Investments in information systems and on education of key stakeholders are key to foster VBHC implementation in the region.
This is a republication of an excerpt version of the paper below, with the title above.
Value-based healthcare in Latin America: a survey of 70 healthcare provider organisations from Argentina, Brazil, Chile, Colombia and Mexico
BMJ Open
Marcia Makdisse ,1,2 Pedro Ramos,1,3 Daniel Malheiro,1 Marcelo Katz,1 Luisa Novoa,1 Miguel Cendoroglo Neto,1 Jose Henrique Germann Ferreira,1 Sidney Klajner 1
04 May 2022
One page summary by:
Joaquim Cardoso MSc.
Health Transformation Institute(HTI)
Value Based Health Care Unit
July 7, 2022, nchc
Objectives
- Value-based healthcare (VBHC) is a health system reform gradually being implemented in health systems worldwide.
- A previous national-level survey has shown that Latin American countries were in the early stages of alignment with VBHC.
- Data at the healthcare provider organisations (HPOs) level are lacking.
- This study aim was to investigate how HPOs in five Latin American countries are implementing VBHC.
Design
- Mixed-methods research was conducted using online questionnaire, semistructured interviews based on selected elements of the value agenda (from December 2018 to June 2020), analyses of aggregated data and documents.
- Qualitative analysis was performed using NVivo QSR International, 1.6.1 (4830).
- Quantitative analysis used Fisher’s exact test.
- Univariate analysis was used to compare organisations in relation to the implementation of VBHC initiatives. A p≤0.05 was considered significant.
Participants
- Top and middle-level executives from 70 HPOs from Argentina, Brazil, Chile, Colombia and Mexico.
Results
- The definition of VBHC varied across participating organisations. Although the value equation had been cited by 24% of participants, its composition differed in most case from the original Equation.
- Most VBHC initiatives were related to:
– care delivery organisation (56.9%) and
– outcomes measurement (22.4%) …
- … but in most cases, integrated practice unit features had not been fully developed and outcome data was not used to guide improvement.
- Information, stakeholders buy-in, compensation and fragmented care delivery were the most cited challenges to VBHC implementation.
- Fee-for-service predominated, although one-third of organisations were experimenting with alternative payment models.
Conclusions
- A wide variation in the definition and level of VBHC implementation existed across organisations.
- Our finding suggests investments in information systems and on education of key stakeholders will be key to foster VBHC implementation in the region.
- Further research is needed to identify successful implementation cases that may serve as regional benchmark for other Latin American organisations advancing with VBHC.
Key indicator (by the editor of the site) :
- Fee For Service (FFS) was the predominant payment modality in 91% of HPOs with 54% of them being reimbursed solely based on the FFS model, mostly private hospitals, and the remaining by means of global budgets, all public hospitals.
Selected images:
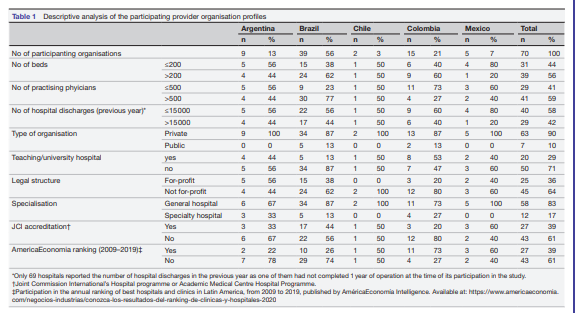
Table 1 Descriptive analysis of the participating provider organisation profiles
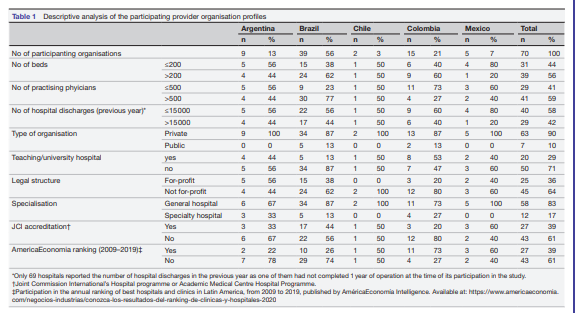
Figure 1 — The meaning of value-based healthcare for participating healthcare provider organisations.
The figure displays the distribution of codes by number and percentage of coding references derived from the qualitative analysis.
