This is an excerpt of the publication below, with the title above, focusing on the topic in question.
Global Horizons for Value-Based Care: Lessons Learned from the Cleveland Clinic
NEJM Catalyst
Chibueze Okey Agba, MBA, Joshua Snowden-Bahr, JD, MHA, Kushal T. Kadakia, MSc, Samer Abi Chaker, MD, MPH, James B. Young, MD, and Alex G. Forystek
June 28, 2022
One page summary by:
Joaquim Cardoso MSc.
Health Transformation Institute
Continuous transformation for universal health
Value Based Care Unit
July 5, 2022
Summary
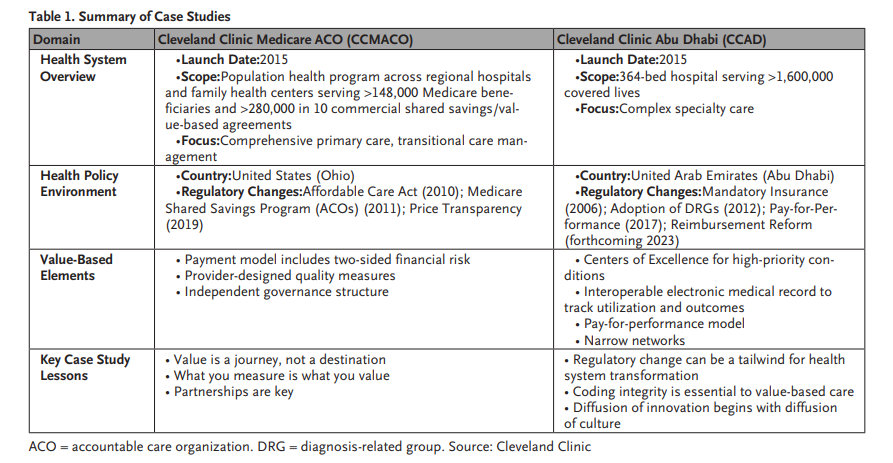
- The full version of this article reviews the Cleveland Clinic’s unique experience developing, operating, and refining value-based care models
(1) in the United States and
(2) The United Arab Emirates, with early applications and lessons learned
(3) in the United Kingdom,
… using these case studies to extrapolate challenges, successes, and opportunities for implementing global value-based care models.
- This excerpt focuses on the “Case Study 2: Cleveland Clinic Abu Dhabi”
ORIGINAL PUBLICATION (excerpt of full version)
Case Study #2: Cleveland Clinic Abu Dhabi
Model Overview
Cleveland Clinic expanded its international footprint in 2015 by opening a hospital in the UAE.
In contrast to CCMACO’s primary care focus, Cleveland Clinic Abu Dhabi (CCAD) focused on introducing technological and clinical innovations for specialties such as cardiac, transplant, and neurological care.
CCAD also leveraged the new “institute” model of Cleveland Clinic, with care organized around multidisciplinary teams for diseases and organs rather than traditional academic departments.
To expand coverage for new treatments and service lines and support payment system modernization, CCAD collaborated closely with the Departments of Health and Finance, and public and private insurers.
As of December 2021, CCAD has completed over 3.2 million outpatient visits, 94,000 surgeries and served 312,000 unique patients from over 80 countries.
Policy and Market Context
CCAD’s creation occurred amidst significant health system reform in the UAE, including the development of mandatory health care coverage and the adoption of prospective payment methodologies.
The Emirati population has faced a growing disease burden exacerbated by gaps in specialty care, particularly for complex procedures, resulting in increased costs for both payers and the Department of Health.
Together, the competitive market, evolving policy landscape, and opportunity to reduce pressure on public budgets and improve population health outcomes presented a unique environment for value-based care.
CCAD Timeline
CCAD is a joint venture between Cleveland Clinic and Mubadala Investment Company that employs physicians from more than 55 sub-specializations in its 14 institutes (including 6 centers of excellence).
In addition to expanding specialty care capacity, CCAD also introduced innovations across many diseases.
For example, CCAD became the market leader for services in cardiology (e.g., transcatheter aortic valve replacement) and digestive disease (e.g., robotic-assisted subtotal pancreatectomy).
CCAD has demonstrated great ability to provide high-quality care for patients with severe illness and conditions, treating a patient population with a case mix index (CMI) of 3.73 by the end of 2021. (CMI represents a relative value assigned to a diagnosis-related group of patients in an inpatient setting.
It is used in determining the resources required to provide care, and thus gives an indication of level of acuity.
By comparison for year-end 2021, the CMI for Cleveland Clinic was 1.94, with the Medicare CMI for Main Campus being 3.02.)
Contracts with the government and key private insurers helped establish CCAD’s base population, which by 2019 exceeded more than 1,000,000 covered lives, the majority of whom were Emirati nationals.
Likewise, the shift from inpatient to outpatient cases required engagement regarding Abu Dhabi’s payment methodology, which reimburses same-day procedures through per diem charges, inpatient encounters through international refined diagnostics-related group (IR-DRG) payments, and outpatient visits through fee-for-service.
