Health, Care and Tech Transformation (HCTT)
research institute, knowledge portal and
advisory consulting
Joaquim Cardoso MSc*
Founder and Chief Researcher, Editor and Advisory
November 5, 2022
MSc* from London Business School
MIT Sloan Masters Program
Overview
- The 2022 edition of Health at a Glance: Europe examines the key challenges European countries must address to develop stronger, more resilient health systems following the acute phase of the COVID-19 pandemic.
- It includes a special focus on how the pandemic has affected young people’s mental and physical health.
- The report emphasises the need for additional measures to prevent the COVID-19 pandemic from scarring a generation of young people.
- This edition of Health at a Glance: Europe also assesses the pandemic’s disruption of a wide range of health services for non-COVID patients, as well as the policy responses European countries deployed to minimise the adverse consequences of these disruptions.
- It also addresses a number of important behavioural and environmental risk factors that have a major impact on people’s health and mortality, highlighting the need to put a greater focus on the prevention of both communicable and non-communicable diseases.
The 5 key recommendations of the report are the following:
- 1.Strengthening health system resilience
- 2.Promoting better prevention and management of non-communicable diseases
- 3.Improving mental health
- 4.Supporting the digital transformation of health systems
- 5.Strengthening national, European and global efforts to prepare for future health threats
ORIGINAL PUBLICATION (oecd)
Health at a Glance: Europe 2022 — State of Health in the EU Cycle [executive summary]
OECD
December 2022
EXECUTIVE SUMMARY
Introduction
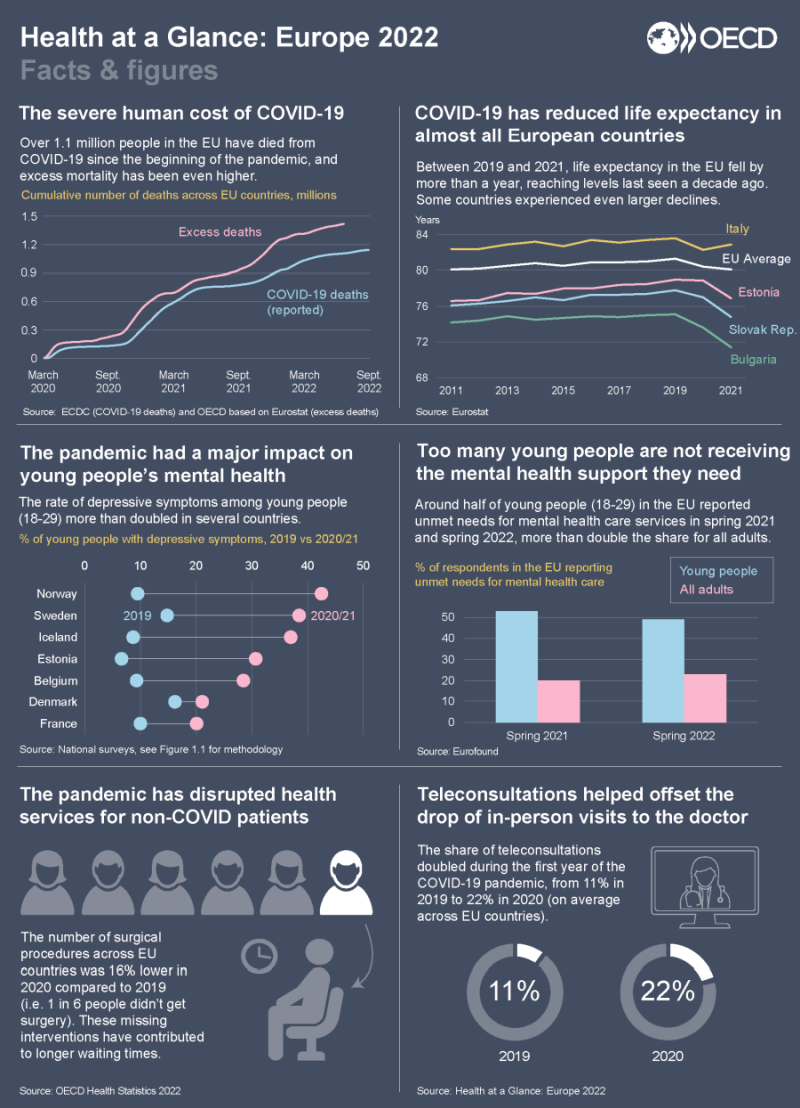
The pandemic has had a dramatic impact on people’s lives in Europe and around the world.