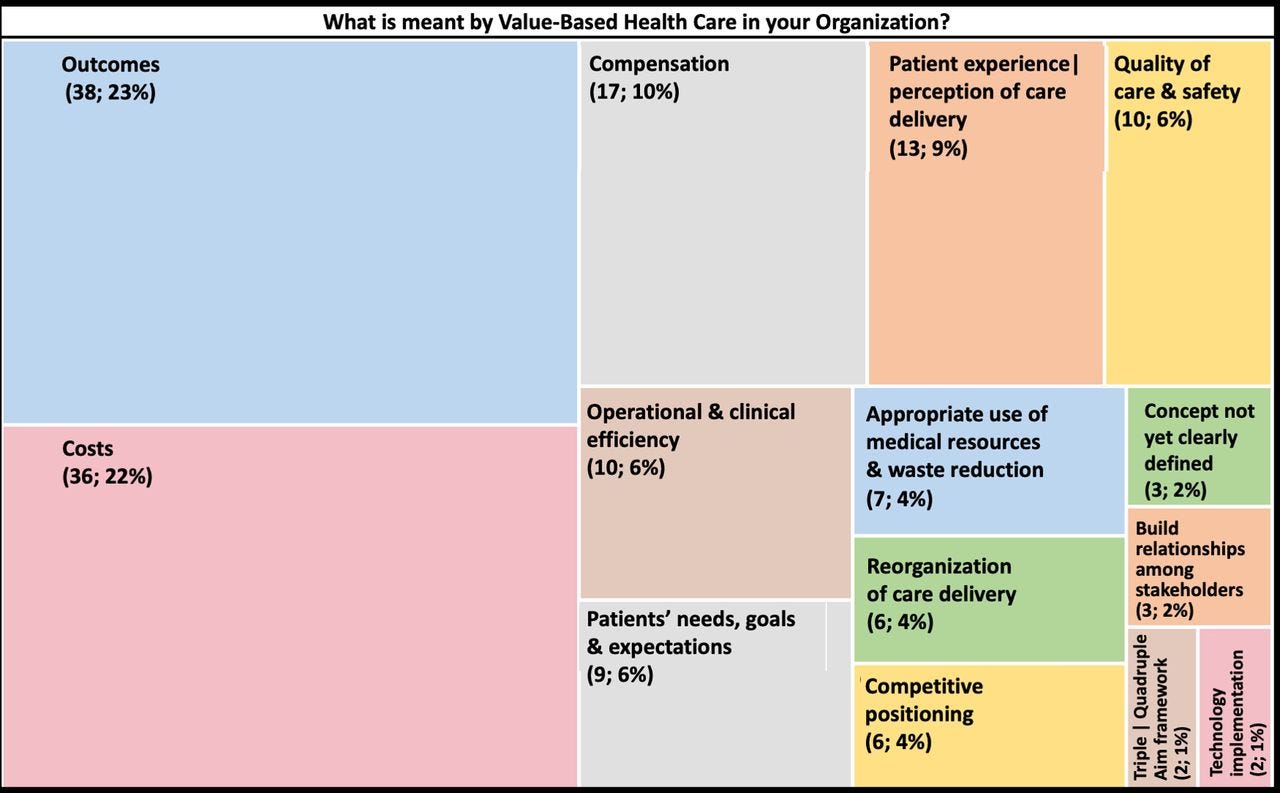
Table 2 — Implementation of the core elements of the value agenda among participants
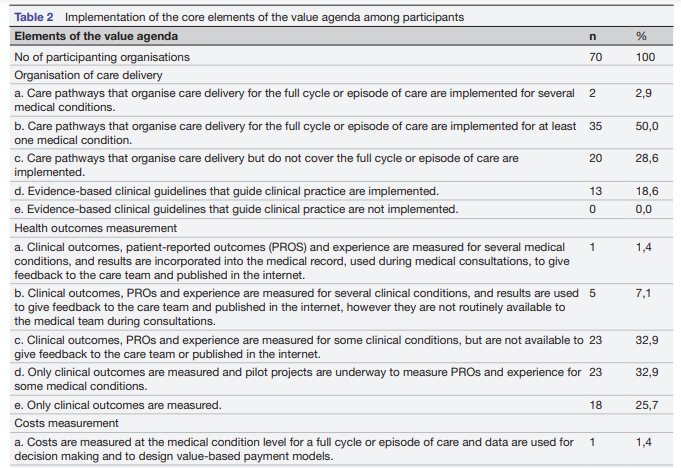
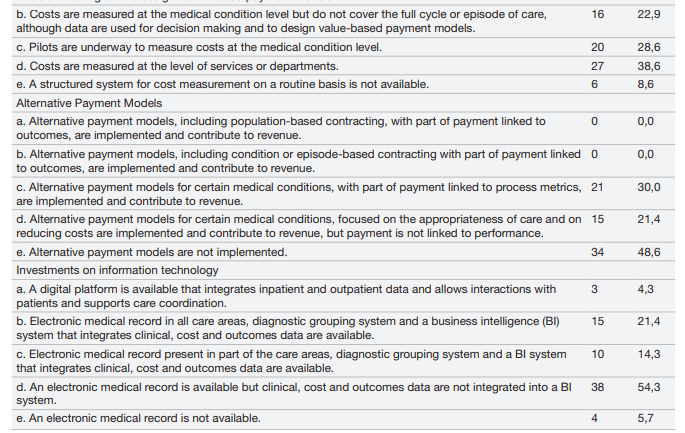
Figure 2 — Initiatives alignment with the integrated practice unit (IPU) features.
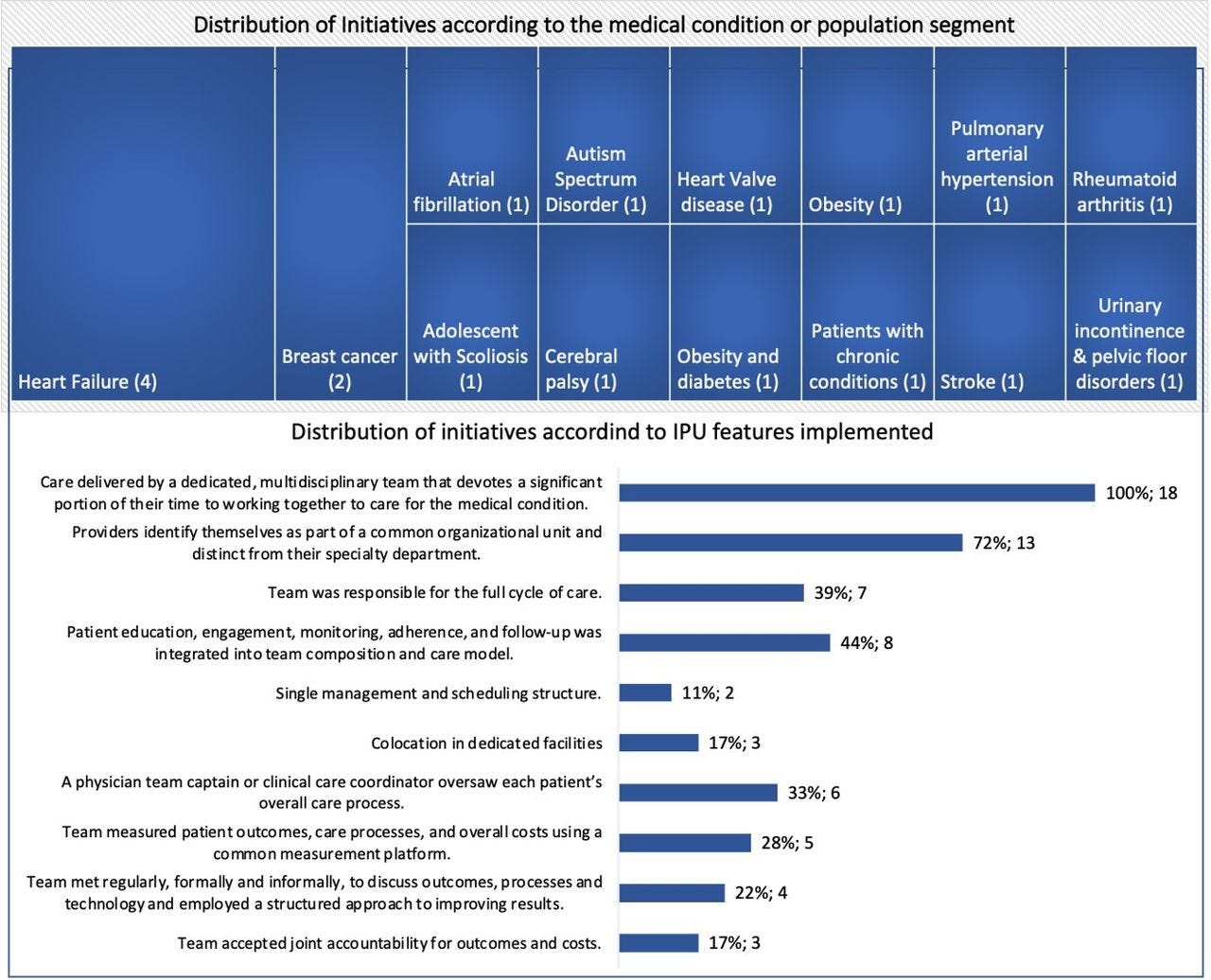
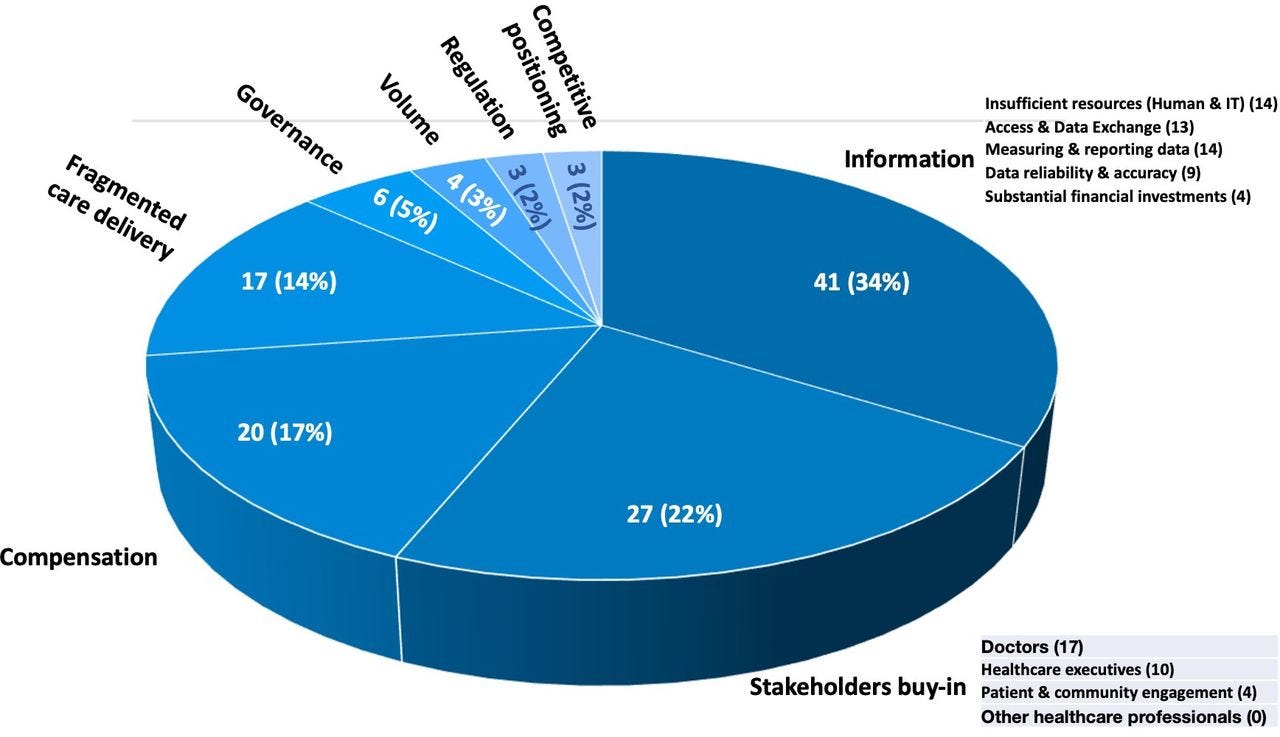
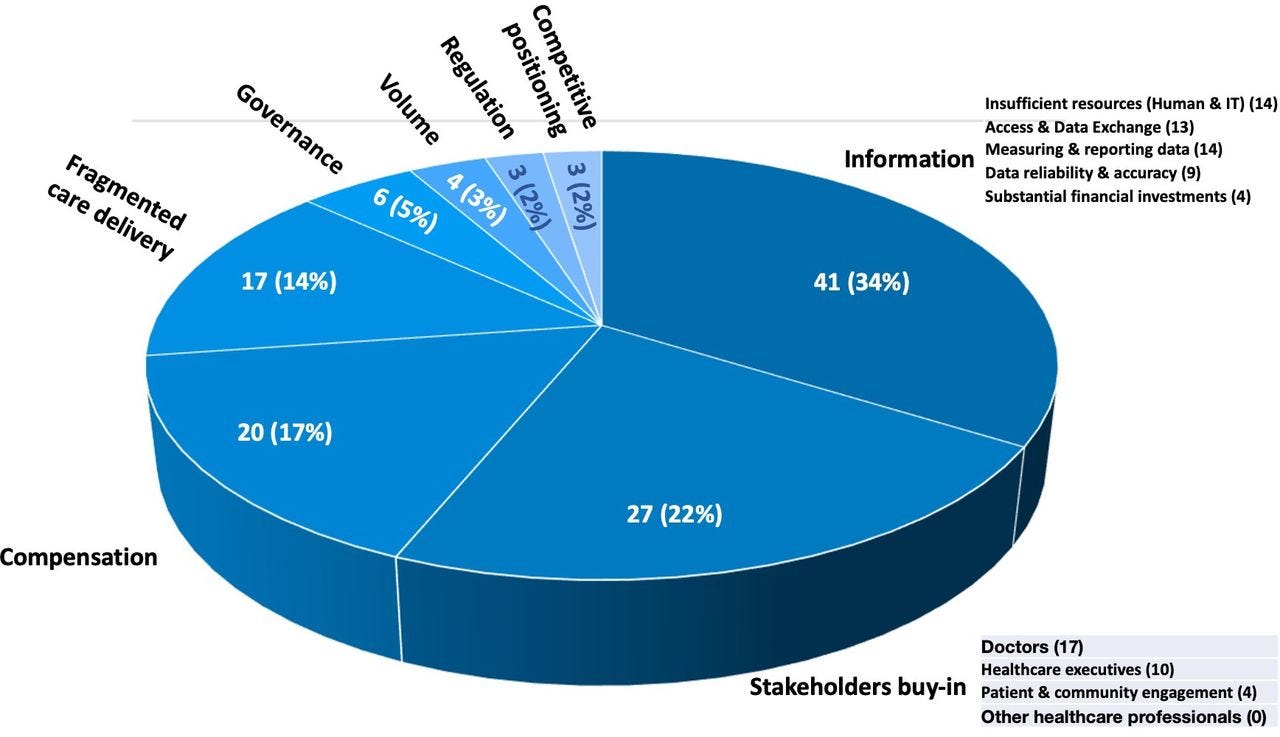
Figure 3 — Challenges for a healthcare provider organisation to implement value-based healthcare. IT, information technology.
ORIGINAL PUBLICATION (excerpt of the full version)

Value-based healthcare in Latin America: a survey of 70 healthcare provider organisations from Argentina, Brazil, Chile, Colombia and Mexico
BMJ Open
Marcia Makdisse ,1,2 Pedro Ramos,1,3 Daniel Malheiro,1 Marcelo Katz,1 Luisa Novoa,1 Miguel Cendoroglo Neto,1 Jose Henrique Germann Ferreira,1 Sidney Klajner 1
04 May 2022
Introduction
Escalating costs and substantial variation in the quality of health services threatens the sustainability of health systems globally.
In several countries, a double-digit difference between general inflation and medical inflation has been reported,1along with an evident failure of healthcare systems to address preventable diseases and to warrant universal and equitable access to care. Such challenges are even bigger for Latin American countries where increasing rates of chronic non-communicable diseases are combined with endemic and emerging diseases and, despite the positive effects of a series of health system reforms implemented in the last three decades, great disparities remain in terms of access to effective health services.2
The value-based healthcare (VBHC) approach, proposed by Porter and Teisberg, has been seen as a strategy to transform the healthcare system through a redesign of the care-delivery processes around medical conditions or population segments, monitoring of outcomes and costs and a change in the financing model from paying for each service provided (fee-for-service (FFS)) to paying for outcomes achieved (fee-for-value).3
