JAMA Network
Jennifer Abbasi
January 18, 2022
The synthesis below was edited by the author of the blog:
SmartHealth Blog
Joaquim Cardoso MSc. (Chief Editor)
January 22, 2022
SYNTHESIS
Key points
- We’re moving from crisis to control, and that the national strategy needs to be updated accordingly.
- We clearly need a convenient, easy-to-access testing infrastructure that also links results to other important data
- Is a variant vaccine something that we could do quickly, especially during this phase of the pandemic where we’re still having such large numbers of cases? What about therapeutics?
Specific points
- Specific vaccines — It’s important to plan a parallel approach for variant-specific vaccines and for more broadly neutralizing, or universal, vaccines.
- Universal coronavirus vaccine — Is this something that you think is likely in the near future? Do you have an estimated time line on that? Dr Borio: I’ll say they should be as fast as possible but no faster than needed.
- At Home Testing — It’s remarkable that we have now a situation where people are able to do these sophisticated tests at home. I don’t see us going back. I think it’s going to open up a lot of novel ways to diagnose diseases at home.
- Oral antivirals , Testing Infrastructure & Management : Oral antivirals are starting to become available but the demand is super high, and supply and resources for administration are limited. These therapeutics are most effective early, so you need early testing and you need to connect people. How do we do a better job of linking the COVID-19 testing systems with an eye on equitable allocation of these limited resources?
- Testing infrastructure: We clearly need a convenient, easy-to-access testing infrastructure that also links results to other important data:
- Big data databases: The work of the government is to develop a system around this so that we can adequately capture the data. It may require some incentives to report the test.
- Data Services: Then somebody’s going to have to aggregate this data and create information from it. Because we all know that having a result is just the beginning and not the end.
- Telemedicine: … one of the things that I think is very, very important is how we think about telemedicine.
- Quality masks: In 2022, we have to be clear: N95, KN95, KF94 masks are the best masks, and they ought to supersede all others.
- Indoor Air Quality: A mitigation measure that we have not heavily discussed is indoor air quality. We don’t have an assurance that when we go into a building the air quality is of a very high standard. If we are going to really improve, for the long term, public health around a respiratory viral illness, upping the air quality indoors to MERV [Minimum Efficiency Reporting Value] 13 or better is going to be really important.
In the interim, people can use HEPA [high-efficiency particulate air] filters in school classrooms and other public places while we’re in the process of getting these better air filtration handling systems. - National electronic vaccine certification platform — There is some hope for a national electronic vaccine certification platform , that it’ll be widespread, even if it won’t be national.
- National and Regional Leadership —… it has to have national leadership but, as with politics, all health care is local in a sense, even though it may be paid for by the federal government.
Particular issues:
- Children under 5 & immunocompromising conditions — … We have about 25 million children under 5 years of age in this country and about 7 million people that are living with immunocompromising conditions.
- So even though we’d like to be able to move to the new normal as soon as possible, I think that one of the barriers to getting there is the fact that we have people that cannot access the vaccine yet and people that, despite being vaccinated, do not mount a protective immune response.
- Until we have ample supply of effective therapeutics and a way to link testing to diagnosis and therapeutics, that is going to slow us down.
Other impacts of Covid-19
- Deferred medical care — We have deferred medical care and many of our public health programs around the world, whether it be HIV, malaria, or polio eradication. The cost that’s occurred there has been substantial.
- Rebalance public health — We’re going to have to understand how to rebalance public health back to a time when many of these issues were not forgotten like they have been during COVID.
Conclusion
- I think the silver lining, if there is one to this pandemic, is that it gives us every reason to go back and reevaluate:
- Now is the time for renaissance thinking, as it relates to public health.
- Rebuilding public health is a key aspect of the strategy described in the Viewpoint.
I think that this is an exciting time coming up. It’s our opportunity.
