Health Systems Transformation (HST)
Research Institute and Knowledge Portal
Joaquim Cardoso MSc*
Chief Researcher, Editor and Strategy Officer
November 13, 2022
*MSc from London Business School — MIT Sloan Masters Program
Source: Commonwealth Fund
ORIGINAL PUBLICATION [Excerpt]
Mirror, Mirror on the Wall [2004]: Looking at the Quality of American Health Care through the Patient’s Lens
Commonwealth Fund
2006
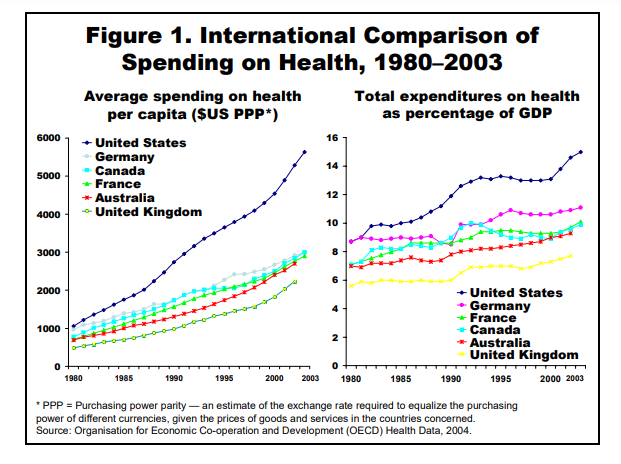
Health care leaders in the United States often claim that the American health system is the best in the world.
Based on both per-capita spending and the percentage of national income spent on health care, our nation is certainly far and away the leader. But are Americans really getting what they pay for?
A report from The Commonwealth Fund that examines how well the health system works from the perspective of patients confirms what several other recent studies have shown that the U.S. performs worse than its peer nations on several dimensions of quality.
the U.S. performs worse than its peer nations on several dimensions of quality.
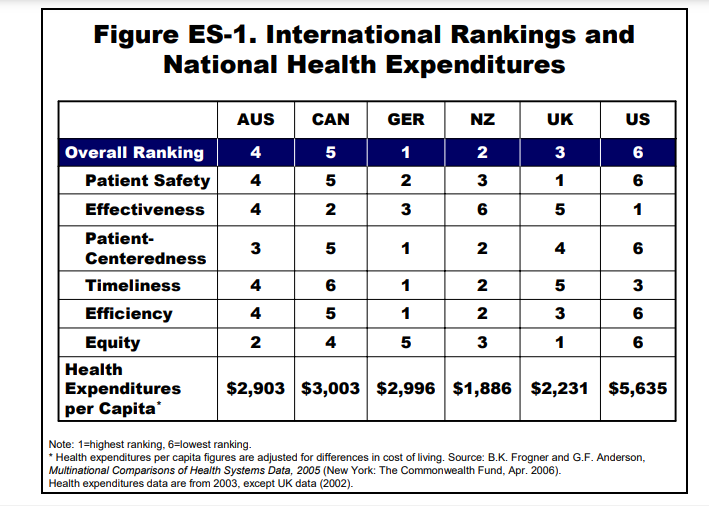
According to Mirror, Mirror on the Wall: Looking at the Quality of American Health Care Through the Patient’s Lens, four other industrialized nations Australia, Canada, New Zealand, and the United Kingdom scored better than the U.S. on safety, efficiency, effectiveness, and equity, while the U.S. ranked second-to-last on measures of “patient-centered” care.
four other industrialized nations Australia, Canada, New Zealand, and the United Kingdom scored better than the U.S. on safety, efficiency, effectiveness, and equity, while the U.S. ranked second-to-last on measures of “patient-centered” care.
The U.S. did, however, have the shortest waits for hospitalization and elective surgery, and placed second (to New Zealand) on prompt access to primary care physicians and specialists.
“While the U.S. spends the most on health care of any country, we’re not getting commensurate value from the view of patients,” said Fund president Karen Davis, the report’s lead author.
“We have the most highly skilled health professionals and most advanced medical technology, yet our system doesn’t ensure that patients fully benefit from this wealth of resources.”