The value-based healthcare (VBHC) approach, proposed by Porter and Teisberg, has been seen as a strategy to transform the healthcare system through …
… a redesign of the care-delivery processes around medical conditions or population segments, monitoring of outcomes and costs and a change in the financing model from paying for each service provided
This theory has been expressed in the value equation, where value is defined as health outcomes relative to the cost, and in the value agenda composed of six elements (organise into integrated practice units (IPUs), measure outcomes and costs for every patient, move to bundled payments for care cycles, integrate care across separate facilities, expand excellent services across geography and build an enabling information technology platform).4
Most reports on the VBHC adoption come from Europe and North America 5 6 and little is known about its implementation in Latin America.
A report published in 2016, by The economist intelligence unit (EIU), assessed the alignment with VBHC components in 25 countries, including Brazil, Colombia, Chile and Mexico.
Assessment was organised around four domains (Enabling context, policies and institutions for value in healthcare; Measuring outcomes and costs; Integrated and patient-focused care and Outcome-based payment) and 17 qualitative indicators.
Results showed considerable variations in the adoption of such domains across countries.
Sweden was the only country with a very high alignment and about half of participating countries emerged as having low alignment with VBHC, including Latin American countries, except for Colombia, which was considered to have a moderate alignment as a result of the healthcare reforms aimed at achieving universal coverage, redirecting care delivery around patient needs and monitoring of costs for high-cost conditions.
