institute for health transformation
(inHealth)
research, strategy and advisory consulting
Joaquim Cardoso MSc
January 18, 2023
SOURCE:
Beckers Hospital Review
Alan Condon
January 18, 2023
Hospitals and health systems are increasing spending on technology and software that can improve productivity and alleviate cost and labor pressures.
While large, urban health systems ramped up tech investments during the pandemic, smaller, rural systems with tighter budgets hit reduced spending to balance investment priorities with financial pressures.
But many systems that paused tech spending have fallen behind on pre-pandemic investment strategies and are struggling to navigate an explosion of vendor offerings.
But many systems that paused tech spending have fallen behind on pre-pandemic investment strategies and are struggling to navigate an explosion of vendor offerings.
However, over the last year or so, as pandemic conditions eased, many providers have ramped up software investments, according to the report.
About 45 percent of providers accelerated software investment over the past year, with only 10 percent decelerating spending.
Of those accelerating investments over the past year, almost 80 percent cite inflation, staffing shortages or specific organizational situations — such as leadership changes or a merger/acquisition — as the top catalysts spurring new investments.
About 45 percent of providers accelerated software investment over the past year, with only 10 percent decelerating spending.
Of those accelerating investments over the past year, almost 80 percent cite inflation, staffing shortages or specific organizational situations — such as leadership changes or a merger/acquisition — as the top catalysts spurring new investments.
This year, 95 percent of providers are expected to purchase new technologies; those that can improve productivity or reduce labor costs are in high demand.
Providers cited revenue cycle management, patient intake/flow, clinical systems and telehealth as the most strategically important investments.
Providers cited revenue cycle management, patient intake/flow, clinical systems and telehealth as the most strategically important investments.
Artificial intelligence-powered scheduling, virtual nurses, remote patient monitoring and chatbots designed to provide medical advice to pregnant patients are among the health system investments Becker’s Hospital Review has reported on in the last month.
Artificial intelligence-powered scheduling, virtual nurses, remote patient monitoring and chatbots designed to provide medical advice to pregnant patients are among the health system investments Becker’s Hospital Review has reported on in the last month.
Rising investment in these technologies confirms that healthcare operations significantly affect a health system’s overall financial health.
Originally published at https://www.beckershospitalreview.com on January 18, 2023.
DEEP DIVE

2022 Healthcare Provider IT Report: Post-Pandemic Investment Priorities
Post-Pandemic Investment Priorities
As healthcare providers enter a new period of disruption, their software investment priorities present opportunities for vendors and investors.
By Eric Berger, Laila Kassis, Aaron Feinberg, Michael Brookshire, John Day, and Rebecca Hammond
October 17, 2022
At a Glance
- As healthcare providers emerge from a global pandemic, they are doubling down on software investments, even in the face of macroeconomic turbulence.
- Providers are focusing investments on revenue cycle management, patient intake, and cybersecurity.
- Providers are increasingly streamlining bloated tech stacks and looking to their electronic medical records (EMR) providers and other existing vendors for new solutions before evaluating new vendor offerings.
- Competition in the provider IT space shows no signs of abating: Early-stage capital, big tech, and scale EMR players continue crowding into more segments.
- This has significant implications for providers as they transition into a new disruptive period, …
- … for software players as they fine-tune go-to-market models for the current environment, and …
- … for private equity investors as they look to invest behind winning themes.
Covid-19 radically stretched healthcare providers in countless ways, including accelerating digitization and changing patient expectations about care delivery.
Some organizations adopted multiple systems to keep pace with the changes; others pressed pause.
Both sets of organizations are now regrouping, looking to be more focused with their investments and streamline their existing tech stacks.
Provider organizations, regardless of size or sophistication, are emerging from the pandemic and taking stock of the software solutions they’ll need in the long term and determining where and how to invest.
As part of this reflection, many are seeking to better integrate new solutions and rationalize vendors.
In the short term, clinician shortages and wage inflation are driving demand for solutions that improve productivity and alleviate labor needs.
Against this backdrop, vendors face growing competition from large electronic medical record (EMR) incumbents pursuing product adjacencies, big tech, and innovative venture capital–funded start-ups.
In the current environment, it is critical that vendors understand the investment posture of their customers, properly segment them based on their needs and behaviors, and refine go-to-market (GTM) models by articulating their differentiated value proposition in a crowded field.
The healthcare information technology (HCIT) space has been historically attractive for investors, and it is expected to remain so despite recent macroeconomic turbulence.
Investors must maintain discipline amid this uncertainty and continue to pursue attractive themes while assessing the impact of potential headwinds from market conditions, rising vendor rationalization, and the risk of being boxed out from existing provider solutions (especially EMRs) as part of diligence.

From Disruption to Disruption: How Provider IT Priorities Are Evolving
Post–Covid-19, providers are doubling down on software investments
Covid-19 led to a bifurcation in providers’ approaches to their software investments. Larger, urban organizations with a more innovative orientation accelerated HCIT investments during the pandemic. Citing the challenges posed by Covid-19, they focused on telehealth, clinical systems, and clinical decision support.
Smaller, rural organizations with tighter budgets tapped the brakes during the pandemic, balancing investment priorities with financial pressures. Many of these providers have fallen behind on pre–Covid-19 investment roadmaps and are struggling to navigate an explosion of vendor offerings.
As pandemic conditions eased, many providers ramped up their software investments. Some 45% of providers accelerated software investment over the past year, with only 10% decelerating their spending. This signals a turning point in the provider IT market as we emerge from the pandemic, with forward-thinking providers doubling down on technology roadmaps and many who spent the past few years on the sidelines looking to retool software roadmaps for a “new normal” that presents a host of new challenges, including macroeconomic pressures and long-term shifts in ways of working.