“While the U.S. spends the most on health care of any country, we’re not getting commensurate value from the view of patients,” said Fund president Karen Davis, the report’s lead author.
“We have the most highly skilled health professionals and most advanced medical technology, yet our system doesn’t ensure that patients fully benefit from this wealth of resources.”
The Fund analysis, which was based on patients’ responses to the 2001 International Health Policy Survey and the 2002 International Health Policy Survey of Sicker Adults, used criteria for evaluating quality developed by the Institute of Medicine.
used criteria for evaluating quality developed by the Institute of Medicine.
For each of the quality dimensions below, an overall score was assigned to each country based on scores on several measures.
Patient Safety: U.S. Ranked Last
- Highest reports of medication errors (receiving the wrong medication or dose over the past two years).
- Most likely to say a medical mistake was made in their treatment.
Patient-Centered Care: U.S. Ranked Second-to-Last
Timeliness: U.S. Ranked Third
- Best on hospital admission waiting times.
- Next to last on waiting five days or more for physician appointment when last needed medical attention.
Efficiency: U.S. Ranked Last
- Last on being sent for duplicate tests by different health care professionals.
- Worst on not having medical records or test results reach doctor’s office in time for appointment
Effectiveness: U.S. Tied for Last
- Last in patients not getting a recommended test, treatment, or follow-up due to cost.
- Last in patients not filling a prescription due to cost.
Equity: U.S. Ranked Last for Lower-Income Patients
- Worst on patients having problems paying medical bills.
- Worst on patients being unable to get care where they live.
Infographic
Summary and Implications
These rankings summarize evidence on measures of quality as perceived or experienced by patients.
They do not capture important dimensions of effectiveness or efficiency that might be obtained from medical records or administrative data. Patients’ assessments might be affected by their experiences and expectations, which could differ by country and culture. Yet, reports from the World Health Organization (WHO) that compare health care system performance using measures such as life expectancy, infant mortality, or preventable years of life lost as well as health expenditures also suggest that the U.S. achieves the least for its population among these six countries.4 A working group — supported by The Commonwealth Fund and with experts from each of the five countries surveyed in 2004, the Organization for Economic Cooperation and Development (OECD), and WHO — developed a set of indicators that provide measures of clinical effectiveness.5 It found that none of the five countries included in the study — Australia, Canada, New Zealand, the U.K., and the U.S. — were systematically best or worst on measures of clinical effectiveness, confirming the mixed story reported by patients.
On four of the six domains of quality of care included in the Institute of Medicine framework, the U.S. performs relatively poorly from the patients’ perspective.
On timeliness, the U.S. performs about average. Effectiveness was the only measure on which the U.S. system performed slightly better than the five other countries, due largely to greater use of preventive care services and better care for the chronically ill. Notably, both of these dimensions of quality have been the focus of quality and reporting measurement in the U.S. for more than a decade.
Findings from the 2004 and 2005 surveys confirm many of the findings from surveys in 2001 and 2002.7
In the earlier surveys, the U.S. ranked last on measures of patient safety, patient-centeredness, efficiency, and equity. However, compared with the earlier surveys, the U.S. has improved on measures of effectiveness, from being tied for last place with Australia to ranking first among the six countries. The earlier surveys included only limited effectiveness measures while the more recent surveys contained a broader array of measures.
The findings suggest that, if the health care system is to perform according to patients’ expectations, the U.S. will need to remove financial barriers to care and improve the delivery of care.
Disparities in terms of access to services signal the need to expand insurance to cover the uninsured and to ensure that the system works well for all Americans. Based on these patient reports, the U.S. should improve the delivery, coordination, and equity of the health care system.
Originally published at https://www.commonwealthfund.org on January 1, 2004.
Citation:
Mirror, Mirror on the Wall: Looking at the Quality of American Health Care through the Patient’s Lens, Karen Davis, Ph.D., Cathy Schoen, M.S., Stephen C. Schoenbaum, M.D., M.P.H., Anne-Marie J. Audet, M.D., M.Sc., S.M., Michelle M. Doty, Ph.D., M.P.H., and Katie Tenney, The Commonwealth Fund, January 2004












