital redlining, have limited the reach of digital health tools.
Beyond digital redlining, limited broadband infrastructure, high prices for broadband service, and lack of access to Internet-enabled devices have made deploying digital health tools difficult.
At least 21 million people in the United States don’t have broadband access, which has constrained the use of telehealth. People living in areas with low broadband access are less likely to make use of video visits than people in areas with more widespread access.
Beyond digital redlining, limited broadband infrastructure, high prices for broadband service, and lack of access to Internet-enabled devices have made deploying digital health tools difficult.
At least 21 million people in the United States don’t have broadband access, which has constrained the use of telehealth
The digital health expansion fueled by the Covid-19 pandemic has also made evident the importance of digital literacy for empowering patients to engage with this new care model.
Delivering equitable care to underserved patients requires an inclusive system that ensures access to affordable broadband, Internet-enabled devices, digital-literacy supports, and appropriately designed platforms.
The digital health expansion fueled by the Covid-19 pandemic has also made evident the importance of digital literacy for empowering patients to engage with this new care model.
In this new digital care environment, health care organizations are playing an important role in addressing digital divides.
Organizations are developing dashboards to better measure digital disparities and guide systemwide solutions.
Some are attempting to narrow access and affordability gaps by purchasing and offering patients tools to support broadband access (e.g., Wi-Fi hotspots) and Internet-enabled devices.
The Federal Communications Commission (FCC) Covid-19 Telehealth Program provided financial support for devices and organizational telehealth infrastructure, though resources were limited.
Organizations have also reviewed their existing platforms and translated content into multiple languages.
Digital navigators, who had previously been deployed outside health care, emerged as new care team members to help patients use digital tools. Navigators can be costly and resource-intensive for health care organizations, however, which limits the sustainability of navigator programs.
In this new digital care environment, health care organizations are playing an important role in addressing digital divides.
The IIJA takes much of the responsibility for building digital infrastructure away from individual health care organizations and makes digital inclusion a public concern.
The law includes $65 billion for digital-inclusion initiatives.
It earmarks $42.5 billion for investment in broadband infrastructure by means of state deployment grants, promotes broadband affordability by providing
- $14.2 billion for $30-per-month subsidies for Internet costs for underserved people, and
- allocates $2.8 billion for the creation of digital-literacy programs.
- It also includes funds to support connectivity in tribal communities and broadband deployment in rural areas.
The IIJA takes much of the responsibility for building digital infrastructure away from individual health care organizations and makes digital inclusion a public concern.
The law includes $65 billion for digital-inclusion initiatives.
Although health care organizations have begun screening for digital needs, resources for addressing identified needs have been limited or underused.
For example, the Covid-related Emergency Broadband Benefit, which provides subsidies for Internet and device purchases, hasn’t been widely adopted.4
Moving forward, health care organizations, particularly those in underserved communities, could not only refer people to digital-inclusion programs, but also serve as active stakeholders in targeted outreach initiatives.
Although health care organizations have begun screening for digital needs, resources for addressing identified needs have been limited or underused.
Moving forward, health care organizations, particularly those in underserved communities, could not only refer people to digital-inclusion programs, but also serve as active stakeholders in targeted outreach initiatives.
In addition to providing funding, the IIJA could address health disparities stemming from digital exclusion.
The law charges the FCC with adopting rules to prevent “digital discrimination of access based on income level, race, ethnicity, color, religion, or national origin.”
These policies are an attempt to overcome structural barriers to digital inclusion, such as redlining.
Health care organizations will have to actively support antidiscrimination efforts to ensure that telecommunication companies are held to policies requiring equitable implementation.
Organizations could also partner with community groups and nonprofit organizations, such as the National Digital Inclusion Alliance, to advocate for equitable broadband deployment so that digital health tools could be harnessed to promote health care equity.
In addition to providing funding, the IIJA could address health disparities stemming from digital exclusion.
The IIJA also emphasizes a community-based approach to digital inclusion by establishing state-based grant mechanisms that encourage collaboration.