ORIGINAL PUBLICATION
Long Version
Even as COVID-19 efforts focus on the current Omicron surge, most public health experts finally can foresee a near future when SARS-CoV-2 is endemic, not pandemic.
That vision for a new normal — the idea that, while transmission eventually will decline, COVID-19 is not going away — was woven through recent Viewpoints in JAMA coauthored by former members of the Biden-Harris COVID-19 Advisory Board.
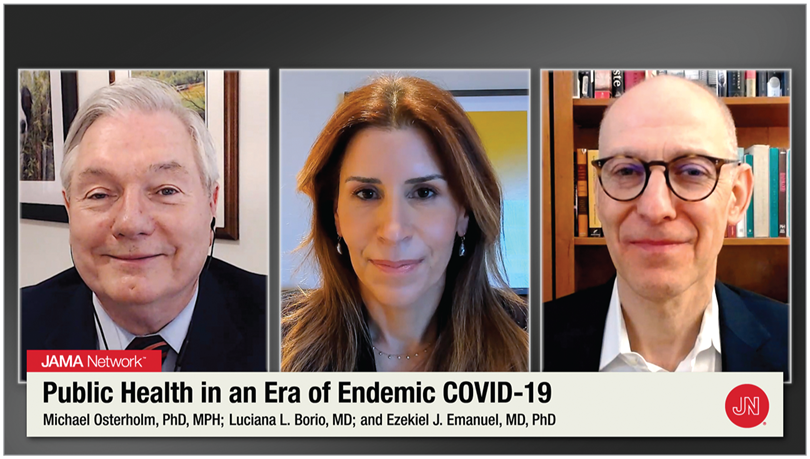
Luciana Borio, MD, senior fellow for global health at the Council on Foreign Relations; Ezekiel Emanuel, MD, PhD, vice provost for global initiatives at the University of Pennsylvania; and Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, were among the experts who served on the board from November 2020 to January 2021, helping to shape President Biden’s National Strategy for the COVID-19 Response and Pandemic Preparedness.
A year later, they say it’s time to update the plan.
The trio recently sat down for an interview with JAMA Associate Editor Preeti Malani, MD, MSJ, professor of medicine in the Division of Infectious Diseases at the University of Michigan Medical School and the university’s chief health officer.
The following is an edited version of their conversation, in which they shared ideas for living with a virus that’s not so novel anymore.
Dr Malani:The first Viewpoint outlines the idea that we’re moving from crisis to control, and that the national strategy needs to be updated accordingly.
You and your coauthors wrote that a new normal does not mean living without COVID-19. Tell me about the vision for this new normal.
… a new normal does not mean living without COVID-19.
Dr Emanuel: We’re not going back to 2019, when there was no COVID. COVID is going to be around us. It’s going to be one of the multitude of respiratory viral illnesses that we face and it’s going to wax and wane just like flu, just like RSV [respiratory syncytial virus], just like rhinovirus. We’re far from that situation at the moment, with about 1600 deaths a day, so getting there is going to require reducing transmission. That’s mainly going to be done through things like air quality improvements indoors, wearing masks, and some vaccination to get the incidence level low.
Then it’s making sure that people have fewer complications.
That’s partially achieved with the vaccines, which really are very, very good at reducing hospitalization and death, as well as the new therapeutics we have.
And then COVID should begin looking like a flu: you get it and you stay home so you don’t infect other people.
When you’re feeling better, you can go into work, probably wearing a mask for a few days to reduce the chance of infection. We’re simply going to get back to the life that we’ve known, with some modifications.
Dr Malani: Rebuilding public health is a key aspect of the strategy described in the Viewpoint. What can be done realistically to build the type of capacity you described?
Dr Osterholm: I think the silver lining, if there is one to this pandemic, is that it gives us every reason to go back and reevaluate: What are we doing with health care or disease care? What are we paying for? What are we not paying for that could make a difference from a public health standpoint? This is potentially either going to end up a forgotten moment we just want to move on from or it could be a renaissance moment in which we actually go back and ask ourselves these hard questions.