It has led to a reduction of more than one year in life expectancy in the EU in 2021 compared with the pre-pandemic level — the largest drop observed in most EU countries since World War II.
By the end of October 2022, more than 1.1 million COVID-19 deaths had been reported across the 27 EU countries.
This is however an under-estimation, with excess mortality statistics pointing to an additional 300 000 people dying as a direct or indirect result of the pandemic.
Over 90% of COVID19 deaths have occurred among people over the age of 60.
By the end of October 2022, more than 1.1 million COVID-19 deaths had been reported across the 27 EU countries. This is however an under-estimation, with excess mortality statistics pointing to an additional 300 000 people dying as a direct or indirect result of the pandemic.
Over 90% of COVID19 deaths have occurred among people over the age of 60.
The mortality impact of COVID-19 has been
- lowest in the Nordic countries (Iceland, Norway, Denmark and Finland), and
- highest in Central and Eastern European countries (Bulgaria, Hungary, Croatia, Czech Republic, Slovenia, Latvia and Romania).
Many factors explain cross-country differences in COVID-19 mortality, …
… including the pre-existing health conditions and vulnerabilities of the population before COVID-19, the timing and effectiveness of containment strategies, the take-up of COVID-19 vaccination, and differences in the capacity of health systems to respond effectively to the unprecedented challenges imposed by COVID-19.

The pandemic has had a major impact on the mental and physical health of young people
Although the pandemic has had an impact on nearly everyone’s life, there have been particular concerns about the mental and physical health of the millions of young Europeans whose formative years have been marked by disruptions in their education and social activities.
In several European countries such as Belgium, Estonia, France, Sweden and Norway, the share of young people reporting symptoms of depression more than doubled during the pandemic, reaching prevalence levels at least twice as high as in older age groups.
Many children and young people also spent considerably less time engaging in physical activity and had worsening nutrition habits, with indications of a rise in child overweight and obesity in some countries.
In several European countries such as Belgium, Estonia, France, Sweden and Norway, the share of young people reporting symptoms of depression more than doubled during the pandemic, …
Many children and young people also spent considerably less time engaging in physical activity and had worsening nutrition habits, …
The growing demand for mental health support, combined with disruptions in care delivery during the pandemic, challenged already-stretched mental health services.
About 50% of young Europeans reported unmet needs for mental health care in spring 2021 and again in spring 2022.
Many countries have implemented some measures to protect and care for young people’s mental health, yet the magnitude of the impact warrants further action to ensure the pandemic does not leave permanent scars on this generation.
About 50% of young Europeans reported unmet needs for mental health care in spring 2021 and again in spring 2022.

Care disruption during the pandemic created a backlog of patients for cancer care and elective surgery
The pandemic also disrupted the provision of primary care, cancer screening and treatment, care continuity for people with chronic conditions, and elective (non-urgent) surgery, especially during times when confinement measures were in place.
During the first months of the pandemic in spring 2020, disruptions in cancer screening programmes and specialist consultations resulted in cancer patients being diagnosed at a later stage.
Many countries were able to offset some of the initial reductions in cancer screening by scaling up activities in the second half of the year.
However, screening rates for breast and cervical cancer still fell by 6 % on average in EU countries in 2020.
Delays in cancer screening can lead to many cancer patients being diagnosed at more advanced stages, making their treatment more complex and reducing their chances of survival.