Some 45% of providers accelerated software investment over the past year, with only 10% decelerating their spending.
Of those accelerating investments over the past year, nearly 80% cite labor shortages, or inflation concerns, or specific organizational situations (e.g., M&A, change in leadership) as the top catalysts spurring new investments (see Figure 1). Covid-19–era staffing shortfalls and burnout among physicians, nurses, and other clinicians, as well as IT and office personnel, continue to plague providers. These shortages led to a pandemic-era spike in wage inflation, which has been further exacerbated by rising wages and product cost inflation in the broader economy over the past 12 to 18 months. As a result, providers are looking to software solutions to boost productivity and automate tasks, with the ultimate goal of stronger financial outcomes and higher-quality patient care.
Figure 1: Covid-19 bifurcated software spending, but nearly 45% of providers claim that they spent more on software over the past year
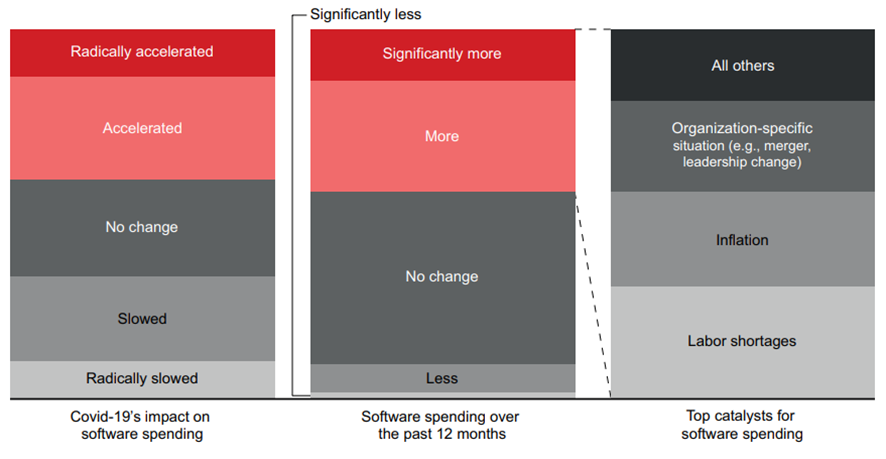
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Additionally, the past few years also led to a variety of organizational shifts, including a flurry of leadership changes and retirements by provider executives who had prolonged their careers to lead their organizations through the pandemic, as well as a spike in consolidation as M&A activity boomed. In connection with these changes, many providers are revisiting strategic plans and making investments to integrate acquisitions into more sophisticated parent company tech environments.
Software is now a top five strategic priority for nearly 80% of provider organizations and a top three priority for almost 40% (see Figure 2). Concerns about the macroeconomic environment are having an impact on investment plans. For now, though, we see few signs of a broad-based slowdown on provider software roadmaps.
Providers have displayed resilience during past recessions despite some adverse impact around elective procedure volumes and declining commercial insurance coverage amid rising unemployment. Uncertainty remains, however, in the current environment. The modern provider IT market has not experienced a pronounced period of high inflation, potentially tipping into a recession. Similar to what we saw during the Covid-19 pandemic, our research indicates that a prolonged period of market turbulence would likely lead to a bifurcation of software investment postures, with large, sophisticated providers accelerating investments and smaller providers hitting the brakes. This would result in a further widening of the gap between how different types of provider organizations use technology to deliver care, support clinicians and administrative staff, and boost the bottom line.
Figure 2: Healthcare IT is a top 3 strategic priority for almost 40% of providers and a top 5 priority for nearly 80%
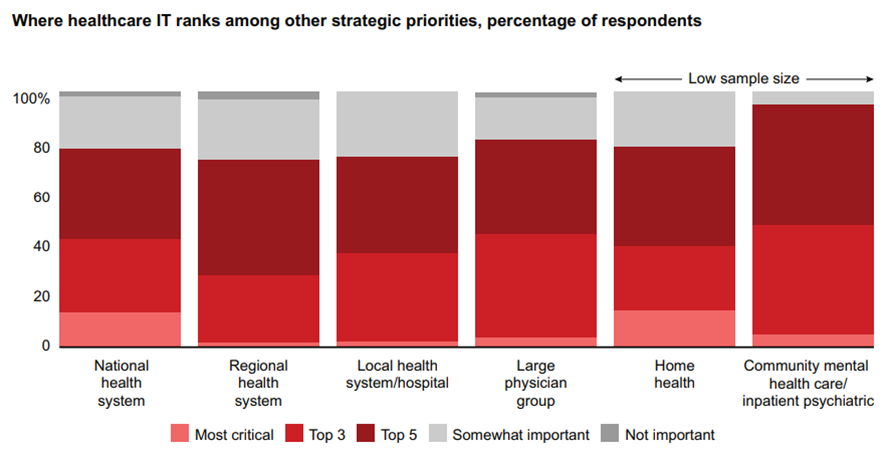
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Over the next year, more than 95% of providers expect to make new software investments, with one-third planning significant new investments (see Figure 3). Roughly 35% of providers say that because of the current environment, they plan to spend more than usual over the next 12 months as they seek productivity and efficiency improvements to address rising margin pressure and labor tightening. About 30% say that they will likely spend less than they would in more favorable conditions over the next year.
Leading hospitals, academic medical centers, and large physician groups will especially continue to prioritize clinical outcomes and innovation during a recession. Most other hospitals and midsized physician groups will continue executing on current investment plans, although they may be more budget conscious. At the tail, some smaller hospitals and provider groups with tight budgets might halt investments entirely.
