institute for continuous
health transformation
Joaquim Cardoso MSc
Senior Advisor for Continuous Health Transformation
and Digital Health
January 9, 2023
Executive Summary
- The National Health Service (NHS) in Britain is facing a crisis in its general practice sector, with increasing numbers of patients unable to see their GP and record delays at accident and emergency departments.
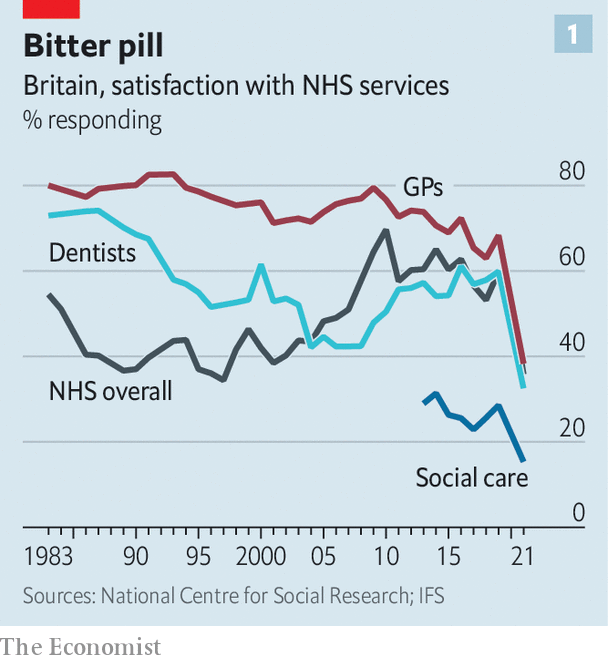
- The pressures on GP services are having knock-on effects on other parts of the NHS, with hospital waiting lists reaching 7.2 million, and patient satisfaction with GP services plummeting from 68% to 38% between 2019 and 2021.
- The GP sector is also facing a recruitment crisis, with many doctors opting to work overseas or in other parts of the NHS, and an increasing number of GPs retiring early.
- The problems in the GP sector are being exacerbated by the fact that it is underfunded and undervalued, with primary care services, which include general practice, accounting for 90% of clinical contact in the NHS but only receiving 10% of its budget.
- To try to alleviate the crisis, Britain is now training more new GPs than ever.
- But given difficulties retaining the doctors it already has, the government appears to have quietly dropped its manifesto pledge from 2019 of a net increase of 6,000 new family doctors by 2024.
The pressures on GP services are having knock-on effects on other parts of the NHS, with hospital waiting lists reaching 7.2 million, and patient satisfaction with GP services plummeting from 68% to 38% between 2019 and 2021.
What are the indicators of poor performance?
- High levels of patient dissatisfaction, as measured by surveys such as the British Social Attitudes Survey.
In 2021, satisfaction with GP services plummeted from 68% to 38%, according to the survey.
- Long waiting times for appointments with GPs, or high numbers of patients being unable to see a GP.
In October 2022, some 5 million people tried and failed to see their GP, according to one analysis.
- High levels of complaints from patients about their experiences with GP services.
In the year to April 2022, almost 100,000 written complaints were made about GPs, an increase of more than a third compared with the same period three years before.
- High levels of burnout and stress among GPs, which can lead to poor patient care and high levels of absenteeism.
- High levels of staff turnover, which can disrupt the delivery of care and reduce patient satisfaction.
- Poor patient outcomes, such as (1) high rates of hospitalization or (2) preventable deaths, which may be a result of inadequate care in the primary care setting.
DEEP DIVE

General practitioners are a big part of Britain’s health-care crisis
The Economist
MOUNTAIN ASH
Jan 9th 2023
Sajad ahmad seems to have a nice life. He makes good money working as a part-time general practitioner (GP), a family doctor, in the small town of Mountain Ash in southern Wales. From a fancy Scandinavian-style building, his consulting room looks out over fells of burnished copper crowned with firs.
But he cannot escape the immense strains currently affecting the National Health Service ( NHS).
One afternoon in December he had 42 appointments (the British Medical Association, the doctor’s union, advises a safe workload for GP s should not exceed 25 patients per day). “I had a horrible day,” recalls Dr Ahmad. “I broke down; I was probably horrible to the staff.”
General practice is one part of a health-care system in turmoil.
The most visible and alarming symptoms of crisis are overwhelmed accident-and-emergency ( A&E) departments in hospitals.
Record delays getting into A&E partly reflect pressures in the social-care sector, which mean that people who are fit to be discharged stay in hospital for longer than they should.
But they can also be traced to GPs, the gatekeepers to the NHS and conventionally the first port of call when a person feels sick.
The most visible and alarming symptoms of crisis are overwhelmed accident-and-emergency ( A&E) departments in hospitals.
But they can also be traced to GPs, the gatekeepers to the NHS and conventionally the first port of call when a person feels sick.
Primary-care services, which include general practice, pharmacy, dentistry and optometry, provide 90% of clinical contact in the NHS for less than a tenth of its budget. If things go wrong here, the knock-on effects are huge.
Primary-care services, which include general practice, pharmacy, dentistry and optometry, provide 90% of clinical contact in the NHS for less than a tenth of its budget. If things go wrong here, the knock-on effects are huge.
Things are going very wrong indeed.
In October 2022 some 5m people tried and failed to see their GP, according to one analysis.
That puts pressure on other services.
Some rebuffed patients call an ambulance; according to a recent poll, around one in five adults have gone to A&E because they cannot see their GP.
Those who stay at home may find that their condition becomes harder to treat; for a few, treatment comes too late.
Just as patients spill over from general practice into other services, problems in the rest of the NHS flow back to GP s.
Hospital waiting lists have ballooned from 4.2m to 7.2m since the pandemic began.
Unable to get their hip replacement, dermatology appointment or emergency treatment, many desperate patients are returning to their family doctor.
Hospital waiting lists have ballooned from 4.2m to 7.2m since the pandemic began.
Unable to get their hip replacement, dermatology appointment or emergency treatment, many desperate patients are returning to their family doctor.