Chile scored second due to the implementation of a bundle payment system in several areas and monitoring of treatment costs by major payers.
Brazil and Mexico had the lowest scores, and Brazil was the only country in the region not to have a condition-based national registry 7.
Brazil and Mexico had the lowest scores, and Brazil was the only country in the region not to have a condition-based national registry 7.
The EIU study, however, focused on the macrolevel evaluation of health systems.
More recent reports from leading Latin American healthcare organisations have shown an emerging movement around the implementation of alternatives to FFS payments, more integrated care models, monitoring of outcomes and costs using the International Consortium for Health Outcomes Measurement (ICHOM) standard sets and time-driven activity-based costing (TDABC).8–11
These experiences by front-runner organisations may serve as a benchmark for other organisations in the region initiating similar endeavours.
Therefore, the aim of this study was to investigate how healthcare provider organisations (HPOs) from the five biggest Latin American economies were advancing with VBHC implementation in their local contexts.
Methods
See the original publication
Results (excerpt)
Participants
A total of 70 HPO representatives completed the online survey. Of those, 58 (83%) also participated in a virtual interview to deepen the information provided in the questionnaire.
Table 1 presents a descriptive analysis of the organisation profiles.
Table 1
The meaning of VBHC
Figure 1 presents the distribution of the 14 codes compared by number and percentage of the 163 coding references derived from the qualitative analysis performed with NVivo on the meaning of VBHC given by each organisation during the interviews.