Figure 3: A third of providers expect to make significant software investments, but the effect of macro conditions on spending varies
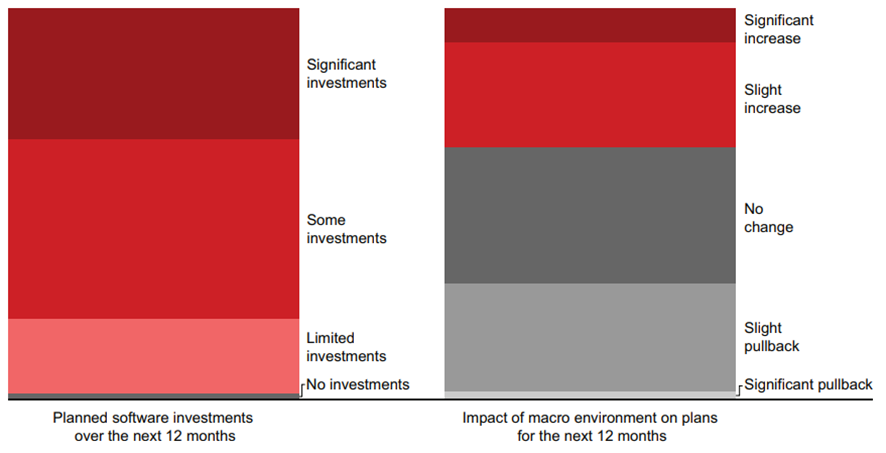
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)

Where spending is happening: Priority categories for the next year
Providers cite revenue cycle management (RCM), security and privacy, patient intake/flow, clinical systems, and telehealth as the most strategically important categories for software investment over the next year (see Figure 4).
Revenue cycle management software is critical in the current environment given the direct link with cash collections as well as the labor-intensive nature of revenue cycle processes. This is especially true for smaller provider organizations navigating complex payer landscapes and physician groups that lag health systems on the adoption of RCM software. Large health systems also continue to make investments in RCM, however, via both business process outsourcing and adoption of enhanced RCM software modules (e.g., complex claims, artificial intelligence–enhanced features). Providers of all types cited RCM as a top priority for the next year, pointing to a broad set of specific priorities, including revenue integrity, charge capture, and complex claims, and underscoring a robust set of RCM needs across the provider ecosystem.
Figure 4: Top provider investment priorities over the next 12 months
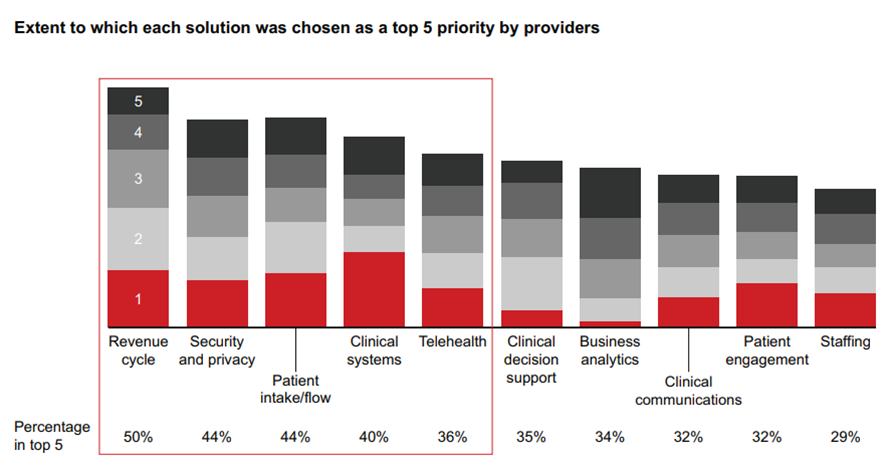
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Security and privacy software is another top investment priority for providers over the next year. Even before Covid-19, providers were vulnerable to cyberattacks. But the risks have risen. And as a result of the increase in the number of nodes in provider tech ecosystems, there’s been a surge in security breaches. From 2018 to 2021, the number of data breaches reported by providers to the US Department of Health and Human Services’ Office for Civil Rights has nearly doubled for incidents impacting 500 or more medical records. Additionally, provider data breaches are getting more expensive. According to data from IBM, the average cost of a provider data breach has now surpassed $10 million, up nearly 40% since 2020. Our research shows that regional health systems, freestanding hospitals, and mental health providers are especially focused on security and privacy investments, especially in areas such as cybersecurity, IoT security, and patient privacy monitoring.
Patient intake/flow software remains another critical area for investment. Covid-19 stretched hospital capacity to the max while also driving the need for enhanced virtual intake processes. As a result, providers continue to invest in patient flow systems and are also investing heavily in patient intake management tools and patient portals. Many providers are recognizing the importance of simplifying intake processes to accelerate cash collections and provide more seamless patient experiences in a world where patients increasingly expect to navigate the health system like consumers.
Clinical systems remain a top investment priority, with providers citing EMRs as their primary investment area. While a few providers are making first-time investments in EMR solutions, most are planning investments focused on optimizing existing EMR systems to streamline provider workflows and boost productivity, extending core EMR environments to recently acquired entities, or even switching EMR vendors altogether.
Telehealth, while having declined in importance since the nadir of the Covid-19 pandemic, remains a critical strategic priority. Large national health systems view telehealth systems as integral to care delivery and are looking to bolster existing video consultation/collaboration platforms and add enhanced telehealth capabilities. Given the value of greater integration between care delivery platforms and EMRs, some large providers appear to be reconsidering the virtual care platforms offered by their EMRs. This suggests that some large EMR players, particularly Epic, are improving telehealth platforms that were insufficient for providers during the early days of Covid-19.
While each of these priorities is broadly relevant across a wide variety of organizations, certain priorities are uniquely important to different types of providers (see Figure 5).