Digital health initiatives that are integrated into community-based programs can be more sustainable than piecemeal digital-literacy programs.
For example, health care organizations could work with groups offering classes for English-language learners or with libraries, which have long been essential to digital inclusion, to codevelop digital-literacy training programs for marginalized populations.
In addition, the IIJA supports connectivity for community anchor institutions (e.g., schools and libraries), which have become integral to equitable care delivery.
By capitalizing on new policies, health care organizations could become a critical part of an environment of community-based players working toward digital inclusion.
The IIJA also emphasizes a community-based approach to digital inclusion by establishing state-based grant mechanisms that encourage collaboration.
In this way, digital inclusion could be framed as a social determinant of health, and supporting digital inclusion could have positive effects on other social determinants, including education, employment, civic engagement, and housing.5
In this way, digital inclusion could be framed as a social determinant of health, and supporting digital inclusion could have positive effects on other social determinants, including education, employment, civic engagement, and housing.
Although passage of the IIJA represents an exciting step toward digital inclusion, we believe health care organizations must address additional barriers to create an inclusive system.
First, it’s unclear whether the new funding will be adequate to close access gaps, given the FCC’s unreliable broadband data. Organizations could collect information on which patients have broadband access to guide allocation of infrastructure-building resources.
Second, the IIJA considers adequate broadband speeds to be at least 100 megabits per second for downloads and 20 megabits per second for uploads. Digital health care implementation teams should be aware of bandwidth limitations, which could exclude patients with slower Internet speeds.
Third, the law doesn’t address changes that are needed to the design of digital health platforms (e.g., language translation) or to make workflows more inclusive (e.g., integration of interpreters into telehealth visits).
Fourth, it will be critical to evaluate the effects of digital tools to avoid exacerbating disparities.
Finally, organizations should continue to provide multimodal care options, since access to digital tools may vary, and such tools may not be appropriate for or preferred by all patients.
Although passage of the IIJA represents an exciting step toward digital inclusion, we believe health care organizations must address additional barriers to create an inclusive system.
The future of digital health care relies not only on digital inclusion but also on the extension of policies enacted during the Covid-19 public health emergency that align with value-based care and equity.
Harnessing community anchor sites will require the permanent removal of geographic restrictions and originating-site restrictions, which depend on a patient’s location during a telehealth visit.
Simplification of interstate licensing laws for clinicians would also enable digital tools to increase access to care for marginalized populations.
In addition, reimbursement parity among various forms of telehealth, including audio-only visits, would ensure that patients without full digital access could still benefit from remote care, including mental health services.
A combination of progressive digital-inclusion efforts and digital health policies could lay the foundation for technology-powered health care equity.
The future of digital health care relies not only on digital inclusion but also on the extension of policies enacted during the Covid-19 public health emergency that align with value-based care and equity.
A combination of progressive digital-inclusion efforts and digital health policies could lay the foundation for technology-powered health care equity.
Patients will benefit from digital tools only if health care systems advocate for digital-inclusion policies.
As health care increasingly moves to a “digital first” approach, digital inclusion is becoming intertwined with health care equity.
Health care organizations should therefore engage with digital-policy initiatives, including the IIJA, and providers should be prepared to capitalize on the opportunities afforded by such policies.
Patients will benefit from digital tools only if health care systems advocate for digital-inclusion policies.
As health care increasingly moves to a “digital first” approach, digital inclusion is becoming intertwined with health care equity.
Health care organizations should therefore engage with digital-policy initiatives, including the IIJA, and providers should be prepared to capitalize on the opportunities afforded by such policies.
This article was published on March 19, 2022, at NEJM.org.
Author Affiliations
From the Division of General Internal Medicine and Primary Care, Brigham and Women’s Hospital (J.A.R., D.W.B.),
Harvard Medical School (J.A.R., D.W.B.),
and the Department of Health Policy and Management, Harvard T.H. Chan School of Public Health (D.W.B.), Boston,
and the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics, Harvard Law School, Cambridge (C.S.) — all in Massachusetts.
References
See original publication.
Originally published at https://www.nejm.org.