Figure 1 — The meaning of value-based healthcare for participating healthcare provider organisations.
The figure displays the distribution of codes by number and percentage of coding references derived from the qualitative analysis.
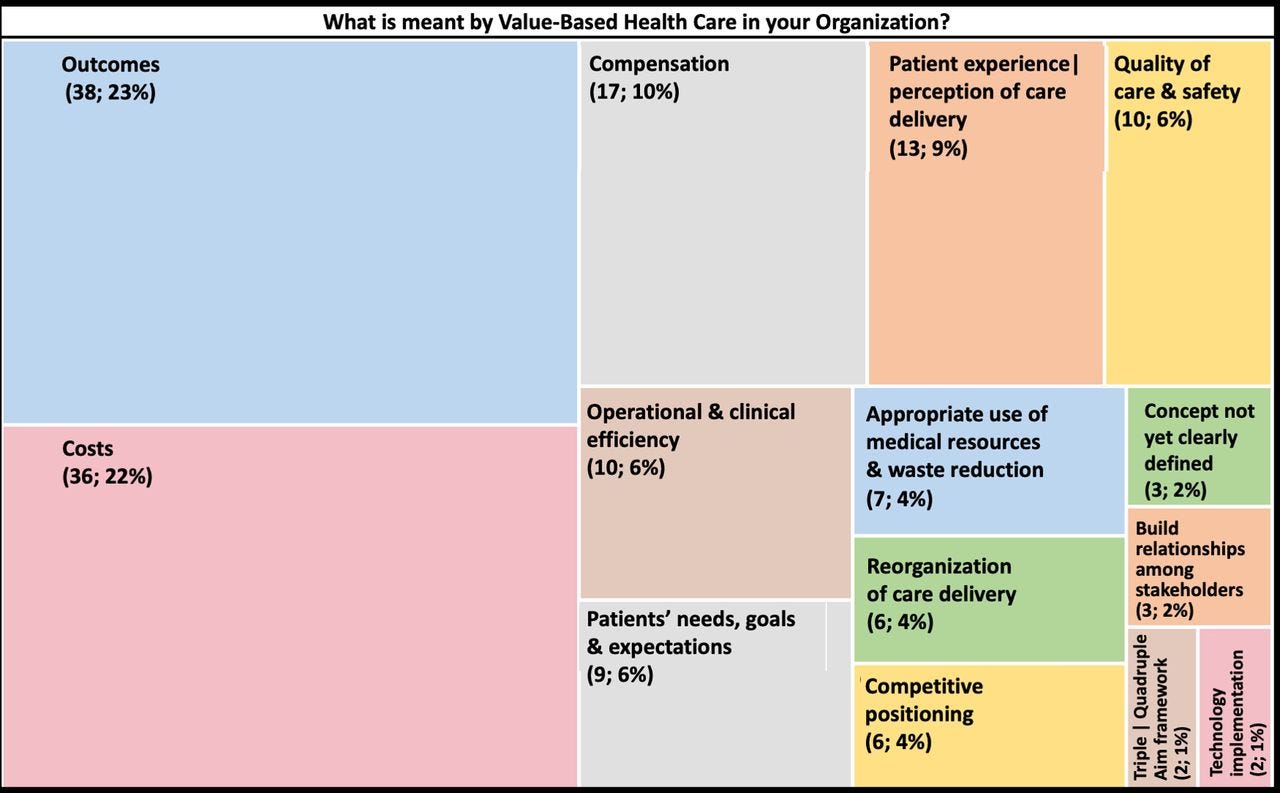
Outcomes and cost were the codes with the highest number of references, followed by compensation and patient experience or perception of care.
Examples of references, selected for the 14 different codes, is presented in online appendix E.
The value equation was mentioned by 14 participants (24%), although only 5 mentioned ‘outcomes/costs’ as its components.
The remaining defined the value equation as ‘value/cost’, ‘best medicine/cost’, ‘individual value/cost’, ‘best care possible/cost’, ‘outcomes or patient experience/cost’, ‘quality of care perceived by the patient/cost’, ‘quality/cost’ and ‘outcomes/price’.
Implementation of the elements of the value agenda
The level of adoption of the value agenda elements are described in table 2 .
In regard to care delivery organisation, half of participants informed care delivery was organised around medical conditions for full care cycles for at least one medical condition, although less than 3% informed this was the case for several medical conditions.
Table 2
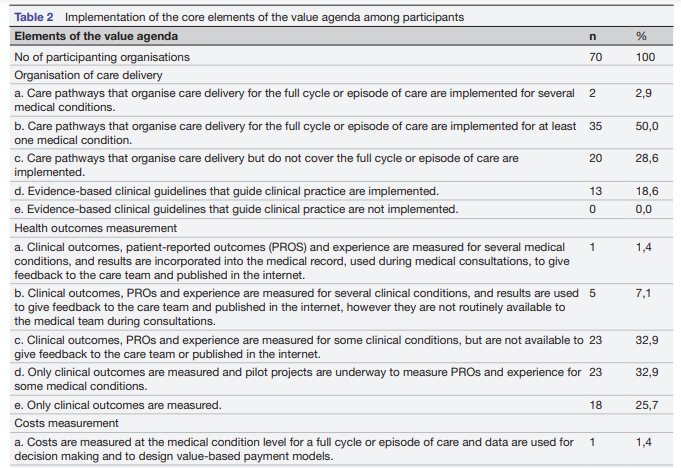
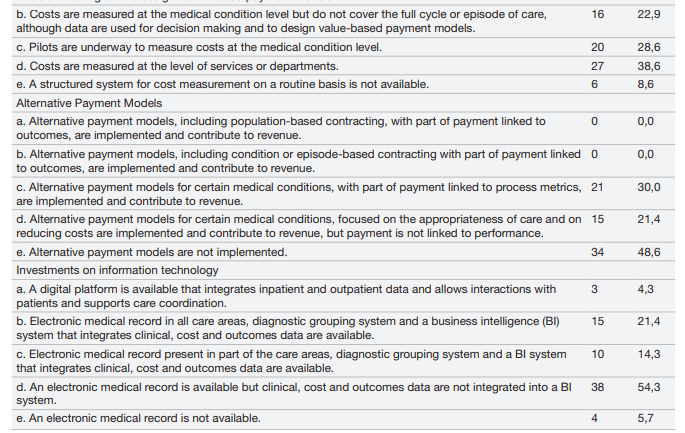
All organisations referred to measure clinician-reported outcomes, most frequently mortality and complications rates.