Figure 5: Certain investment priorities are uniquely important to different provider types
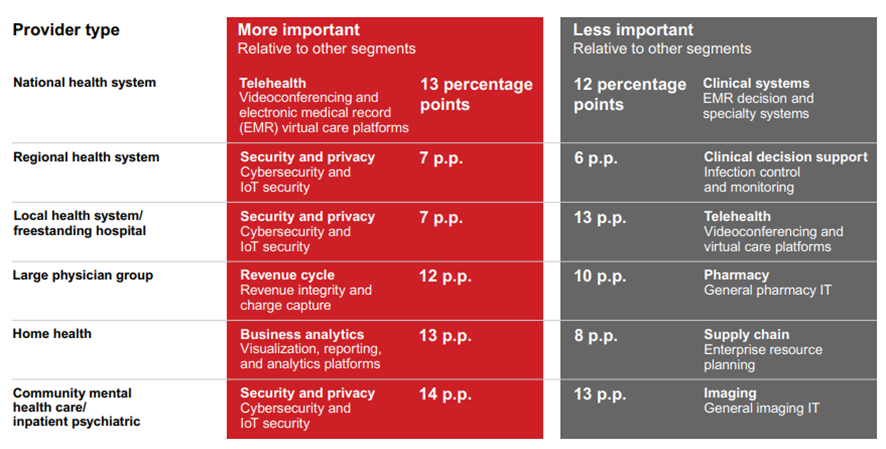
Note: Percentage-point differences were calculated by comparing the percentage-point delta for provider type importance to the average importance across all other provider segments
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Figure 6: Provider software buyer archetypes based on organizational and behavioral characteristics
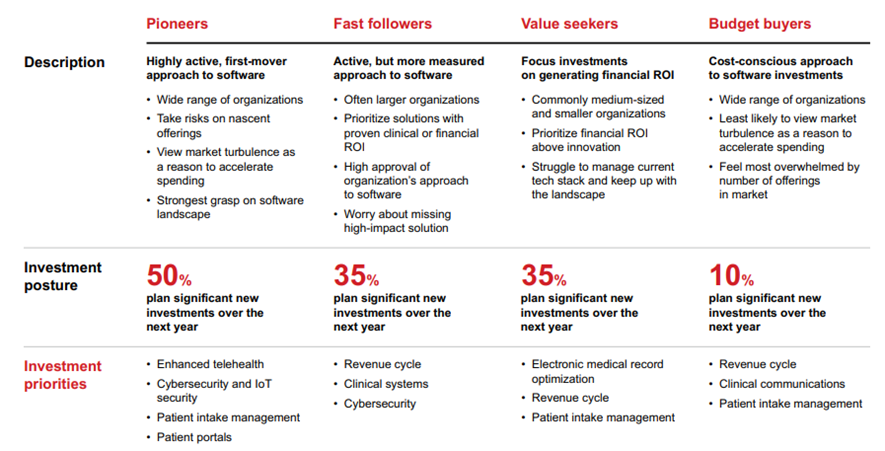
Note: Investment posture percentages for fast followers, value seekers, and budget buyers were rounded to the nearest 5 Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
In addition, further nuances exist based on a broader matrix of provider organizational features and behavioral characteristics, which are critical for software vendors to consider when fine-tuning offerings and value propositions to meet the needs of customers. Four provider archetypes emerged from our research based on their orientations toward making software investments (see Figure 6).

How providers spend is evolving: The impact of vendor proliferation and complex tech stacks
While the outlook for provider software investments is strong, vendor proliferation and expanding tech stacks are driving changes in how providers plan to make software investments over the next year.
According to our research, more than 50% of providers are struggling with the flood of offerings in the market: They cite concerns about missing high-impact new solutions or simply feeling overwhelmed by the number of offerings to evaluate.
Additionally, during the pandemic, many providers adopted new technology solutions across a broad set of clinical and operational areas.
As a result, many are emerging from Covid-19 with greater complexity in their tech stacks than ever before. In fact, a quarter of all providers claim that their existing tech stacks keep them too busy to stay current on new offerings in the market (see Figure 7).
Tangentially, providers cite lack of cross-solution interoperability and poor EMR integration with existing tech stacks as some of the top pain points with their existing tech stacks, further illustrating the unique challenge of the current environment (see Figure 8).
While the 21st Century Cures Act offers some promise for beginning to address these issues, material change has not yet occurred, and many providers remain skeptical about whether this regulation will bring about a real shift.
Figure 7: Providers see challenges with vendor proliferation and an increase in tech stack complexity
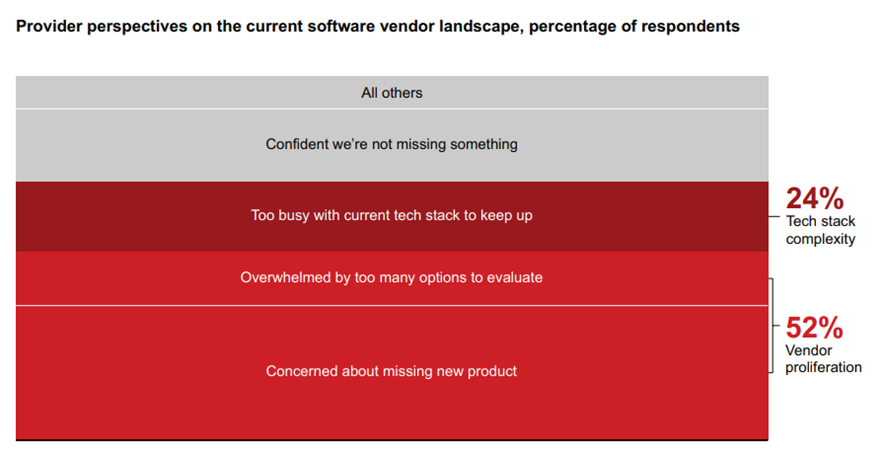
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Providers are responding to these challenges in various ways (see Figure 9).
