This is a republication of the article “Value-based healthcare is a necessity — not a nice to have”, published by “NHG”, with the title above.
inHealthTransformation
institute for continuous health transformation
Joaquim Cardoso MSc
Founder and Chief Researcher & Advisor
December 28, 2022
SOURCE:
NHG EN — Nordig Health Care
December 16, 2022
NHG had the pleasure to participate in ICHOM’s 2022 conference in Boston.
This conference celebrated the 10th anniversary of ICHOM — the International Consortium for Health Outcomes Measurement — founded in 2012.
What a thrilling event with more than 500 healthcare leaders from 42 different countries discussing and sharing experiences about value-based healthcare and outcomes collection!
What were the key take-aways from the conference?
NHG’s team shares their key findings for you:
- 1.Healthcare is in crisis and value-based healthcare is a necessity, not a nice to have
- 2.Central coordination by payers is
- 3.Outcomes collection is still difficult — but there a are already a lot of successful examples on how to overcome these challenges
- 4.Patients could be an undervalued advocacy group for advancing value-based healthcare
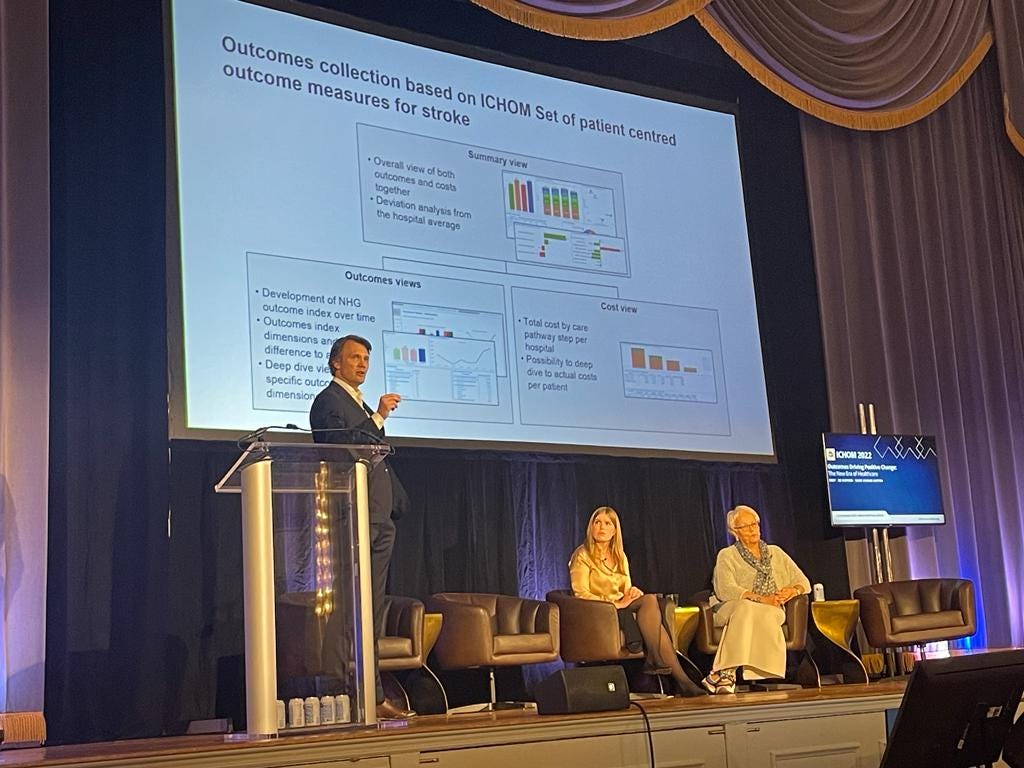
Vesa Komssi, Executive Vice President at NHG, held a presentation together with Tiina Sats, Head of Department at the Estonian Health Insurance Fund, and Terje Peetso, Member of the Board at the North Estonian Medical Centre, on a national stroke patient pathway pilot in Estonia.
In addition, Vesa co-chaired a roundtable discussion regarding implementation challenges and solutions.
There was a vast number of insights in the presentations and discussions. NHG’s team summarized some key findings we found especially inspiring and important.
1.Healthcare is in crisis and value-based healthcare is a necessity, not a nice to have
We are facing a unprecedent pressure towards the healthcare systems globally.
An aging population brings a whole new level of complexity in treating patients, the costs are increasing due to new more expensive treatments and there is a significant lack of healthcare professionals — to name just a few most pressing challenges in healthcare’s crisis.
So, what can a value-based approach bring to the table to solve this crisis?
If we do not understand the comparative value (i.e., outcomes that matter to patients vs. full care chain costs) of different treatment alternatives, providers, patient pathways, and healthcare systems, we are groping in the dark.
If we do not understand the value, it is impossible for us to systematically improve without sacrificing either outcomes that matter to patients or our cost effectiveness.
However, if we standardize outcomes measurement combined with collection of full care chain costs, …