The jams are fuelling growing frustration.
In the year to April 2022 almost 100,000 written complaints were made about GPs, an increase of more than a third compared with the same period three years before.
Satisfaction with GPs, as measured by the British Social Attitudes Survey, plummeted from 68% to 38% between 2019 and 2021, a more dramatic drop than for any other NHS service (see chart 1).
There are several sticks with which to beat GP s, from availability to pay to hours. Some of the criticism is warranted; much of it is unfair.
Satisfaction with GPs, as measured by the British Social Attitudes Survey, plummeted from 68% to 38% between 2019 and 2021, a more dramatic drop than for any other NHS service .
Many patients cannot forgive GPs for shutting their doors at the start of the covid-19 pandemic (albeit initially on the advice of the government).
After switching to telephone and virtual appointments, some doctors have been slow to resume face-to-face consultations, although seven in ten appointments are now in person.
But general practice stands out for providing more services than it did before the pandemic (see chart 2).

After switching to telephone and virtual appointments, some doctors have been slow to resume face-to-face consultations, although seven in ten appointments are now in person.
Some dissatisfaction with GPs reflects the fact that they are well-paid.
Unlike hospitals, general practices are small-to-medium-sized businesses, which are independently contracted by the NHS.
Most are owned by GP partners, who work together to secure premises, run their business and pay their staff, including salaried GPs.
The bulk of their income comes from delivering the essential services agreed in their contract.
For this, according to a special formula, they are paid a fixed sum for each patient on their registers. Other parts of the GP contract enable them to buttress their earnings.
Unlike hospitals, general practices are small-to-medium-sized businesses, which are independently contracted by the NHS. Most are owned by GP partners, who work together to secure premises, run their business and pay their staff, including salaried GPs.
The bulk of their income comes from delivering the essential services agreed in their contract.
For this, according to a special formula, they are paid a fixed sum for each patient on their registers. Other parts of the GP contract enable them to buttress their earnings.
Partnership can be a very lucrative arrangement.
In 2020–21, the salary of the average GP partner in England increased to £142,000 ($172,000).
But its allure seems to be fading.
Many GPs are choosing to become salaried, which means they earn less than half as much as partners but forgo the commitment of running a demanding business.
Some partners are handing back their contracts.
An investigation by Pulse, a website for GP s, found that in the nine years to August 2022, 474 surgeries across Britain had closed without being replaced.
Many GPs are choosing to become salaried, which means they earn less than half as much as partners but forgo the commitment of running a demanding business.
Some partners are handing back their contracts.

A shortage of doctors is by far the biggest challenge facing general practice.
Whereas there are 9% more consultants and 15% more junior doctors in hospitals than there were in 2019, there are 2% fewer full-time family doctors.
Whereas there are 9% more consultants and 15% more junior doctors in hospitals than there were in 2019, there are 2% fewer full-time family doctors.
Analysis by the Health Foundation, a think-tank, found that England was missing the equivalent of 4,200 full-time GP s in 2022, a number projected to double by 2030. Some are retiring early or moving abroad. The rest are steadily reducing their hours.
Analysis by the Health Foundation, a think-tank, found that England was missing the equivalent of 4,200 full-time GP s in 2022, a number projected to double by 2030.
Some are retiring early or moving abroad. The rest are steadily reducing their hours.
Covid-19 is not sufficient to explain this shortfall.
Recruitment and retention have been problems for the past decade, says Azeem Majeed, a professor at Imperial College London, and a part-time GP.
In fact, the profession was haemorrhaging doctors at a faster rate before the pandemic.
Recruitment and retention have been problems for the past decade, …In fact, the profession was haemorrhaging doctors at a faster rate before the pandemic.

