WHO
André Ilbawi, Cherian Varghese — Executive WHO editors and writers
February 2020
Key messages
- In 2018, there were an estimated 18 million new cases of cancer and 10 million deaths from cancer worldwide.
- The predicted global burden will double to about 29–37 million new cancer cases by 2040, with the greatest increases in LMIC.
- Cancer cases and deaths occur inequitably. Countries with lower incomes have significantly worse population outcomes, and, within countries, people at the lowest economic levels have poorer cancer outcomes and are more likely to suffer financial hardship.
- Of the 15 million deaths between the ages of 30 and 69 (“premature deaths”) in 2018, 4.5 million were due to cancer. In 80% of countries, trends in premature mortality from cancer are inhibiting progress toward achieving SDG target 3.4.
- Scaling-up cancer control to achieve UHC is essential to improve outcomes and save lives in all countries.
Table of Contents (TOC)
1.1 Understanding the global burden of cancer
1.2 Social and economic inequalities in cancer
1.1 Understanding the global burden of cancer
NCDs are by far the leading cause of death globally, responsible for 71% of all deaths in 2016[1] (1), and, of the 15.2 million premature deaths, 4.5 million (29.7%) were due to cancer. Cancer is the first or second leading cause of premature death in 134 of 183 countries in the world[2] (2).
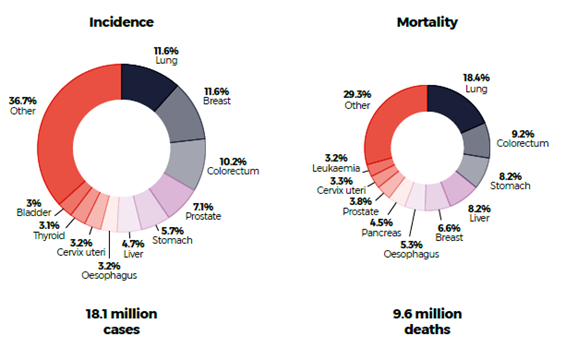
In 2018, there were an estimated 18.1 million new cases and 9.6 million deaths from cancer (Fig. 1.1).
Cancer is already responsible for one in six deaths globally. The numbers of new cases and deaths continue to rise because of increasing life expectancy and epidemiological and demographic transitions[3] (3). SDG 3.4 calls for a one-third reduction in premature mortality from NCDs by 2030. Unfortunately, progress in cancer has been slower than general progress in NCDs[4] (4).
Cancer will develop in one in five people before they reach the age of 75.
Fig. 1.1. Estimated global burden of cancer in 2018
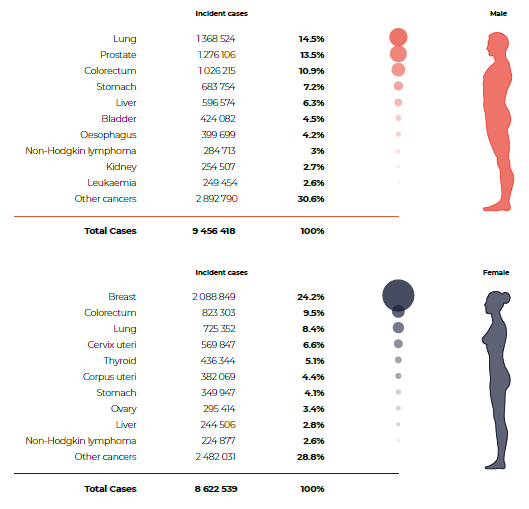
Source: reference 2
1.1.1 Scale and profile of cancer
In 2018, the most frequently diagnosed cancer was of the lung (11.6% of all cases), followed by female breast (11.6%) and colorectal cancer (10.2%). Lung cancer is also the leading cause of death from cancer (18.4% of all deaths), followed by colorectal (9.2%) and stomach cancers (8.2%). The 10 most common cancers are responsible for 60–70% of cancer incidence and mortality (Fig. 1.2).
Fig. 1.2. Distribution of cases and deaths by the leading 10 cancer types in 2018 for both sexes.