- Many plan to increasingly look to existing vendors with proven solutions before considering offerings from new vendors (around 72% of providers).
- Second, and more specifically, many plan to look to their EMRs for new solutions before looking to others (around 71% of providers). While provider tech stacks have become larger and more sophisticated, EMRs remain the single most critical software solution for most providers. Our research shows that many providers are taking a second look at new or enhanced offerings from their EMRs in areas such as telehealth.
- Thirdly, some providers are making plans to streamline the number of third-party software solutions in their tech stacks over the next year (around 63% of providers).
Figure 8: Interoperability and electronic medical record integration are top pain points for providers with their existing third-party tech stacks
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Figure 9: How providers are responding to rising vendor proliferation and increasing complexity in their tech stacks
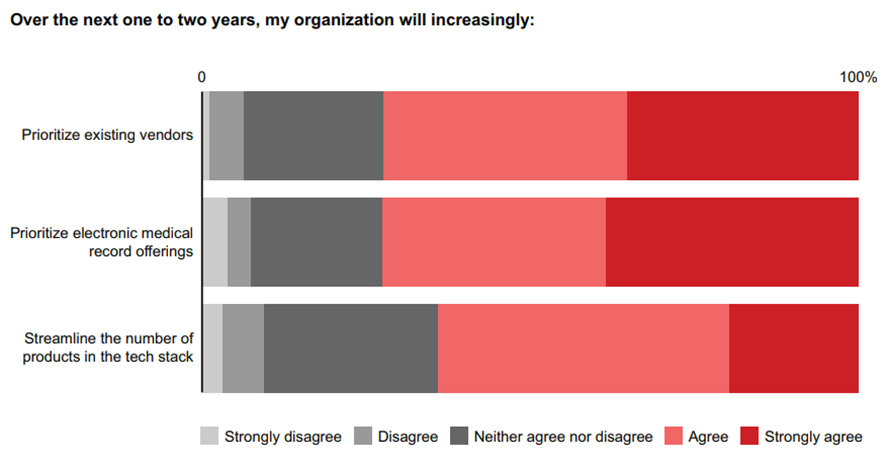
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Competitive pressures in the provider software space show no signs of abating
Providers should expect continued vendor proliferation, and incumbent software providers should continue to expect rising competitive pressures caused by three primary forces: big tech, leading EMRs, and start-ups.
Big tech: Big tech players (including Amazon, Microsoft, Google, and Apple) have been pushing into healthcare in recent years with targeted offerings and investments (see Figure 10). In general, they have focused on building upon core competencies — such as cloud services, data storage, customer relationship management (CRM), consumer devices, and wearables — to fill in the white space rather than going headto-head with entrenched incumbent enterprise software providers. This is evident in the development of healthcare-specific cloud offerings from cloud service providers (e.g., Amazon’s AWS for Health, Microsoft’s Azure for Healthcare) or in the development of an increasing number of healthcare mobile apps that make it easier for patients to share health data with providers (e.g., Apple Health).
More recently, however, big tech has been investing in healthcare capabilities further afield from core capabilities, especially via M&A activity, reflecting the growing attractiveness of the healthcare market.
Figure 10: Big tech has increasingly pushed into healthcare in recent years, making many significant investments since 2020
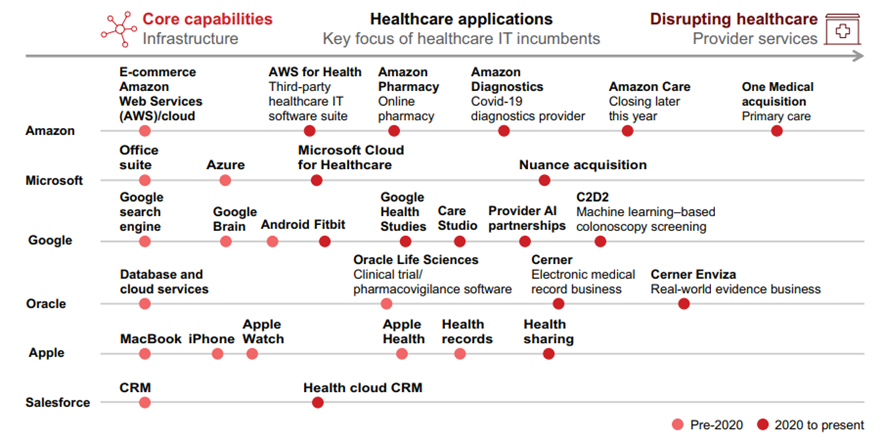
Sources: Company websites; financial filings; press releases
In 2022, Microsoft bought artificial intelligence and speech recognition software company Nuance (March), Oracle acquired EMR giant Cerner (June), and Amazon announced plans to purchase tech-enabled primary care provider One Medical (July, abandoning its attempt at building a scale in-house platform, Amazon Care).
According to Microsoft, its acquisition of Nuance will double the tech giant’s addressable market in healthcare to almost $500 billion given the use of Nuance products in more than 75% of US hospitals. Similarly, Oracle’s purchase of Cerner will expand its provider customer base to include additional hospitals in which the EMR giant is entrenched. The deal could also position Oracle for more ambitious moves in the healthcare software space given Cerner’s investments around new growth horizons, including real-world evidence (Cerner Enviza).
Amazon’s announced $3.9 billion deal to acquire primary care player One Medical, which has its own EMR platform, signals that the e-commerce and cloud giant is serious about becoming a key player in the provider space.