Many countries were able to offset some of the initial reductions in cancer screening by scaling up activities in the second half of the year.
However, screening rates for breast and cervical cancer still fell by 6 % on average in EU countries in 2020.
Elective surgical procedures were also halted, creating a backlog of patients awaiting these interventions.
In 2020, two million fewer elective surgical procedures (such as cataract surgery, and hip and knee replacements) were performed than in 2019 across EU countries — a decrease of one-sixth compared to pre-pandemic volumes.
These “missing volumes” of operations have increased waiting times for patients in need of surgery, increasing patient dissatisfaction.
Many EU countries have provided additional funding to address these backlogs, but the main constraint to scaling up volumes of procedures has been shortages of health workers.
Incentives were provided to staff to work longer hours, but these clearly had limits and ran the risk of leading to burnout and resignation.
In 2020, two million fewer elective surgical procedures (such as cataract surgery, and hip and knee replacements) were performed than in 2019 across EU countries — a decrease of one-sixth compared to pre-pandemic volumes.
These “missing volumes” of operations have increased waiting times for patients in need of surgery, increasing patient dissatisfaction.
On a more positive note, the rapid development of teleconsultations in early 2020 helped to maintain access to care, in particular for patients with chronic conditions.
Although it is encouraging that the vast majority of people who used telemedicine expressed high satisfaction, …
… there are nevertheless concerns that some teleconsultations provide little benefit and that teleconsultations pose risks of widening health inequalities through digital exclusion for older, poorer people and those living in rural areas.
… there are nevertheless concerns that some teleconsultations provide little benefit and that teleconsultations pose risks of widening health inequalities through digital exclusion for older, poorer people and those living in rural areas.
EU countries generally recognised the need to boost resources to respond to the pandemic.
Despite a significant reduction in GDP, per-capita health expenditure increased by over 5 % on average across EU countries in 2020, and by over 10% in Bulgaria, the Czech Republic and Hungary.
However, several of the weaknesses and vulnerabilities identified during the pandemic remain — most notably the widespread shortage of health workers.
Despite a significant reduction in GDP, per-capita health expenditure increased by over 5 % on average across EU countries in 2020, and by over 10% in Bulgaria, the Czech Republic and Hungary.
However, several of the weaknesses and vulnerabilities identified during the pandemic remain — most notably the widespread shortage of health workers.
According to recent OECD estimates, about half of all the new investments required to make health systems more resilient should be devoted to increasing both recruitment and retention of health workers through improved working conditions.
According to recent OECD estimates, about half of all the new investments required to make health systems more resilient should be devoted to increasing both recruitment and retention of health workers through improved working conditions.

Prioritizing the prevention of infectious and non-communicable diseases
Despite much talk of health spending being an investment rather than a cost, policy approaches had not changed significantly before the pandemic.
Health spending remained overwhelmingly focused on curative care, with only 3% of total health spending going toward prevention on average.
Despite much talk of health spending being an investment rather than a cost, policy approaches had not changed significantly before the pandemic. Health spending remained overwhelmingly focused on curative care, with only 3% of total health spending going toward prevention on average.
In 2020, most EU countries substantially increased their spending on prevention, at least temporarily, to fund testing, tracing, surveillance and public information campaigns related to the pandemic.
In 2021, large additional resources were allocated to the roll-out of COVID-19 vaccination campaigns.
In 2020, most EU countries substantially increased their spending on prevention, at least temporarily, to fund testing, tracing, surveillance and public information campaigns related to the pandemic. In 2021, large additional resources were allocated to the roll-out of COVID-19 vaccination campaigns.
The rapid deployment of vaccines was an important contributor to the management of the pandemic: …
… vaccinations were estimated to have prevented over 250 000 deaths across the EU only in 2021, although vaccination rates among vulnerable groups remained quite low in some countries.