Substantial global heterogeneity in the leading cancer types is due to differences in exposure to risk factors and in life expectancy (Fig. 1.3)[7] (5). The age-standardized rates for the majority of cancer types are higher in countries with a higher HDI[8] (6), although some cancers, such as Kaposi sarcoma, cervical cancer and nasopharyngeal cancer, are more frequent in countries with low HDI (Figs 1.4 and 1.5; Annex 2)[9] (3). Differences among countries in the occurrence of most common cancers indicate that the national response must be contextualized to the epidemiological burden.
Fig. 1.3. Age-standardized rates for cancer incidence and mortality according to human development index in 2018.
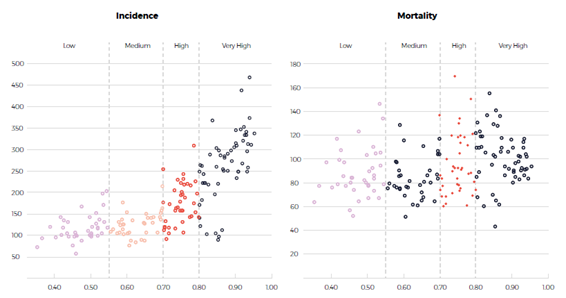
Source: references 3,6[10] [11].
Fig. 1.4. Age-standardized rates of prostate cancer and of cervical cancer in countries according to human development index in 2018.
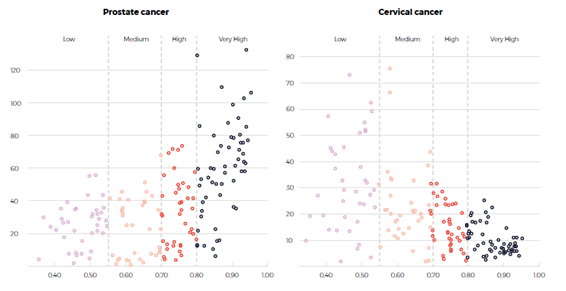
Source: references 3,6[12] [13].
Fig. 1.5. Differences in relative risks of cancers according to human development index.
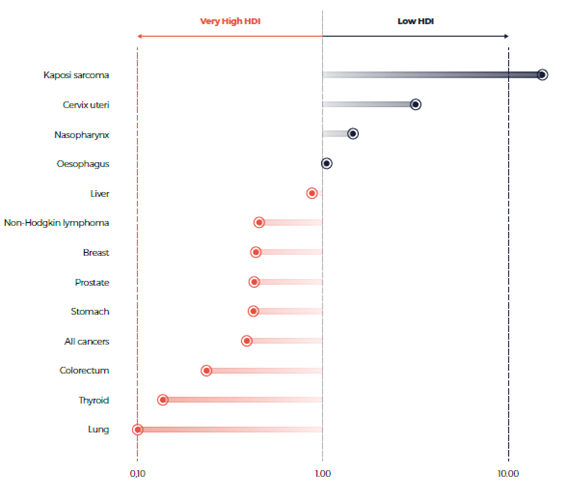
Source: reference 5[14].
Ideally, long-term predictions also account for recent trends in national cancer- and sex-specific rates based on projections of age, period and birth cohort[15] (7). Yet, for much of the world, there is too little information on cancer incidence and mortality. Exercises in which recent trends in the rates of major cancers in countries by HDI were derived from high-quality cancer registry data indicated that increased life expectancy and the ageing of the population contribute three fifths and the increased age-standardized rates contribute two fifths of future trends[16] (8). If these assumptions hold, the predicted global incidence will double to about 37 million new cancer cases by 2040 (Fig. 1.6).
Fig. 1.6. Estimated global burden of cancer in 2018 and that in 2040 according to United Nations population projections.
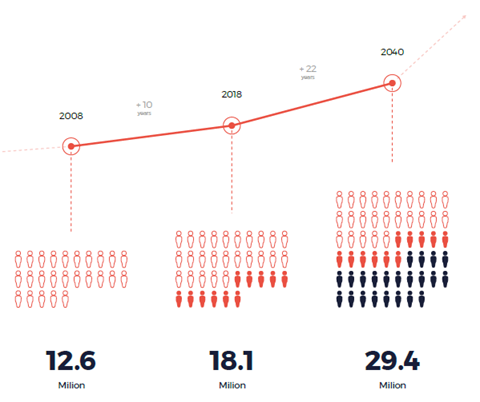
Source: reference 3[17]
In absolute terms, the burden is highest in countries with high and very high HDIs, although, in relative terms, the increases will be proportionally greater in countries with low and medium HDIs[18] (2). The anticipated surge in the annual number of new cancer patients over the coming decades, particularly in countries with low or medium HDI (see Fig. 1.7), is a clear signal for immediate, sound investment in cancer control.