While big tech appears increasingly serious about pushing into healthcare, we believe that the threat to traditional provider software players is minimal in the immediate term, especially when looking at providers’ top 10 strategic investment priorities for the next year in which big tech’s current positioning lags market leaders (see Figure 11).
It remains to be seen how software providers will respond to big tech encroaching on their territory and how patients would feel about big tech companies having access to some of their most sensitive data.
There are exceptions, however, where providers’ top software investment priorities align with the core capabilities of big tech players. For example, Microsoft was quick to position Microsoft Teams as a critical telehealth platform during Covid-19, and it appears well positioned in the space as we emerge from the pandemic. CRM solutions leader Salesforce could have a strong claim on winning in patient engagement. (CRM is a category some healthcare providers have long neglected but are growing increasingly interested in as a means of enhancing patient experience.) With its acquisition of Cerner, Oracle is primed to grow its share of the health system enterprise resource planning space. It remains to be seen how software providers will respond to big tech encroaching on their territory and how patients would feel about big tech companies having access to some of their most sensitive data.
Figure 11: Big tech’s current positioning lags market leaders in many of providers’ top strategic priorities for this next year
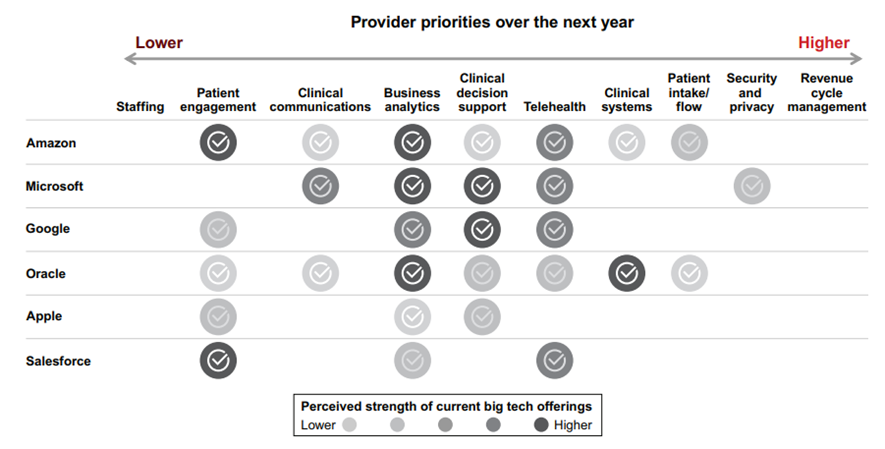
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289); company websites; financial filings; press releases
Ultimately, while we do not see big tech capturing a significant share of the enterprise provider IT space in the immediate term, providers and incumbent software players should not underestimate cash-rich big tech players, especially in an environment of depressed valuations.
EMRs, especially Epic, are expanding offerings: Over the past decade, Epic has become the market leader in acute and ambulatory EMR, where it has gained formidable share from competitors (see Figure 12). Beyond reinforcing its strong core offering and providing exceptional customer service, Epic has aggressively pursued product adjacencies to elevate its value proposition beyond core EMR. Over the years, Epic has developed new products catering to a wide range of needs, spanning RCM, data analytics, patient portals, clinical communications, and clinical department modules (e.g., cardiology), and it is continuing to expand its reach across an ever-increasing set of areas.
What’s next? While that’s impossible to predict with any certainty, many of Epic’s successful product expansions were strong across three dimensions.
· Table stakes: Does the potential expansion area under consideration meet basic prerequisites for engagement (i.e., product synergy with Epic’s core EMR platform, leverages existing sales channels and customer relationships, and enhances or defends the core product)?
Figure 12: Epic has gained share rapidly in recent years, with most provider executives preferring it to other top solutions
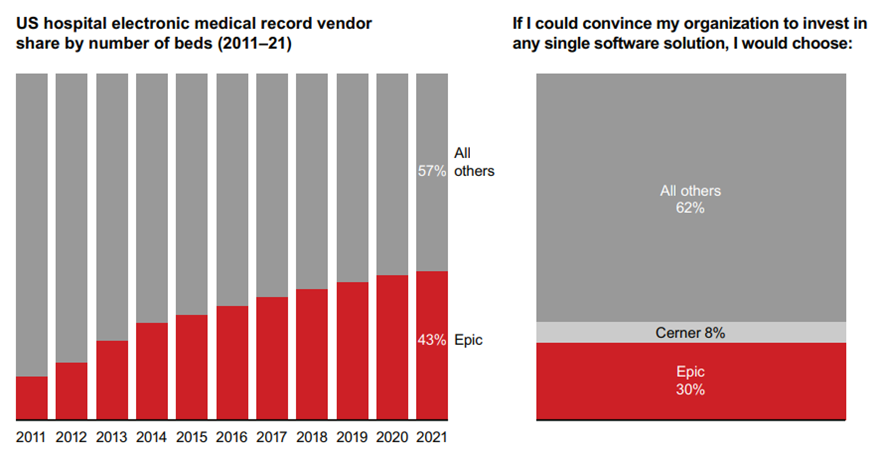
Sources: Bain experience; Bain-KLAS 2022 Provider Executive Survey (N=289)
· Ability to win: Does Epic have a high likelihood of success in this expansion (e.g., low context dependency, low switching costs, manageable complexity, proven capabilities)?
· Other strategic imperatives: Does the expansion area present other attractive characteristics (e.g., large addressable market, low regulatory exposure, limited security risks)?
While we cannot predict Epic’s future product roadmap, our research suggests that Epic and other scale EMRs will continue being spoilers to point solution software providers operating in close proximity to Epic’s ever-expanding core.
Provider pain points around vendor proliferation could play into Epic’s hand: Again, as Figure 9 showed, more than 70% of providers expect to look to their EMRs for new solutions before taking meetings with point solution providers over the next one to two years. This is truer of Epic customers than any other, including Cerner (see Figure 13).