A deeper crisis plagues the modern GP -for many, their job is less satisfying than it was before.
The births and deaths they once presided over are now largely the domain of specialists.
The sickness they deal with has become more complex and more chronic.
Fifty years ago “most people were dead at 70,” notes Beccy Baird of the King’s Fund, another think-tank.
Now there are around 15m Britons with long-term conditions, such as diabetes and dementia, who expect their illness to be managed.
Practices carry out double the number of consultations with frequent attenders (those who visit clinics more often than 90% of other patients) than they did 20 years ago.
Such patients, who are likely to be older and have multiple conditions, take up around four in ten of a clinic’s appointments.
The births and deaths they once presided over are now largely the domain of specialists.
The sickness they deal with has become more complex and more chronic
Bureaucracy has increased, although GPs often conveniently forget that this a commitment they once happily signed up for.
As part of the GP contract introduced in 2004, practices exchanged a much-maligned responsibility to provide round-the-clock care for a pay-for-performance scheme to supplement their main income.
The Quality and Outcomes Framework incentivises GP s to earn points, and thus more money, for chasing 72 targets.
Most of these are related to chronic-disease management: maintaining a list of patients with heart disease, for example, or tracking whether they are taking aspirin.
That deal, which within three years had earned GP partners a pay bump of 58%, now looks like a Faustian bargain.
As part of the GP contract introduced in 2004, practices exchanged a much-maligned responsibility to provide round-the-clock care for a pay-for-performance scheme to supplement their main income.
That deal, which within three years had earned GP partners a pay bump of 58%, now looks like a Faustian bargain.
Doctors have traded time with patients for paperwork.
Although only one in four GPs now works full-time, practitioners still clock in an average of 38.4 hours per week, according to the GP work-life survey by the National Institute for Health and Care Research.
That is more than the typical full-time employee in Britain.
Time spent box-ticking means that patients are less likely to receive continuity of care (ie, seeing the same doctor consistently) and more easily “reduced to a statistic”, sighs James Le Fanu, an ex- GP-turned-commentator.
“They go in to find someone staring at a computer screen who does not know them from Adam.”
GP partners also have a rising managerial burden.
In November 2022 over half of all appointments at surgeries were with non- GP staff such as nurses, pharmacists, physiotherapists and physician associates (who help diagnose patients, but do not prescribe).
In the long term this shift should make general practice more sustainable, but staff require training and supervision.
Clinics who try to cut costs by using physician associates risk a backlash from patients.
GPs who decide to call it quits are leaving the places that need them most.
Researchers at the University of Cambridge found that between 2015 and 2022 the number of GPs per 10,000 patients increased from 5.6 to 5.8 in the richest areas of England; over the same period this number fell from 5.6 to 5.3 in the poorest areas.
The most deprived quintile of areas in Wales, which includes Mountain Ash, also has the lowest number of GPs.
between 2015 and 2022 the number of GPs per 10,000 patients increased from 5.6 to 5.8 in the richest areas of England; over the same period this number fell from 5.6 to 5.3 in the poorest areas.
Part of the problem is that a practice’s core funding is weighted mostly for age, not for deprivation, even though the needs of the poorest are greater.
On the high street in Mountain Ash, houses with cracked plaster and blackened walls bear the signs of damp and mould, both of which are associated with many chronic illnesses.
A sweet shop with bright flashing lights guides children to its doors like an airport runway, a reminder that children in the poorest areas are nearly twice as likely to be obese.
Patients in these places are also less likely to join the record numbers of people going private in order to bypass NHS backlogs, or to have the education to manage their health well for themselves.
“We had a patient two to three months ago [who] went for a walk and part of her breast fell off,” says Dr Ahmad.
She had ignored the signs for so long that the tumour had burst through her skin, necrotising the surrounding tissue.
She was instantly placed under palliative care. In funding terms she would be worth as much to the surgery as someone who would pay for a private mammogram, says Dr Ahmad. “It doesn’t make sense.”

To try to alleviate the crisis, Britain is now training more new GPs than ever.
But given difficulties retaining the doctors it already has, the government appears to have quietly dropped its manifesto pledge from 2019 of a net increase of 6,000 new family doctors by 2024.
Kamila Hawthorne, a colleague of Dr Ahmad’s in Mountain Ash and the new chair of the Royal College of General Practitioners, the professional body representing GPs, is doing all she can to promote the good side of general practice.
Medical students need less convincing than those who have already qualified and are then training as family doctors.
The students arrive “all misty-eyed and altruistic”, she says. “The GP trainees see the workload.”
To try to alleviate the crisis, Britain is now training more new GPs than ever.
But given difficulties retaining the doctors it already has, the government appears to have quietly dropped its manifesto pledge from 2019 of a net increase of 6,000 new family doctors by 2024.
Originally published at https://www.economist.com on January 9, 2023.
People mentioned & Organizations
Sajad Ahmad — a general practitioner (GP) in the town of Mountain Ash in Wales
Azeem Majeed, a professor at Imperial College London, and a part-time GP.
Beccy Baird of the King’s Fund, another think-tank.
James Le Fanu, an ex- GP-turned-commentator.
Kamila Hawthorne, a colleague of Dr Ahmad’s in Mountain Ash and the new chair of the Royal College of General Practitioners