Fig. 1.7. Trends in annual numbers of breast cancer cases in Ethiopia and Germany, 2010–2110.
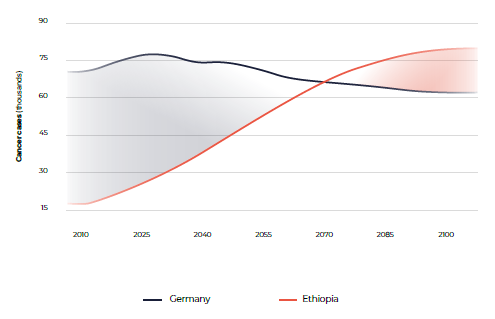
Source: reference 1,7[19] [20]
The full cancer burden, including those in children and rare cancers, should be considered. Cancer in children is commonly under-recognized, which has resulted in significant global inequality. Cancer occurs in more than 300 000 children every year worldwide, and the rate is expected to increase with control of competing causes of mortality, such as communicable diseases. Studies of the burden of childhood cancer have shown wide inequality among countries, as children in countries with low and medium HDIs are significantly less likely to access care or receive successful treatment[21] (10).
1.1.2 Recent trends and future cancer burden
An epidemiological transition has occurred over the past 60 years, as deaths from infectious disease have decreased and the burden of NCDs, including cancer, has increased.
Improvements in sanitation, the discovery of antibiotics and vaccine development have contributed to this epidemiological shift.
Changes in the prevalence and the distribution of risk factors strongly affect trends in cancer types, with implications for cancer control strategies.
For example, the different impact of the smoking epidemic on lung cancer incidence in countries with high and lower HDIs is correlated with the prevalence of tobacco use.
Countries with very high HDIs were the first to adopt and subsequently relinquish tobacco habits; thus, a steady rise, peak and decrease in smoking prevalence among men were followed 20–30 years later by a similar pattern in lung cancer rates[22] (11).
Similarly, the incidence of infection-related cancers, such as of the cervix, liver and stomach, has decreased significantly over the past three decades in countries with very high HDIs, but they remain common in those with low and medium HDIs.
Trends in mortality rates are also a function of changes in incidence and survival, which are related to health system capacity for cancer management, including earlier diagnosis and access to effective treatment.
Studies on the probability of surviving cancer have two clear findings:
(i) survival can be improved by investing in cancer management, and
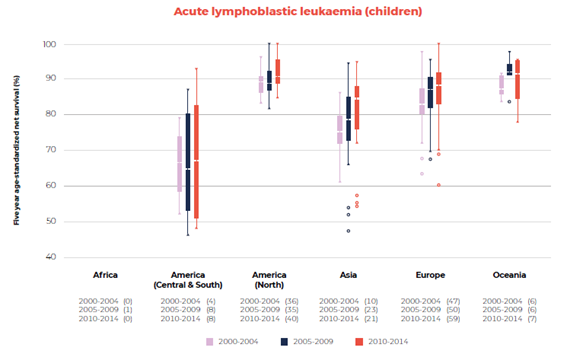
(ii) trends in survival differ by country and region (Fig. 1.8; 12[23]).
Fig. 1.8. Box plot (minimum, first quartile, median, third quartile, and maximum) for survival from breast and acute lymphoblastic leukaemia (children) by continent
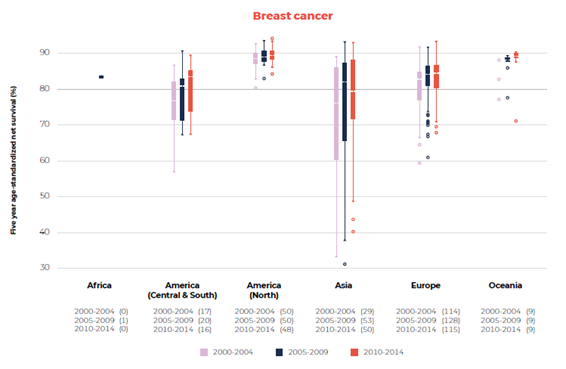
Source: reference 12[24].