And now the lessons learned are right in front of us. They’re not imaginary. So I think this is a very critical time to look at how we improve the public’s health.
I’m an infectious disease epidemiologist, but I am very aware of all the adverse health outcomes that have occurred because we have deferred medical care and many of our public health programs around the world, whether it be HIV, malaria, or polio eradication.
The cost that’s occurred there has been substantial.
We’re going to have to understand how to rebalance public health back to a time when many of these issues were not forgotten like they have been during COVID.
Dr Malani: Could that happen nationally or is it going to be more of a local phenomenon?
Dr Osterholm: I think it has to have national leadership but, as with politics, all health care is local in a sense, even though it may be paid for by the federal government.
Look at what’s happening with our health care systems in terms of responding to all these cases of COVID. It turns out in the end, it’s local. What assets and resources do you have? Which people do you have that can come to work today or can’t come to work today? So I think it’s going to be a combination of both. It can’t be just top down.
iStock.com/WoodysPhotos
Dr Malani:Let’s move on to the second Viewpoint. We clearly need a convenient, easy-to-access testing infrastructure that also links results to other important data:
sociodemographics, vaccination status, and certainly clinical outcomes. But we’re a long way from this.
What do you think testing needs to look like for this new normal and how do you build a robust system to deal with the positive test results that arise?
Dr Borio: That’s the hard work. Sometimes we focus so much on developing the test, the vaccine, or the drugs, but linking the assets we have is the challenge.
It’s remarkable that we have now a situation where people are able to do these sophisticated tests at home. I don’t see us going back.
I think it’s going to open up a lot of novel ways to diagnose diseases at home.
The work of the government is to develop a system around this so that we can adequately capture the data.
It may require some incentives to report the test.
Then somebody’s going to have to aggregate this data and create information from it. In the near future, one of the great urgencies is to get the results of these tests and link them to an action — whether it’s isolation or access to treatment — as soon as possible.
Because we all know that having a result is just the beginning and not the end.
Dr Malani: Surveillance goes hand in hand with testing. What does a comprehensive surveillance program look like in 2022?
Dr Osterholm: We don’t have to capture every case in disease surveillance to understand what’s happening in our communities, both in terms of the actual number of cases or the impact that they’re having. But we’ve got to have a representative sample, hopefully of most cases, to really make that work.
Right now we have a system that is so broken.
It’s hard to believe, but there are health departments in this country that still receive their reports on disease cases by fax machine. I have no sense at all that the numbers we’re getting are reliable. I’ve been talking to state and local health departments around the country, and some are backed up thousands and thousands — even tens of thousands of cases — that have not yet been reported out over weeks and months, just because of the backlog.
One of the things we have to understand is that big data means something to public health in a way that most people don’t think of when they think of clinical medicine.
We’ve got to have a much better way to document who’s infected (when we do document it) and to aggregate that quickly just like the clinical information.
That has been a priority for public health for the last decade. And yet it has received little attention.
During this particular couple of weeks with Omicron, we’ve had to use alternative measures to understand what’s going on in our community: the number of hospitalizations, the number of people on oxygen in hospitals, and then, unfortunately, even deaths.
Now is the time for renaissance thinking, as it relates to public health.
What could we do if we had much more timely and more accurate information? This is going to be a combined effort of the federal, state, and local governments. And it’s got to involve the private sector in a big way, particularly our health care systems around the country, which is where most of these data come from.
Dr Malani: You write about encouraging the use of N95s or KN95s rather than cloth or surgical masks. But masks are also perhaps the most contentious aspect of mitigation, maybe even more than vaccines. How do you get people to actually do this, especially when they won’t wear a cloth mask?