Patient-reported outcome measures (PROMs) were measured by 41.4% but in only 8.5% this information was used to give feedback to the care team, or in routine medical encounters with patients, or published on the internet.
In 10 Brazilian organisations, which corresponds to 25.6% of participants from that country, PROMs were collected using ICHOM standard sets for heart failure, stroke and hip and knee osteoarthritis as part of a collaborative started in 2017 by the National Association of Private Hospitals.
In regard to cost measurement, 24.3% of organisations informed to measure cost at the medical condition level but only two (2.9%) measured costs of full care cycles.
Most of them measured costs only at the service or department level (67.2%), although 28.7% referred that pilots were underway to measure costs at the condition level.
Six (8.6%) participants did not have a cost system structure in place to measure costs on a routine basis.
Only one organisation was using the TDABC methodology, as part of a public-private partnership with the Ministry of Health focused on training a critical mass of healthcare professionals to measure TDABC and on coordinating multicentre TDABC initiatives in public hospitals.
None of the organisations had a payment model in place where payment was linked to outcome-based performance metrics, although 5 (7%) referred participation in contracts where HPOs bore the costs of treatment-related complications.
Thirty per cent reported to participate in pay-for-performance agreements based on process metrics and 21.4% referred agreements focused on improving the appropriateness of care and on cost reduction.
The remaining were not participating in alternative payment modalities.
FFS was the predominant payment model (91.4%) while global payment was present as the only modality in six public hospitals.
Among organisations on FFS, 54.3% were on FFS only while the remainder (37.1%) were already experimenting a combination of FFS with other alternative payment models such as global payments (capitation and/or global budgets), bundled payments (defined as condition or episodic bundles that covered treatment-related complications for a predefined period of time) or pay-for-performance agreements.
Additionally, three (4.3%) organisations referred to participate in risk-sharing agreements with payers and/or the medical device industry.
Regarding the information technologies (IT) available,
- around 94% of organisations had an electronic medical record, but
- only 40% had a business intelligence system to integrate clinical, cost and outcomes data and
- 4% had implemented an interoperable digital platform that integrated both inpatient and outpatient data and allowed interactions between patient and care team.
Implementation of a VMO
Thirty-one participants (44%) informed to have implemented a VMO.
In the interviews, however, when asked to describe the VMO in terms of the definition proposed by Kaplan et al as a ‘central office to oversee the creation of capabilities and information to implement VBHC initiatives such as outcomes and cost measurement and management, set priorities for continuous improvement projects, facilitate the creation of value-based payment models and ensure that new IT platforms are aligned with the value agenda’, only 12 (17%) were aligned with this definition, although they differed in terms of size, governance and structure.13
Thirty-one participants (44%) informed to have implemented a VMO.
In the interviews, however, when asked to describe the VMO in terms of the definition proposed by Kaplan et al … only 12 (17%) were aligned with this definition, although they differed in terms of size, governance and structure.13
In the remaining, the structure was dedicated to
- patient quality and safety (47%),
- were decentralised corporate areas that collaborated in specific projects (21%),
- innovation (11%),
- patient experience (11%) and
- project management or continuous process improvement (11%).
Implementation of VBHC initiatives
In total, 57 (81.4%) organisations referred 179 initiatives that they considered aligned with the VBHC.
Seven initiatives (3.9%), referred by two organisations were excluded because they had not been implemented, leaving a total of 172 initiatives from 55 organisations to be analysed.
Overall, only one-third of initiatives (n=58) were aligned with VBHC and were related to organisation of care delivery (n=33, 56.9%), outcomes measurement (n=13, 22.4%), cost measurement (n=6, 10.3%) and bundled payments (n=6, 10.3%).
nitiatives not aligned with those elements were categorised as ‘other initiatives’ and were related to quality and safety, operational efficiency and process improvement, alternative payment models other than bundles, patient experience, investment in new technologies, physician relationship programmes, research projects and marketing, among others.
A flow diagram of initiatives and their distribution according to their alignment with VBHC is presented in the radar charts ( online appendix F).
Most participants implemented VBHC initiatives related to organisation of care delivery (n=24, 72.7%), followed by outcomes measurement (n=13, 39.4%), cost measurement (n=6, 18.2%) and bundled payments (n=6, 18.2%). The full list of initiatives can be found in online appendix G.
A univariate analysis was used to assess the factors related to the implementation of VBHC initiatives ( online supplemental appendix H).
Regarding organisation profiles, specialty hospitals were associated with implementation of VBHC initiatives (p=0.05), while all other organisation characteristics such as being public/private, teaching/non-teaching, for-profit/not for-profit, number of beds, JCI accreditation or participation in the ranking of best hospitals were not related to VBHC implementation.
Organisations that referred high level of alignment with organisation of care delivery and outcomes measurement, in the online survey, were associated with the implementation of VBHC initiatives (p<0.01 and 0.01, respectively). Adoption of ICHOM’s standard sets (p<0.01) and implementation of alternative payment models (p=0.010) were also significantly associated with VBHC implementation.
Figure 2 presents the distribution of the initiatives categorised as ‘organisation of care delivery’ according to the medical condition or population segment and to IPU features implemented.
Figure 2 — Initiatives alignment with the integrated practice unit (IPU) features.