Additionally, as provider needs have evolved, EMRs have made investments to position themselves accordingly. This is especially true in telehealth, where some health systems adopted point solution offerings. Our research indicates that some providers are revisiting EMR telehealth offerings, which could benefit Epic given recent investments in its offering
Figure 13: Epic customers are most likely to look to their electronic medical record before evaluating new software solutions
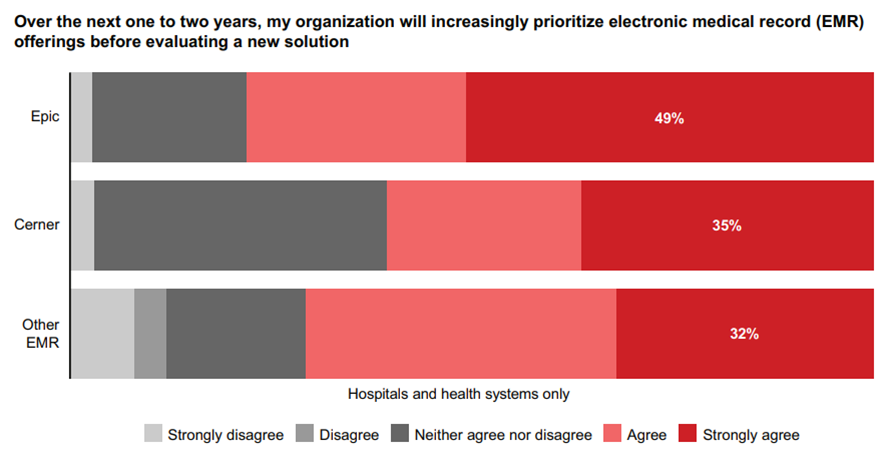
Sources: Provider interviews; Bain-KLAS 2022 Provider Executive Survey (N=289)
Capital continues flowing into early-stage tech offerings: Besides competition from big tech and scale EMRs, provider software players face pressure — and see opportunities — from an increasingly robust health tech start-up ecosystem.
In recent years, early-stage capital has poured into healthcare technology solutions, reshaping the landscape for providers and incumbent software players alike. According to Silicon Valley Bank, between 2019 and 2021, early-stage health tech activity increased from nearly $11 billion to nearly $40 billion. Even amid a difficult start-up funding environment, first-half 2022 funding reached nearly $18 billion, almost surpassing full-year 2020 activity (see Figure 14).
Provider technology funding has been especially active, comprising more than half of deal value from 2019 to 2021 and during the first half of 2022. Provider technology is also a key area in early-stage deals, making up more than 50% of seed/Series A rounds. Most provider technologies receiving funding coalesce around alternative care and provider operations, with later-stage venture activity skewing toward alternative care as a robust funding environment brought an explosion of digital health activity and early-stage provider IT funding slanting toward provider operations solutions.
Figure 14: Early-stage funding for provider IT has erupted in recent years
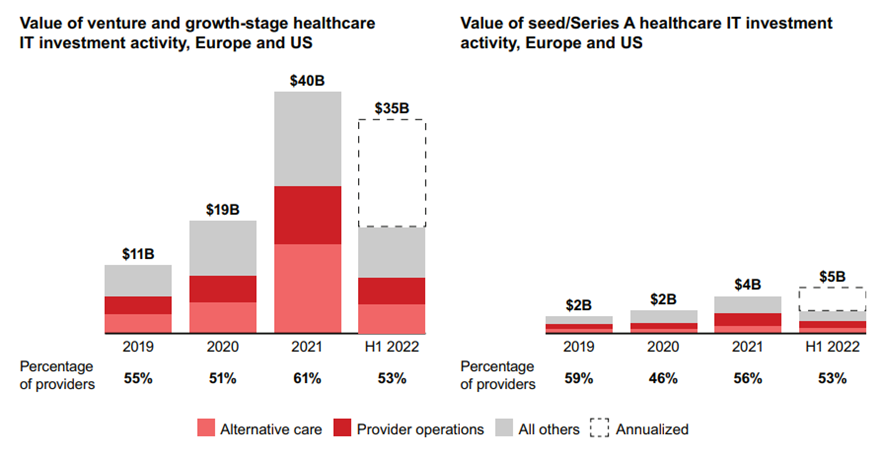
Sources: Silicon Valley Bank; Bain analysis
While uncertainty surrounds the second-half 2022 funding environment, we believe early-stage players will remain a formidable force in the provider IT market. Incumbent vendors would be prudent to keep tabs on early-stage players with disruptive potential and stay active in exploring partnership or acquisition opportunities. With healthcare providers desiring fewer, more meaningful software vendor relationships, savvy incumbents can use tuck-in acquisitions to improve customer stickiness.
Key Implications and Opportunities for Providers, Vendors, and Investors
Providers: How leading providers are leveraging software in a tough environment
Our research underscores four broad macro trends impacting how healthcare providers are thinking about software investments: financial pressures, labor shortages, cybersecurity risks, and HCIT vendor proliferation. While leading healthcare providers are responding to these challenges in various ways, our research suggests that many are deploying software solutions to mitigate the effects.
Financial pressures have long been the reality for providers. As costs rise, providers are doubling down on software that boosts revenue while reducing costs, leveraging digital front door solutions/ patient scheduling applications to increase volume while reducing back-office costs (e.g., schedulers, contact centers). Additionally, strong business analytics tools can rapidly identify inefficiencies and patient leakage. Finally, enhanced RCM modules can help maximize collections and optimize practice revenue — all while alleviating some of the labor intensity associated with revenue cycle processes.