For instance, service code specifications required patients to be admitted for more than 12 hours to account for markedly higher DRG reimbursement given that per diems did not allow hospital additional reimbursement for pathology, secondary procedures, consumables, and prostheses.
Under this system, potential financial misalignments could discourage clinical innovations that could offer benefits for safety, effectiveness, and convenience.
Metric development should be a collaborative process accounting for both physician and patient perspectives.
Additional reimbursement reforms are ongoing, and CCAD continues to prominently partner with the government to advocate sustainable solutions using the hospital’s 7 years of data reflecting tertiary-quaternary care delivery (e.g., extracorporeal membrane oxygenation [ECMO] and transplants).
Through July 2022, the Abu Dhabi Department of Health continues to use feedback from providers and payers to iterate its reimbursement system, including: changes to episode definitions; DRG pricing and weights; and adjustment mechanisms, both for quality-based institutional metrics and for outlier cases.
Challenges and Lessons Learned
- 1.Enabling regulations and strategies at the health-system level is essential for value-based care.
- 2.Coding integrity is essential to value-based care.
- 3. Diffusion of innovation begins with diffusion of culture.

1.Enabling regulations and strategies at the health-system level is essential for value-based care.
Abu Dhabi’s health care reforms were instrumental in incentivizing new care delivery models.
While the regulatory environment continues to evolve, Abu Dhabi pushes for improved performance and collaboration between payers, providers, and policy makers.
CCAD capitalized on this emphasis to navigate new terrain and improve access and outcomes.
CCAD’s experience illustrates how genuine payer-provider partnerships are necessary to modernize coverage policies and expand service offerings according to population needs.
For example, CCAD has engaged payers and regulators on Abu Dhabi’s new JAWDA program (Arabic for “quality”), which contains guidelines covering 19 services including pivotal offerings such as one-day procedures, cardiac surgery, and stroke.
2.Coding integrity is essential to value-based care.
Value does not exist in a vacuum; the unique needs of patients determine definitions.
Consequently, payment systems must be calibrated to account for differences in individual care needs and the population’s disease burden to ensure appropriate resource allocation.
CCAD has the UAE’s highest case-mix and has introduced novel procedures and technologies to advance specialty care.
Partnerships with payers and ongoing dialogue with regulators have enabled meaningful progress in coding and claims processing, including coverage for germline/somatic testing for oncotype diagnosis of breast cancer and pharmacotherapy consultations for heart failure and post-transplant patients. CCAD’s experience illustrates how sustainable financing for clinical innovation requires aligning incentives across contracting and coverage policies to support a checks-and-balances approach to billing.
Regular engagement among CCAD, payers, and regulators has also allowed better measurement of episodic costs through appropriate coding alignment.
3. Diffusion of innovation begins with diffusion of culture.
While delivery models are portable, the “secret sauce” of culture and continuous improvement can prove challenging to replicate.
CCAD leveraged enterprise capabilities to translate the Cleveland Clinic’s three-pronged culture of patient care, scientific research, and clinical education to the UAE.
First, CCAD adopted the same employment (salaried physicians) and organizational model (clinical institutes).
Second, CCAD used the same electronic medical record as Cleveland Clinic’s main campus, enabling replication (with localization) of care processes.
Third, many members from various levels of organizational hierarchy at CCAD came directly from Cleveland Clinic, providing continuity in leadership and vision.
Seeding the new system with U.S. leaders helped instill the Cleveland Clinic culture of “patients first” at CCAD and support the system’s integration into the global Cleveland Clinic enterprise.
Importantly, CCAD also recruited health care leaders from the UAE to its leadership team and hired hundreds of Emirati nationals from both the local community and abroad. Lastly, CCAD also invested in graduate medical education in the UAE to develop a pipeline for future talent.
About the authors and affiliations:
Chibueze Okey Agba, MBA
Chief Financial Officer, Hartford HealthCare, Hartford, Connecticut, USA
Joshua Daniel Snowden-Bahr, JD, MHA
Regional Director, Contracting & Business Development (International Markets), Market & Network Services, Cleveland Clinic Health System, Cleveland, Ohio, USA
Kushal T. Kadakia, MSc
MD Candidate, Harvard Medical School, Boston, Massachusetts, USA
Samer Abi Chaker, MD, MPH
Health Care Program Leader, CAPADEV LLP, Dubai, UAE
James B. Young, MD
Executive Director of Academic Affairs, Cleveland Clinic, Cleveland, Ohio, USA; Professor of Medicine & Vice Dean for Academic Affairs, Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, Ohio, USA
Alex G. Forystek
International Payer Contracts Manager, Cleveland Clinic, Cleveland, Ohio, USA
References and additional information
See original publication
Originally published at https://catalyst.nejm.org on June 28, 2022.
RELATED ARTICLES