… vaccinations were estimated to have prevented over 250 000 deaths across the EU only in 2021, although vaccination rates among vulnerable groups remained quite low in some countries
During the pandemic, many European countries also made substantial progress in vaccinating vulnerable groups against seasonal flu, …
… with the proportion of people aged over 65 vaccinated increasing by over 10 percentage points in several countries.
Despite some temporary challenges in 2021, most European countries were also able to maintain childhood vaccination programmes.
During the pandemic, many European countries also made substantial progress in vaccinating vulnerable groups against seasonal flu, with the proportion of people aged over 65 vaccinated increasing by over 10 percentage points in several countries.
Despite some temporary challenges in 2021, most European countries were also able to maintain childhood vaccination programmes.
One of the lessons from the pandemic is that maximising people’s health and minimising their exposure to risk factors before a crisis is critical.
Obesity and chronic conditions, such as diabetes and respiratory problems, were important risk factors for serious complications and death from COVID-19.
Obesity and chronic conditions, such as diabetes and respiratory problems, were important risk factors for serious complications and death from COVID-19.
The prevention of behavioural and environmental risk factors can go a long way to improving people’s health and reducing the prevalence of chronic diseases and deaths.
Despite progress in reducing smoking rates over the last decades, tobacco consumption remains the largest behavioural risk factor to health, still accounting for about 780 000 deaths per year in the EU.
Alcohol consumption has also been declining over the past decade, but harmful alcohol use is still responsible for nearly 300 000 deaths per year in the EU.
Despite progress in reducing smoking rates over the last decades, tobacco consumption remains the largest behavioural risk factor to health, still accounting for about 780 000 deaths per year in the EU.
Alcohol consumption has also been declining over the past decade, but harmful alcohol use is still responsible for nearly 300 000 deaths per year in the EU.
Environmental factors, such as air pollution and climate change, also have serious consequences on people’s health and mortality.
It is estimated that over 300 000 people in the EU died due to air pollution from fine particulate matters alone in 2019, although this number has fallen in most countries as emissions are declining and air quality is improving.
It is estimated that over 300 000 people in the EU died due to air pollution from fine particulate matters alone in 2019, although this number has fallen in most countries as emissions are declining and air quality is improving.

Monitoring and improving the State of Health in the EU
Health at a Glance: Europe 2022 is the result of ongoing close collaboration between the OECD and the European Commission to improve country-specific and EU-wide knowledge on health issues as part of the Commission’s State of Health in the EU cycle.
Infographic
Foreword
The last two years have seen multiple crises considerably impacting citizens’ physical and mental health, as well as posing a significant threat to the global economy and societal well-being.
As EU and OECD economies gradually recover from the critical phase of the COVID-19 pandemic, their economic and social outlooks have become more uncertain following Russia’s war of aggression against Ukraine.
Major hikes in energy and commodity prices have aggravated inflationary pressures at a time when a cost-of-living crisis was already taking a heavy toll on economies and societies everywhere, and especially low-income households.
As EU and OECD economies gradually recover from the critical phase of the COVID-19 pandemic, their economic and social outlooks have become more uncertain following Russia’s war of aggression against Ukraine.
It is in this uncertain geopolitical, economic and public health environment that we are releasing this 2022 edition of Health at a Glance: Europe, a visible output of the continued strong collaboration between the European Commission and the OECD.
Promoting better public health and stronger health systems in Europe and around the world remain strategic priorities for both the European Commission and OECD.
Moreover, for the first time, this edition of Health at a Glance: Europe reports key indicators of health and health systems for Ukraine and Moldova.
The focus of this edition is on:
- Strengthening the resilience of health systems, crisis preparedness and response capacity through targeted investments;
- Promoting better prevention and treatment of cancer and other non-communicable diseases;
- Preventing and addressing mental health challenges in the aftermath of the pandemic and in the current context of multiple crises;
- Supporting the digital transformation of health systems to make the most out of health data and new digital tools; and
- Recognising the importance of regional, national, European and broader international efforts to address global public health threats.