1.2 Social and economic inequalities in cancer
Cancer cases and deaths occur unequally. Social and economic inequalities such as differences in income, education, housing, employment, diet, culture, gender, ethnic group and environment can affect the cancer burden, and socially and economically disadvantaged populations have poorer outcomes, as they are more likely to have preventable cancers that are diagnosed at a later stage, with a poorer prognosis, and they are more likely to have inadequate access to treatment.
In order to reduce inequality, cancer control should include targeted activities to decrease the exposure of such populations to avoidable risk factors.
In absolute terms, the burden of cancer is highest in countries with high and very high HDIs, but, in relative terms, the increases will be proportionally greater in countries with low and medium HDIs
By 2040, 67% of annual cancer cases will be in LMIC[25] (3).
1.2.1 Socioeconomic determinants of cancers
Determinants of health and cancer incidence: Determinants of health, such as biological factors, physical and social environments and economic status, influence cancer incidence and outcomes.
Tobacco use, for example, is more prevalent in lower socioeconomic groups in countries with higher HDIs, resulting in 60–90% higher rates of tobacco-related cancers[26] (13).
The differential distribution of cancer rates by socioeconomic status is partly explained by differences in tobacco use, alcohol consumption, unhealthy nutrition, obesity and lack of physical activity[27] (14).
Environmental factors also contribute to socioeconomic inequality in cancer (Fig. 1.9). The prevalence of a number of common cancers related to infection, including cancers of the stomach (Helicobacter pylori), cervix (HPV) and liver (hepatitis B and C viruses), is higher in the most disadvantaged groups[28] (13), both nationally and sub-nationally, with larger overall proportions of infection-associated cancers in lower-income countries and lower socioeconomic groups[29] (14).
Unequal access to policies and programmes for cancer prevention increases inequality over time.
For example, in 2014, 34% of young women in HIC and only 3% of those in LMIC received a full course of HPV vaccine[30] (15). There has been recent progress.
While access to HPV vaccine was previously mainly restricted to girls in HIV, by 2020, most HPV vaccine doses are to be given to girls in LMIC.
Fig. 1.9. Proportions of cancer cases attributable to infectious agents, 2018.
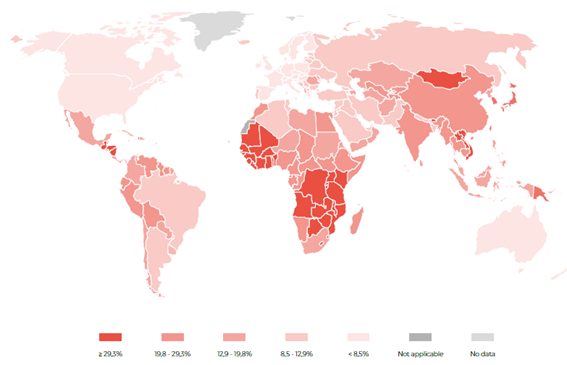
Source: reference 14[31]
People living with HIV are also at higher risk of several cancers, particularly those that are AIDS-defining (Kaposi sarcoma, non-Hodgkin lymphomas and invasive cervical cancer) and those associated with infectious agents (anal cancer caused by HPV, Hodgkin lymphoma linked to Epstein-Barr viruses and liver cancer related to hepatitis B and C viruses).
Public health interventions for the control of HIV have already mitigated the growing cancer burden[32] (16).
With even better treatment and a projected increase in the life expectancy of people living with HIV/AIDS, further investment in clinical trials will be required to identify the most effective cancer prevention and control strategies.
Determinants of health and cancer mortality: Mortality from cancer is strongly correlated to the stage of cancer at diagnosis and the quality of treatment. Disadvantaged groups often delay presentation, experience geographical and economic barriers to care and participate less in screening programmes, resulting in more late diagnoses and marked differences in outcomes[33] [34] [35](17–19).