… we are able to see where we create value and where we actually destroy value — i.e., what brings value and what does not, where should we focus in our improvement work, and who should we learn from.
Stefan Larsson, the Chairman of ICHOM, put it very well:
“Galileo Galilei was not a genius, he had a better telescope than anyone else.
If we could create that telescope for healthcare, that we measure outcomes in standardised manner, we will see things we have never seen before.
Unless we do that, we will keep doing wrong things over and over again and it is going to be more expensive”
We are constantly bombarded by new innovations, and it is impossible to truly know which ones would be beneficial for the specific situation.
However, as David Buchanan, Chief Clinical Officer at Oak Street Health, pointed out:
“If you have outcomes measurement in place, you can try out different innovations and see if they have value or not”.
Setting up outcomes measurement just for the purpose of evaluating a specific innovation is way too difficult and costly, but if you have continuous outcomes measurement in place, you can foster a culture of experimentation.
For example, in the Estonian stroke patient pathway pilot NHG created a dashboard that allows identification of specific intervention patient groups and, in real time, comparing their outcomes and full care chain costs with other intervention and control groups.
For example, in the Estonian stroke patient pathway pilot NHG created a dashboard that allows identification of specific intervention patient groups and, in real time, comparing their outcomes and full care chain costs with other intervention and control groups.
Pieter de Bey, Managing Director of Santeon, raised an important question in one of the panel discussions:
“Could you require the same from tech companies and pharma companies [as from healthcare providers], to be transparent about the outcomes they deliver?”
One key aspect of the healthcare crisis is shortage in professionals.
There are many underlying reasons for this, but one reason is that healthcare has lost its purpose.
The focus is way too often in outputs, budgets, and rush, and way too little on what outcomes we are able to deliver to patients.
One key aspect of the healthcare crisis is shortage in professionals.
There are many underlying reasons for this, but one reason is that healthcare has lost its purpose.
The focus is way too often in outputs, budgets, and rush, and way too little on what outcomes we are able to deliver to patients.
Elizabeth Teisberg, Co-author of Redefining Healthcare put it well:
“We need to return healthcare to its purpose of health.”
We need to change our focus towards those outcomes that matter to patients.