The 5 key recommendations are:
- 1.Strengthening health system resilience
- 2.Promoting better prevention and management of non-communicable diseases
- 3.Improving mental health
- 4.Supporting the digital transformation of health systems
- 5.Strengthening national, European and global efforts to prepare for future health threats

1.Strengthening health system resilience
The pandemic has exposed weaknesses and vulnerabilities in health systems created by years of underfunding across the board, as well as the inadequacy of planning and co-ordination mechanisms for developing effective responses to cross-border public health emergencies.
In response, and building on the experiences of the COVID-19 pandemic, the European Commission and Member States have begun the process of building a strong European Health Union.
This includes an ambitious package of measures aimed at providing the EU with better instruments for detecting and responding to future infectious disease outbreaks, which is underpinned by a new EU health security framework to manage serious cross-border health threats.
The OECD has highlighted the urgent need for smart investments in health systems to protect people’s health, strengthen the foundations of health systems, and empower health professionals working on the frontline.
According to OECD estimates, the costs of deploying these necessary investments in prevention, health workforce and health system digitisation would amount to around 1.4% of pre-pandemic GDP, on average across OECD countries.
According to OECD estimates, the costs of deploying these necessary investments in prevention, health workforce and health system digitisation would amount to around 1.4% of pre-pandemic GDP, on average across OECD countries.
Targeted spending must be combined with effective prevention interventions and measures to reduce wasteful spending to ensure that health systems remain fiscally sustainable in the medium to long term.
Targeted spending must be combined with effective prevention interventions and measures to reduce wasteful spending to ensure that health systems remain fiscally sustainable in the medium to long term.
The Recovery and Resilience Facility is the EU’s direct response to the COVID-19 crisis, which focuses on accelerating the green and digital transitions as well as building health system resilience.
To date, EUR 40 billion have been set aside in EU Member States’ Recovery and Resilience Plans to support health investments and reforms.
In parallel, the ambitious and standalone EU4Health programme will fund actions aimed at building stronger and more sustainable health care systems that deliver better care for EU patients.
To date, EUR 40 billion have been set aside in EU Member States’ Recovery and Resilience Plans to support health investments and reforms.

2.Promoting better prevention and management of non-communicable diseases
We cannot allow the pandemic to distract us from the fact that non-communicable diseases (NCDs) continue to account for 80% of the overall burden of disease in Europe.
In February 2021, the European Commission launched Europe’s Beating Cancer Plan, setting out a new EU approach to cancer prevention and treatment.
The plan is designed to address the entire disease pathway, from prevention to quality of life of cancer patients and survivors, focusing on actions where the EU can add the most value for patients and their families.
In this context, the OECD is collaborating closely with the European Commission to launch the Cancer Inequalities Registry, a flagship initiative of the Europe’s Beating Cancer Plan to monitor trends and inequalities in cancer prevention and care throughout Europe.
We cannot allow the pandemic to distract us from the fact that non-communicable diseases (NCDs) continue to account for 80% of the overall burden of disease in Europe.
In February 2021, the European Commission launched Europe’s Beating Cancer Plan, setting out a new EU approach to cancer prevention and treatment.
In June 2022, the European Commission presented the Healthier Together initiative to address other major NCDs in the EU, such as cardiovascular diseases, diabetes and respiratory diseases, as well as mental health and neurological disorders.
Tackling these conditions requires both greater prevention and improved disease management.
… tackling major NCDs — such as cardiovascular diseases, diabetes and respiratory diseases, as well as mental health and neurological disorders — requires both greater prevention and improved disease management.
Historically, there has been an under-investment in prevention …
… OECD data shows that only about 3% of health spending on average in EU and OECD countries were allocated to prevention activities before the pandemic.
The OECD has for many years made the economic case for investing in disease prevention and tackling risk factors, and it is encouraging that as much of 20% of the EU4Health programme budget is allocated to health promotion and disease prevention.