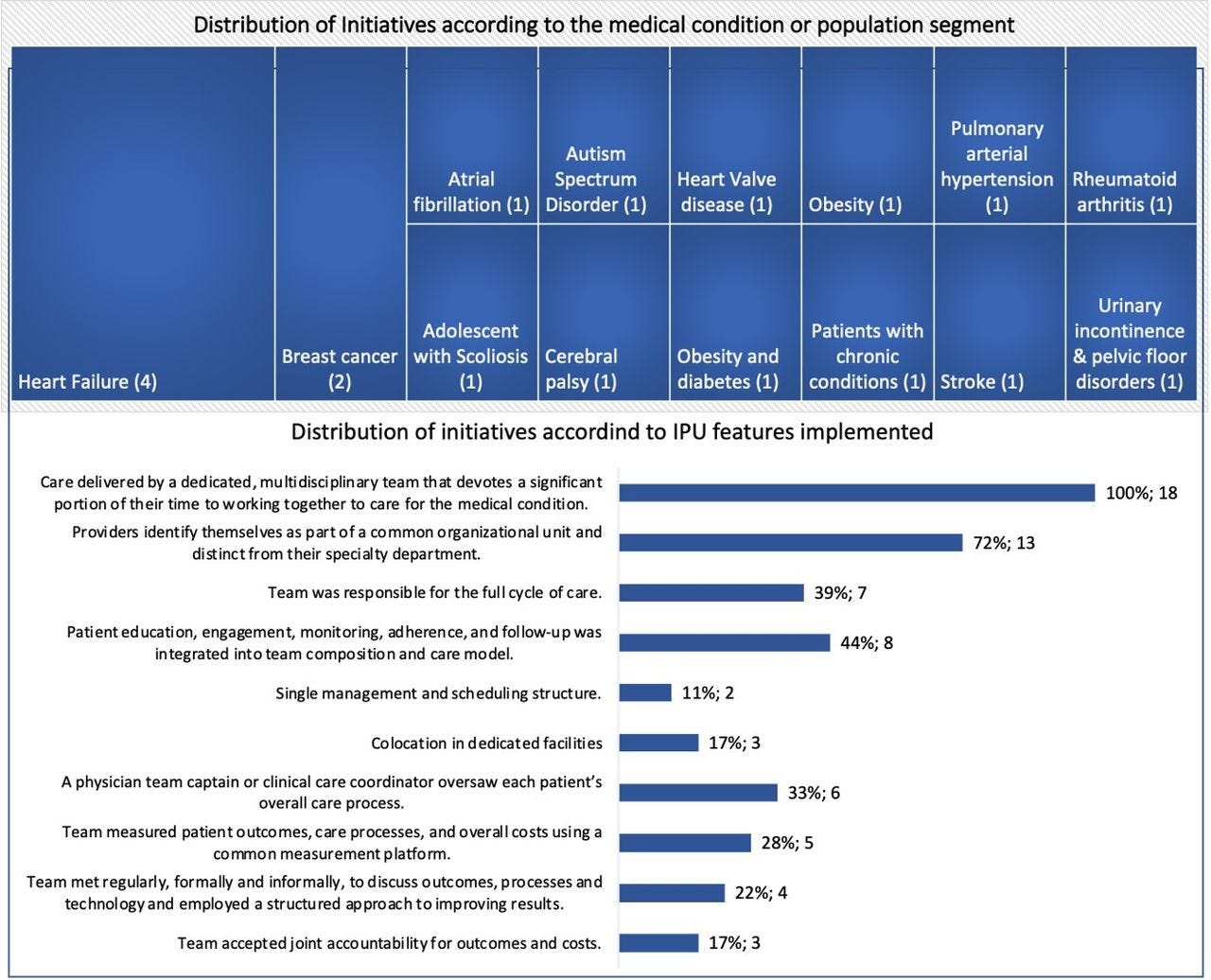
Eighteen initiatives were identified in which care was organised around 14 medical conditions or patient segments and delivered by a multidisciplinary team, although only 39% covered the full cycle of care of that condition.
Heart failure and breast cancer were the most prevalent conditions. None of the initiatives had fully developed all IPU features.
Challenges to VBHC implementation
Figure 3 presents the challenges to VBHC implementation shared during the interviews.
Most references were related to
- the unavailability of meaningful and actionable information (34%), followed by
- stakeholders buy-in (22%) and
- compensation (17%).
Examples of references, selected for the eight different codes, are presented in online appendix I.
Figure 3 — Challenges for a healthcare provider organisation to implement value-based healthcare. IT, information technology.
Discussion
To the best of our knowledge, this study is the first to assess how HPOs from Latin American countries are implementing VBHC strategies.
It differs from a previous study that assessed VBHC implementation in 25 countries, 4 Latin American countries among them, which focused on the macrolevel evaluation of health systems.7
Another difference is that Argentina was included in our study due to its relevance to the region, as Latin America’s third-largest economy.
Our findings show a wide variation in how VBHC is defined and on the level of implementation of VBHC initiatives across HPOs.
Although ‘outcomes’ and ‘costs’ were the referenced codes, it represented less that one-quarter of total references and, in most cases, when the value equation was mentioned, most respondents used less specific terms such as ‘value’ or ‘quality’ instead of ‘outcomes’, which makes the concept less tangible.
The same happened when participants were asked to inform VBHC initiatives implemented and two third of initiatives mentioned were not aligned with VBHC.
This finding suggests there is an awareness on VBHC in the region but that there is a gap in relation to its core concepts.
This is in accordance with previous studies that reported a dilution instead of a diffusion of the original concepts of the VBHC strategy.
This highlights the need to educate different stakeholders on VBHC in order to advance with its implementation.14 15
… there is an awareness on VBHC in the region but that there is a gap in relation to its core concepts.
Most initiatives were directed at reorganising care delivery and outcomes measurement but when the IPU features were assessed, most features had not been fully implemented specially in terms of:
- taking responsibility for full cycles of care,
- having a team captain/care coordinator,
- measuring outcomes and costs,
- assuming responsibilities for the results and
- meeting regularly to promote continuous improvements.