2.Central coordination by payers is vital for the value-based healthcare to truly take off
Implementing outcomes measurement is not easy, and it is especially difficult if you do it alone.
Healthcare systems are typically organized around payers, either public or private.
Payers have a critical role in enabling the implementation of outcomes measurement and, typically, have access to full care chain costs.
There is no point that each healthcare provider selects their own set of outcome measures and builds infrastructure for outcomes and costs collection.
There is no point that each healthcare provider selects their own set of outcome measures and builds infrastructure for outcomes and costs collection.
Payers are best positioned to coordinate decisions on which measures to use across providers and join forces to build outcomes collection and visualization infrastructure.
In the conference, we heard good examples from Estonia, Singapore and US where payers have taken leading role in defining outcomes measures and building outcomes collection and visualization infrastructure.
Central coordination also directs the process and enables implementations to start simultaneously for providers within same therapeutical area.
This makes it possible to later benchmark results and share learnings and best practices between providers.
Payers and/or government level central coordination are especially needed for determining:
(a) which measures to use,
(b) outcomes collection and visualization infrastructure, and
(c) funding for the implementation.
Payer involvement typically leads to commitment among all stakeholders and, therefore, also chances of success are higher.

3.Outcomes collection is still difficult — but there a are already a lot of successful examples of how to overcome these challenges
There are many challenges associated with outcomes collection.
Clinical outcomes are in general easier to collect than patient-reported outcomes, PROM’s, but some of the clinical measures might also be scattered in many places in the electronic medical record, EMR.
PROM collection is seen as more difficult as the questionnaires are often lengthy and seldom integrated into the EMR and the results are not systematically used in patient work.
Also, patients may have several parallel treatment processes ongoing which creates conflicts in answering and interpreting the PROM results.
Choosing the right PROM questionnaire is also a challenge and there is a lack of disease specific and sensitive PROM questionnaires.
Possible solutions include the use of computer adapted testing and use platforms that integrate with EMR.
Physicians’ and nurses’ involvement early on is also critical if you want to succeed with the collection and imbed it into the treatment process.
As starting the VBHC journey can be a daunting experience, it is best to get going in simple and clearly defined procedures.
Typically, secondary care patient segments are easier that chronic conditions, primary care, or social care where problems are in many cases very complex and the causality harder to define.
It is important that first implementations are successful and, hence, it makes sense to start where chances of success are higher.
Another way to start out in a simple way, is collecting overall quality of life measures and starting to use that information in daily clinical practice.
“This is not rocket science — we are only asking patients how they are doing,” said Matthias Rose, Medical Director at Charite Berlin.

4.Patients could be an undervalued advocacy group for advancing value-based healthcare
The whole purpose of healthcare is to improve the health of patients, and patients should have a say in what brings value to them and how value-based healthcare should be promoted and most importantly why.
For example, Movember sponsored the very first ICHOM standard set and has been since then a key advocate for advancement of prostate cancer outcomes collection.
Could other global and national patient organizations follow their example?
Patients have the power to impact politicians who in turn can demand central coordination, secure funding, set goals and require the collection of outcomes.
For this, VBHC theory needs to be translated into real life patient stories and combined with design thinking.
…VBHC theory needs to be translated into real life patient stories and combined with design thinking.
Empowering patients and shared decision making have been discussed for a long time, but only measuring patient outcomes makes shared decisions really possible.
When combining outcomes measurement with AI, shared decision-making truly comes to live.
However, a sufficient amount of clinical and PROM data is needed as optimal treatment decisions cannot be reached without abundance of outcomes data.

All in all, the message from the conference was loud and clear: standardised outcomes measurement can provide the acutely needed keys for solving the healthcare crisis.
All we need is to take those learnings from earlier implementations, start measuring outcomes in standardised manner and use outcomes from every patient interaction to management meetings and research & development!
All we need is to take those learnings from earlier implementations, start measuring outcomes in standardised manner and use outcomes from every patient interaction to management meetings and research & development!
Originally published at https://nhg.fi on December 16, 2022.
ICHOM is a non-profit organization setting standards for outcome measurement. Celebrating the 10 th anniversary conference is a significant milestone for an organization that has advanced the worldwide standardization of outcome measurement probably more than any other governmental or non-governmental body in the world.
Nordic Healthcare Group (NHG) is a certified ICHOM Implementation Partner, and our team participated in the conference together with our clients and partners from e.g. Finland, Estonia, Zimbabwe, US, Bulgaria and the Netherlands.
Names mentioned
Vesa Komssi, Executive Vice President at NHG, held a presentation together with
Tiina Sats, Head of Department at the Estonian Health Insurance Fund, and
Terje Peetso, Member of the Board at the North Estonian Medical Centre, on a national stroke patient pathway pilot in Estonia. In addition, Vesa co-chaired a roundtable discussion regarding implementation challenges and solutions.
Stefan Larsson, the Chairman of ICHOM
David Buchanan, Chief Clinical Officer at Oak Street Health
Pieter de Bey, Managing Director of Santeon
Matthias Rose, Medical Director at Charite Berlin.

Note from the Editor of this site (Joaquim Cardoso)
From the summary above, we listed the following tools to expand the VBHC toolbox:
- central coordination by payers
- Outcomes measures definition by payers
- outcomes measurement standardization
- outcomes collection & visualization infrastructure (by payers)
- full care chain costs measurement (by payers)
- funding for the implementation of VBHC (by payers)
- PROMS computer adapted testing and platforms integrated with EMR
- Combining outcomes measurement with AI for shared decision making
- Clinical Outcomes collection in the EMR
We also made a note about VBHC enablers:
- Stakeholders commitment
- Shared decision making
And also a selection of some VBHC barriers:
- PROMs collection
- PROMs not integrated into the EMR