The OECD is also working with countries to more systematically measure the experiences and outcomes of people with chronic conditions in primary care through the Patient-Reported Indicators Surveys (PaRIS).
Historically, there has been an under-investment in prevention … OECD data shows that only about 3% of health spending on average in EU and OECD countries were allocated to prevention activities before the pandemic.
… it is encouraging that as much of 20% of the EU4Health programme budget is allocated to health promotion and disease prevention.
Together, EU Member States and OECD countries can reduce the burden of cancer and other NCDs and strive to achieve the UN Sustainable Development Goals (SDGs) and in particular SDG 3.4 which aims to reduce NCD-related premature mortality by one-third by 2030.

3.Improving mental health
Anxiety and depression have significantly increased in all EU countries during the pandemic, affecting young people especially young women and those facing financial difficulties.
Symptoms of anxiety and depression amongst young people more than doubled in several European countries during the pandemic.
Disruptions in, and growing demand for, mental health support have challenged already-stretched mental health care services, resulting in nearly half of all young Europeans reporting unmet needs for mental health care in the spring of 2022.
Disruptions in, and growing demand for, mental health support have challenged already-stretched mental health care services, resulting in nearly half of all young Europeans reporting unmet needs for mental health care in the spring of 2022.
We need to take better care of each other, across all generations.
This edition of Health at a Glance: Europe makes a strong case for taking bold actions to respond to the mental health needs of young people and ensure the pandemic does not leave permanent scars on the aspirations and outcomes of the new generation.
This edition of Health at a Glance: Europe makes a strong case for taking bold actions to respond to the mental health needs of young people and ensure the pandemic does not leave permanent scars on the aspirations and outcomes of the new generation.
Following the call of the President of the European Commission Ursula von der Leyen in her 2022 State of the Union address for a more comprehensive approach to mental health for the EU, the European Commission has started necessary preparatory work so that we are well equipped to tackle this multifaceted challenge.
OECD work setting a new benchmark for mental health systems highlights critical areas where better evidence needs to be developed and new effective mental health strategies put in place.
The OECD Council Recommendation on Integrated Mental Health, Skills and Work Policy calls for governments to promote the provision of early and fully integrated services to improve the social and labour market outcomes of people with mental health issues.
…the European Commission has started necessary preparatory work so that we are well equipped to tackle this multifaceted challenge.

4.Supporting the digital transformation of health systems
We don’t know when the next crisis will be, but we know that better data and greater use of digital tools in the health sector will be vital to prepare for future shocks.
The COVID-19 pandemic has highlighted the need to improve the timeliness of health data to provide the right information to the right people at the right time.
The COVID-19 pandemic has highlighted the need to improve the timeliness of health data to provide the right information to the right people at the right time.
To unleash the full potential of health data, in May 2022 the European Commission proposed a regulation to set up a European Health Data Space.
Under this framework, citizens’ control of their own health data will be strengthened, and the secure use of health data for purposes of research, innovation, policy making and regulatory activities will be enabled.
To unleash the full potential of health data, in May 2022 the European Commission proposed a regulation to set up a European Health Data Space.
Likewise, the 2017 OECD Council Recommendation on Health Data Governance laid out a framework to encourage greater availability of timely health data within countries and across borders, while ensuring the protection of patients’ privacy and the security of sensitive data.
The OECD is supporting countries’ progress to implement national Health Data Governance frameworks.
Likewise, the 2017 OECD Council Recommendation on Health Data Governance laid out a framework … and
The OECD is supporting countries’ progress to implement national Health Data Governance frameworks.
New digital technologies, such as teleconsultations and other forms of telemedicine, have already transformed people’s experiences of health care.
The number of teleconsultations with doctors nearly doubled during the first year of the pandemic, and will undoubtedly play a crucial role in making health services more accessible also in the future.