Although there is a clear effort underway in over 40% of HPOs to collect PROMs using ICHOM standard sets, such information has not been integrated so far into routine clinical practice or used to improve quality and outcomes, in most organisations, thus limiting their potential for enhancing value in care.16 17
Reorganisation of care delivery and outcomes measurement are key steps to start VBHC implementation in line with recommendations given by Elizabeth Teisberg, cocreator of the VBHC Strategy, based on data collected over more than a decade of research in organisations that achieved better health outcomes, that VBHC implementation begins with identifying unmet needs of patient segments and with designing solutions that meet those needs.18
Information, stakeholders buy-in, compensation and fragmented care delivery were the most cited challenges during the interviews.
Information plays a key role in VBHC implementation, and the lack of an interoperable information and communication technology (ICT) platform may function as a barrier to implement, and even more, to scale-up initiatives and transition into outcome-based agreements as ITC reinforces all other elements of the value agenda.4
Doctors and executives were the most referenced stakeholders in terms of the buy-in process.
Doctors as ‘team captains’ have a key role in IPU implementation and as a member of the multidisciplinary care team,19and quoting one of the interviewees (I_26) ‘ currently doctors are not educated on this and whoever is leading these processes of change is not involving physicians in such discussions.’
Information, stakeholders buy-in, compensation and fragmented care delivery were the most cited challenges during the interviews.
In regard to compensation, FFS was the predominant payment modality in 91% of HPOs with 54% of them being reimbursed solely based on the FFS model, mostly private hospitals, and the remaining by means of global budgets, all public hospitals.
Those two payment modalities do not incentivise care coordination and do not hold HPOs accountable for healthcare outcomes.20Studies have shown that the greater the fragmentation of care, the greater the unnecessary use of resources and the worse the quality and outcomes of care, contributing to enhancing healthcare costs.21Although 37% of organisations were participating in alternative payment models, none of those payment agreements linked payment to performance based on outcome metrics, which define value-based payment models.22
…FFS was the predominant payment modality in 91% of HPOs with 54% of them being reimbursed solely based on the FFS model, mostly private hospitals, and the remaining by means of global budgets, all public hospitals.
When HPOs were compared in terms of implementation of VBHC initiatives, specialisation, a high level of alignment with organisation of care delivery and outcomes measurement, implementation of ICHOM standard sets and participation in alternative payment agreements were associated with implementation of VBHC initiatives.
Among the 12 specialty hospitals participating in the study, 9 had implemented VBHC initiatives (75%, p=0.05).
This finding suggests that it may be simpler for specialty hospitals to adopt VBHC strategies aligned with the Value Agenda.
This is not surprising considering that, at its core, VBHC is a specialisation-oriented management framework, and most success cases have been reported in well defined, narrow ‘focused factories’.23
Further research may address the potential adaptations needed for VBHC adoption to thrive in general hospitals, including in large, academic medical centres.
Strengths and weaknesses of the study
There is a paucity of data regarding VBHC implementation in Latin America. Therefore, the strength of this study is to bring new evidence on VBHC implementation from the perspective of leading HPOs in the region. It is a contribution to improve the understanding of how healthcare transformation is taking place in Latin America, in terms of the value agenda strategies that organisations have focused their efforts on and which initiatives have been implemented providing insights for future studies, follow-up and action.
A limitation of this research was the small number of participants for two of the selected countries. Chile and Mexico had a low acceptance response with only two and five participants, respectively. This fact did not allow us to make any meaningful comparison among participating countries. On the other hand, we believe that the aggregate information presented in our study is relevant as a starting point for discussions around the role of HPOs in care transformation. Additionally, we are not aware of any other study gathering data from 70 different HPOs from the region.
Another limitation is the predominance of private hospitals, which comprised 90% of participants. Although findings cannot be extrapolated to public organisations, leading public HPOs are represented in the study.
Conclusions
VBHC implementation is challenging particularly in Latin American countries where access to care is still a major issue.
A wide variation in the definition and level of VBHC implementation existed across organisations.
Information, stakeholders buy-in, compensation and fragmented care delivery were the most cited challenges.
Nonetheless, some organisations are advancing in terms of implementing VBHC initiatives, mostly focused on the organisation of care delivery and outcomes measurement, that may provide insights for other HPOs in the region.
Scalability of such initiatives will demand investments on education of different stakeholders and on systematic measurement and use of outcomes and cost data, which in turn demand more investments on ICT.
Further research is needed to identify successful implementation cases that may serve as regional benchmark for the other Latin American HPOs advancing with VBHC.
Acknowledgments
We thank all healthcare provider organisations and their representatives for their time and generosity in participating in the study (online supplemental appendix A). We also thank the following organisations and their representatives for their support in the dissemination of the study and in facilitating the communication between study investigators and leaders of the healthcare provider organisations invited to participate in the study. Collaborating organisations had no role in study design and analysis:
- Ezequiel Garcia Elorrio (Instituto de Efectividad Clínica y Sanitária-IECS, Asociación de Clínicas, Sanatorios y Hospitales Privados de la República Argentina y Cámara de Entidades de Diagnóstico y Tratamiento Ambulatorio — ADECRA+CEDIM);
- Jason Arora (Medtronic, Latin America);
- Martha Oliveira (Associação Nacional de Hospitais Privados-ANAHP);
- Ricardo Zisis (AméricaEconomía);
- Silvio Junqueira (Johnson & Johnson, Latin America) and
- Teresa Tono (Organización para la Excelencia de la Salud-OES).
References and additional information
See the original publication
Originally published at https://www.ncbi.nlm.nih.gov.
About the authors and affiliations
Marcia Makdisse ,1,2 Pedro Ramos,1,3 Daniel Malheiro,1 Marcelo Katz,1 Luisa Novoa,1 Miguel Cendoroglo Neto,1 Jose Henrique Germann Ferreira,1 Sidney Klajner1
1 Hospital Israelita Albert Einstein, Sao Paulo, Brazil
2 Academia VBHC Educacao e Consultoria Ltda, Sao Paulo, Brazil
3 Medical Management Centre, Department of Learning, Informatics, Management and Ethics (LIME), Karolinska Institutet, Stockholm, Sweden