Best-in-class providers are leveraging various software solutions to navigate challenges presented by labor shortages. Virtual care solutions, including telehealth and remote patient monitoring solutions, can enhance physician productivity while reducing data collection needs. Sophisticated scheduling solutions can help optimize staff allocations, alleviating pressure. Additionally, by effectively using RCM solutions, providers can further streamline medical coding, eligibility, billing, and collections to reduce administrative burdens.
Given the critical infrastructure and national security role played by healthcare and public health entities, regulators could introduce enhanced security mandates — and even provide funding to support cybersecurity for the US health system.
Security breaches and cyberattacks on US healthcare providers will likely continue to increase, especially considering rising geopolitical tensions. Given the critical infrastructure and national security role played by healthcare and public health entities, regulators could introduce enhanced security mandates — and even provide funding to support cybersecurity for the US health system. In the meantime, leading providers are taking a multilayered approach to cybersecurity systems, including Zero Trust systems, strong firewalls, frequent updating of antivirus software, and sophisticated data storage/backup solutions.
HCIT vendor proliferation pushes providers to seek IT solutions that can cover a full suite of tech needs to minimize pain from interoperability and EMR integration issues. As they evaluate new offerings, leading providers have strong processes in place for assessing business needs and the vendor landscape with an eye toward solution fit with existing core systems. Additionally, providers can partner with peer organizations to keep abreast of the market, with some large national health systems bolstering in-house development capabilities, including software incubators.
1.Software vendors: Meet customers where they are
Software players should ensure their GTM messaging is aligned with providers’ current challenges, emphasizing measurable financial and clinical ROIs of their products while underscoring differentiated security protocols and/or functionality. Additionally, they should consider bolt-on acquisitions to create sticky platform offerings.
With provider labor tightness showing no signs of abating, we expect labor dynamics will continue to spur many software investments.
Emphasize labor productivity and clinical ROI. Labor shortages were the primary incentive behind provider software investments over the past year. With provider labor tightness showing no signs of abating, we expect labor dynamics will continue to spur many software investments. Software vendors should emphasize the impact of their products on labor productivity and retention, especially for clinicians, as part of GTM approaches and post-sale.
Demonstrate financial ROI. With macroeconomic conditions pressuring profit margins, software players need to emphasize financial ROI in their GTM approaches. While messaging should be tailored to each individual customer, demonstrating ROI is critical in the current environment, especially with first-time customers. Proof points should be utilized, with tangible ways to measure the impact of proof of concept and implementations.
Highlight differentiated security features. With cyberattacks top of mind among providers, software vendors with cutting-edge security accreditations, features, and functionality can stand out.
Position solutions, and prioritize platforms. Provider software players can respond to competitive pressures and provider preferences for fewer vendors by positioning their offerings in defensible niches and building offerings that address a broader set of provider pain points, deepening customer relationships and improving stickiness. Savvy players can capitalize on the robust vendor environment via M&A activity, building or bolstering platform capabilities in the process. Additionally, incumbent software players can utilize strategic partnerships with provider organizations, software players, or other key stakeholders to bolster their existing offerings while minimizing financial risk.
2.Investors: Maintain discipline
HCIT has historically been an attractive investment area, outperforming other sectors during economic turbulence (see Figure 15). While there are unknowns about the current macroeconomic environment and how it will evolve, provider IT remains an attractive area for investment.
In the coming years, we believe provider investment priority areas will remain attractive hunting grounds for private equity investors. As credit markets eventually normalize to support deal activity, we believe that the present market could be ripe with add-on acquisition opportunities as the vendor landscape consolidates.
Figure 15: Healthcare IT investments have performed well throughout multiple business cycles
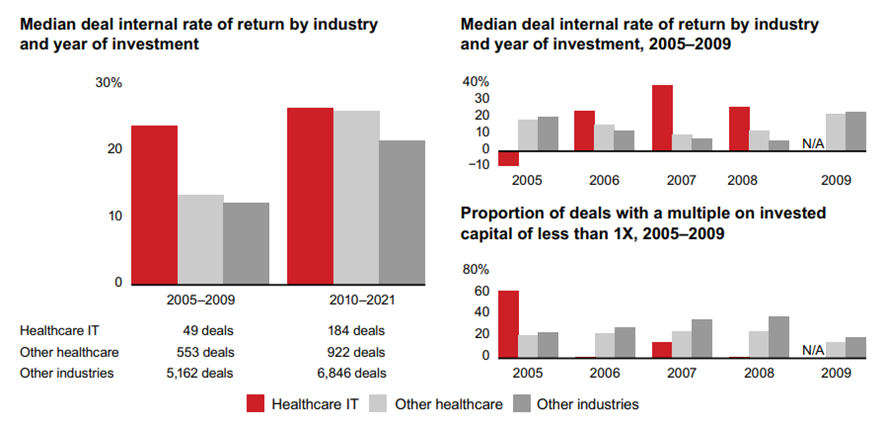
Notes: Median deal internal rate of return by industry and year of investment data set includes buyout and growth deals, fully and partially realized, all sizes, all sectors, all regions, years of investment 2005–2021, and all figures calculated in US dollars; proportion of deals with a multiple on invested capital of less than 1X data set includes buyout and growth deals, fully and partially realized, all sizes, all sectors, all regions; years of investment 2005–2009, and all figures calculated in US dollars
Source: DealEdge
In seeking out new investment opportunities, investors should be sure to perform their due diligence in assessing potential exposure to EMRs, encroachment from big tech, and disruptive innovators. Additionally, they should approach each investment category with an eye toward building a platform, and they should develop a thesis on natural adjacencies early on.
Existing asset owners can tailor GTM approaches to align with customer needs and should strive toward building sticky platform assets in niches that are better insulated against Epic and other forces that are encroaching on the space.