Even when cancers are diagnosed at an early stage, disadvantaged groups are generally more likely to receive lower-quality care, fail to complete treatment or, for cancers with a poor prognosis, be transitioned to non-curative care[36] [37] [38] (20–22).
In countries with universal access to education and health care, outcomes may still be unequal[39] (23).
Concerted, broad population-based approaches are required, such as increasing education, health literacy and access to clinical services for disadvantaged populations.
1.2.2 Social and economic consequences of cancer
Nearly everyone has been affected by a cancer diagnosis in themselves, their family or their friends.
Cancer thus directly affects not only patients but also their families, friends and communities.
People with cancer experience high rates of financial hardship and in many cases, catastrophe, which is increasing over time as cancer care becomes more expensive[40] (24).
In South-East Asia, for example, the rate of financial catastrophe is 70% or higher[41] [42] [43] (24–26) (see also section 2.4.1).
Severe financial distress after a cancer diagnosis may increase the likelihood of death, even after apparently effective treatment[44] (27).
Psychological and financial distress extend to families and caretakers, particularly when there is limited or no access to care or when it is prohibitively expensive.
Family members and caretakers often provide unpaid care that can result in loss of employment, financial hardship and poor physical and mental health[45] (28).
The children of a parent with cancer also have worse health outcomes[46] (29).
The burden of cancer affects a country’s economy because of absence from work, lost productivity and premature mortality.
An assessment of the productivity lost due to premature death from cancer in Brazil, China, India, the Russian Federation and South Africa in 2012 indicated a loss of US$ 46.3 billion, corresponding to 0.2–0.5% of total gross domestic product (GDP) in those countries[47] (30).
In 2009, the total cost of premature mortality related to cancer in Europe was estimated to be €945.7 million[48] (31).
Countries with UHC can protect people against such negative economic and social consequences and improve their outcomes[49] (23).
1.2.3 Achieving cancer-related Sustainable Development Goals
Reducing the burden of cancer is a vital component of meeting commitments to reduce premature death and disability from NCDs, particularly SDG target 3.4. In 2015, the probability of premature death from NCDs was 7.5% in LMIC and 6.8% in HIC[50] (1).
Only 12 countries globally are on track to achieve a one-third reduction in premature mortality from cancer by 2030. Reaching SDG target 3.4 will require greater investment in cancer and other NCDs.
While substantial progress has been made in HIC because of favourable trends in cancer incidence and mortality attributed directly to advances in cancer control, progress in LMIC has been slow and insufficient[51] [52](32, 33) (Fig. 1.10) and must be accelerated.
Fig. 1.10. Progress towards SDG target 3.4. Change between 2000 and 2015 in probability of dying from cancer during ages 30–69 years of age and trend toward 2030, by region and World Bank income level.
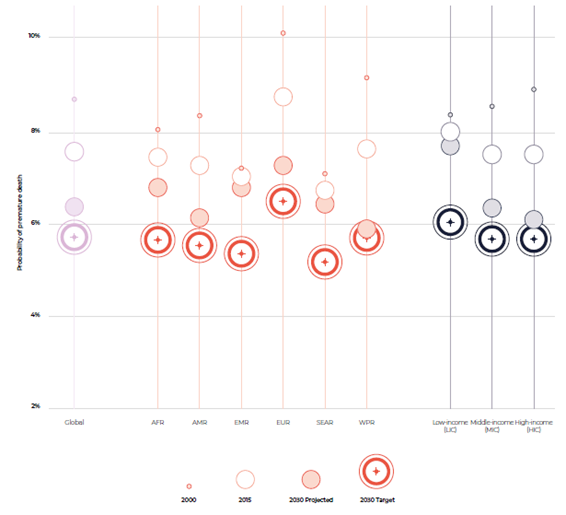
Source: reference 1[53]
… substantial progress has been made in HIC because of favourable trends in cancer incidence and mortality attributed directly to advances in cancer control,
… progress in LMIC has been slow and insufficient and must be accelerated.
References
See the original publication
Suggested citation
WHO report on cancer: setting priorities, investing wisely and providing care for all. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Originally published at https://www.who.int