Dr Emanuel: I think this is a case of social norming. What is expected in society and what are you doing as a responsible citizen? Unfortunately, this has become politicized. It’s been made a badge of culture, and that is the wrong way to look at it. It really is protective. It reduces transmission substantially. In 2022, we have to be clear: N95, KN95, KF94 masks are the best masks, and they ought to supersede all others.
How can we social norm that? One thing we suggested to the government is sending out a voucher so people could go to a pharmacy or grocery and get 3, 4, 5 of these masks free of charge.
That would certainly improve the public’s thinking around them. It would make them easily accessible, free, and I think much more used.
In 2022, we have to be clear: N95, KN95, KF94 masks are the best masks, and they ought to supersede all others.
A mitigation measure that we have not heavily discussed is indoor air quality. We don’t have an assurance that when we go into a building the air quality is of a very high standard. If we are going to really improve, for the long term, public health around a respiratory viral illness, upping the air quality indoors to MERV [Minimum Efficiency Reporting Value] 13 or better is going to be really important.
In the interim, people can use HEPA [high-efficiency particulate air] filters in school classrooms and other public places while we’re in the process of getting these better air filtration handling systems.
A mitigation measure that we have not heavily discussed is indoor air quality.
One other point, to go back to this issue of the health care system,…one of the things that I think is very, very important is how we think about telemedicine. We are going to have these crises, and workforce shortages, and overwhelming of systems in different places.
… one of the things that I think is very, very important is how we think about telemedicine.
A lot of medicine requires face-to-face contact, especially if you’re doing procedures. But there are a lot of things we can do via telemedicine that we have been resistant about adopting.
Primary care, a lot of mental health — we need to begin to make that standard and make permanent the changes we had around regulations for telemedicine during COVID. I think that will help us relieve some of the pressures when a system gets overtaxed.
Not just doctors, but nurses and a lot of others can provide services even while they’re being isolated.
Dr Malani: The third Viewpoint focuses on vaccines and therapeutics. Is a variant vaccine something that we could do quickly, especially during this phase of the pandemic where we’re still having such large numbers of cases?
Dr Borio: It’s important to plan a parallel approach for variant-specific vaccines and for more broadly neutralizing, or universal, vaccines.
One reason is because it’s possible that we’ll have another coronavirus surprise, and it would be really great to have vaccines that would work against several types of coronaviruses.
But it’s also because we can’t predict completely how this virus will evolve. There are trade-offs. At this moment, because there are uncertainties about how this is going to evolve, I think we need to go full steam ahead with this parallel effort.
It’s very important for government to help these companies establish a framework for how these decisions are going to be made.
Who makes the decision about what variants should be included in the vaccine mix? What are the correlates of protection that would allow us to do a rapid authorization for a strain change? That work is ongoing.
Dr Malani: You mentioned the universal coronavirus vaccine. Is this something that you think is likely in the near future? Do you have an estimated time line on that?
Dr Borio: I’ll say they should be as fast as possible but no faster than needed. You have to be very careful because vaccines are given to healthy people. Also, what does it mean to have a universal vaccine? We know that it’s not truly universal.
But I think the science is there for us to develop vaccines that are very good at inducing cell-mediated immunity and protecting us from the worst of this virus. I think the science is there also to select the epitopes very carefully that will maximize the desired impacts.
There’s always a silver lining, right? Vaccinology has dramatically progressed in the setting of COVID.
I can’t think of any other time recently that we had this type of scientific effort around vaccines, immunology, manufacturing, etc.
Dr Malani: Do you think we’ll move to a national electronic vaccine certification platform?
Do you think we’ll move to a national electronic vaccine certification platform?
Dr Emanuel: We’ve been resistant to it. I’m not sure I fully understand the resistance. There are platforms out there in a number of states. We have very, very good certification systems up and running. You’re not required to get an electronic certificate; you have to [opt] in and download the information.
It’s pretty secure because you have to use your phone and only you have your phone. So I think there is some hope that it’ll be widespread, even if it won’t be national.