The number of teleconsultations with doctors nearly doubled during the first year of the pandemic, and will undoubtedly play a crucial role in making health services more accessible also in the future.

5.Strengthening national, European and global efforts to prepare for future health threats
The pandemic has clearly highlighted that health is the foundation upon which resilient, productive and fair economies and societies are built.
However, emerging pathogens, climate change and other public threats know no borders.
The pandemic has clearly highlighted that health is the foundation upon which resilient, productive and fair economies and societies are built.
However, emerging pathogens, climate change and other public threats know no borders.
To secure the health of all people, we must tackle health globally.
The new EU Global Health Strategy is fully aligned with the OECD strategic objective of improving health systems to more effectively prevent and respond to global health threats, as well as combat infectious and non-communicable diseases.
The European Commission and the OECD will continue to work with the WHO and other partners to promote robust actions to secure the health of people in Europe and around the world — actions rooted in the universal values of inclusive growth and equal opportunities for all, human rights and co-operation.
The European Commission and the OECD will continue to work with the WHO and other partners to promote robust actions to secure the health of people in Europe and around the world — actions rooted in the universal values of inclusive growth and equal opportunities for all, human rights and co-operation.
Mathias Cormann, OECD Secretary-General
Stella Kyriakides, European Commissioner for Health and Food Safety
Foreword by
Mathias Cormann, OECD Secretary-General
Stella Kyriakides, European Commissioner for Health and Food Safety
Acknowledgements
Health at a Glance: Europe 2022 marks the start of a new State of Health in the EU cycle — an initiative launched by the European Commission, in co-operation with the OECD and the European Observatory on Health Systems and Policies, to assist EU Member States in improving the health of their citizens and the performance of their health systems.
While the preparation of this publication was led by the OECD, the European Commission provided guidance and substantive inputs throughout the process, as well as financial support via the EU4Health Programme.
This publication would not have been possible without the efforts of national data correspondents from the 38 countries covered in this report who have provided most of the data and metadata.
We are also grateful to all the national officials who have provided helpful comments on a draft of this report.
This report was prepared by a team from the OECD Health Division under the co-ordination of Gaétan Lafortune.
Chapter 1 on the impact of the pandemic on young people’s health was prepared by Doron Wijker and Eileen Rocard.
Chapter 2 on the disruptions of health services during the pandemic for non-COVID patients was prepared by Lucie Bryndová and Noémie Levy. Eileen Rocard prepared
Chapter 3 on the health status of populations.
Chapter 4 on risk factors was prepared by Marion Devaux and Noémie Levy, with input from Joao Matias from the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) for the indicator on illicit drug consumption among adults. Caroline Penn, Michael Mueller and David Morgan prepared
Chapter 5 on health expenditure and financing.
Chapter 6 on effectiveness and quality of care was prepared by Rie Fujisawa, Kadri-Ann Kallas, Kate de Bienassis, Eliana Barrenho, Anamaria Verdugo, Constanza Salas Ramos, Candan Kendir and Noémie Levy.
Chapter 7 on accessibility was prepared by Gaétan Lafortune, Michael Mueller, Gaëlle Balestat, Marie-Clémence Canaud, Noémie Levy and Caroline Berchet, with input from Sarah Thomson and Jorge Alejandro Garcia on behalf of the WHO Barcelona Office for Health Systems Strengthening for the indicator on the financial burden of out-of-pocket spending.
Chapter 8 on resilience was prepared by Philip Haywood, Hansol Min, David Morgan and Gaëlle Balestat.
This publication benefited from useful comments from Francesca Colombo and Frederico Guanais from the OECD Health Division.
Many useful comments were also received from Maya Matthews, Dirk Van den Steen and Federico Pratellesi from the State of Health, European Semester and Health Technology Assessment unit in the European Commission‘s Health and Food Safety Directorate General.
Editorial assistance was provided by Marie-Clémence Canaud, Lucy Hulett and Alastair Wood from the OECD Health Division.