Dr Borio: I’d like to add that we have about 25 million children under 5 years of age in this country and about 7 million people that are living with immunocompromising conditions. So even though we’d like to be able to move to the new normal as soon as possible, I think that one of the barriers to getting there is the fact that we have people that cannot access the vaccine yet and people that, despite being vaccinated, do not mount a protective immune response. Until we have ample supply of effective therapeutics and a way to link testing to diagnosis and therapeutics, that is going to slow us down.
I’d like to add that we have about 25 million children under 5 years of age in this country and about 7 million people that are living with immunocompromising conditions.
Dr Malani: Oral antivirals are starting to become available but the demand is super high, and supply and resources for administration are limited.
These therapeutics are most effective early, so you need early testing and you need to connect people. How do we do a better job of linking the COVID-19 testing systems with an eye on equitable allocation of these limited resources?
Oral antivirals are starting to become available but the demand is super high, and supply and resources for administration are limited.
These therapeutics are most effective early, so you need early testing and you need to connect people
Dr Borio: It will be very important as we move forward to make sure that access is facilitated.
If a person with a positive diagnostic test meets the [treatment] criteria, they should be able to self-refer to an infusion center and get assessed and treated right there without having to go through a physician.
Even when the monoclonals were in more ample supply, sometimes several days elapsed between a patient being diagnosed and then being referred to an infusion center.
Dr Emanuel: It’s not going to be stood up overnight, but we need a system where someone who tests positive — initially it’ll be PCR [polymerase chain reaction] testing but then hopefully we can get the at-home tests linked — gets a robocall that tells them how they can get the therapy or a number to call, as well as information on how they should isolate themselves, mask-wearing, and what they need to do to take care of themselves. That’s not impossible, right?
Dr Osterholm: If I could just add a piece of perspective.…we all remember, very painfully, those early days in the 1980s, when an HIV diagnosis was in essence a death sentence.
Today, we know that we can do amazing things with therapeutics.
On a global basis, we can do that with COVID if we put our minds to it, understanding just how different the world could be with a one-two punch of vaccines and therapeutics.
We could do a tremendous amount to reduce serious illness, hospitalizations, and deaths, and what more can we want?
I think that this is an exciting time coming up. It’s our opportunity.
If we miss it, people will die unnecessarily, and we will continue to deal with the social, economic, and political fallout of this disease. If we do it right, we can do so much to bring this horrible virus under better control.
I think that this is an exciting time coming up. It’s our opportunity.
Conflict of Interest Disclosures:
Dr Borio reported being a venture partner at Arch Venture Partners, receiving personal fees from Resilience Corp, and serving on the scientific advisory board for the Coalition for Epidemic Preparedness Innovations and on the board of directors for Eagle Pharmaceuticals and Insulet Corp. ]
Dr Emanuel reported personal fees, nonfinancial support, or both from companies, organizations, and professional health care meetings and being a venture partner at Oak HC/FT; a partner at Embedded Healthcare LLC, ReCovery Partners LLC, and COVID-19 Recovery Consulting; and an unpaid board member of Village MD and Oncology Analytics. Dr Emanuel owns no stock in pharmaceutical companies, medical device companies, or health insurers. No other disclosures were reported.
Names cited
Luciana Borio, MD, senior fellow for global health at the Council on Foreign Relations;
Ezekiel Emanuel, MD, PhD, vice provost for global initiatives at the University of Pennsylvania; and
Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota,
were among the experts who served on the board from November 2020 to January 2021, helping to shape President Biden’s National Strategy for the COVID-19 Response and Pandemic Preparedness.
Associate Editor Preeti Malani, MD, MSJ, professor of medicine in the Division of Infectious Diseases at the University of Michigan Medical School and the university’s chief health officer.
Originally published at https://jamanetwork.com
TAGS: At Home Testing; Early Warning System; Testing System;