The Yuan
By Verena Voelter
Feb 09, 2022
Figure permission with credit from istockphoto.com
Data science is the future.
Electronic medical records that capture patients’ health data finally move us beyond the legacy systems of pen, paper and fax machines.
The start though has been paved with roadblocks in the form of bureaucracy, inefficiencies and physician burnout — because these first generation EMRs were developed in isolation based on the wrong purpose.
Today, we are experiencing a new wave of next gen EMRs that reverse the order by bringing in early the end users that really matter: healthcare professionals and patients.
Co-creating the right digital solution for the right purpose will bring better healthcare and more efficient systems too.
ZURICH —
“If you add one more useless initiative and one more piece of paperwork, I’ll jump out the window.” 1
This is what you may hear when you approach a doctor or a nurse when confronting them with a new software that you want them to use.
But, why that visceral reaction? Isn’t the move beyond paper, pen, and fax machines in healthcare a good thing? Don’t we finally have all the technology we need — soft- and hardware — available at our fingertips to ease the lives of doctors, nurses, and other healthcare professionals? How come that the first generation of electronic medical records (EMR, or often referred to as EHR, electronic health record -see below figure) has been such a failure in the eyes of many? 2
To understand the context, let’s look at the value chain from the patient’s perspective:
patients receiving care, providers delivering care and payers paying for that care. Remember the last time you went to see a doctor? There’s a high chance that while you were telling them your story, answering their questions, and putting forward your concerns, they would seemingly not pay attention but be hidden behind a computer screen. Why? Because of a system that is paranoid about numbers and documentation. Maybe that’s for justified legal reasons; maybe it’s for necessary billing reasons; or maybe it is for delivering better care through carefully tracking a patient’s story over time? The answer is likely to be all of the above. But shouldn’t it really be only about the latter? Today’s reality of a so-called fee-for-service system leads to an unprecedented pressure to produce. The system incentives numbers and quantity of services, products and procedures rather than rewarding the quality of care. It makes a doctor’s life resemble more the job of an accountant than a life at the forefront of patients’ needs.
So far so good. Other than an unpleasant feeling at the doctor’s office, what precisely is the issue?
Silos Kill Innovation
We do not have a problem of rising cost and lack of resources in healthcare. We have a problem of money in the wrong place and inefficiencies growing like weeds within the cracks in between silos. People acting in silos all along the value chain: providers, payers, pharma, policymakers, and patients with a fee-for-service structure only deepen the divides between these silos.
The way it shows up in real life is through doing more of the same. It leads to all sorts of unnecessary care, diagnostics, and treatments — all driving up administrative burden and billing. It also further fuels our quandary in healthcare: the decreasing quality in care (errors), the increasing cost (waste), and the widespread frustration within healthcare workers and patients. Breaking down those silos and fostering fluid workflows by connecting the dots will dissolve that quandary.
That is the promise of digital health powered by artificial intelligence (AI): to effectively smoothen out the cracks, to break down silos and to reconnect the dots between actors in the value chain.
For digital to work, you need data — electronic data.
In healthcare, this is about capturing patient-related health data.
Up to now though, the issue has been that first generation of EMRs (or EHRs, see figure below) have not precisely delivered on that promise.
Overview of Electronic Data Capture Terminology
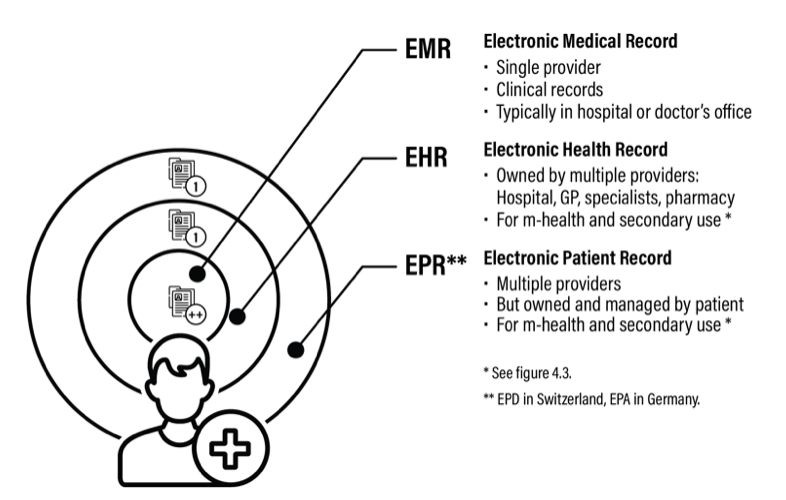
Figure reprinted with permission from ‘It Takes 5 to Tango — from Competition to Cooperation in Health Care.’1
Up to now though, the issue has been that first generation of EMRs (or EHRs, see figure below) have not precisely delivered on that promise.
First Generation EMRs Contribute to Physician Burnout
One of the reasons why this promise has not materialized is because “getting the data out of the EHR has been hampered in large measure because they were developed for billing,” said Dr Zeke Emanuel, in his landmark book “Which Country Has The Best Healthcare?”3
Created in isolation and without input from the end users (i.e., doctors and nurses), first-generation EHRs missed the real purpose: to ease the life of healthcare workers and make their work more efficient in order to focus time on what is the primary goal: caring for the patient -time being the essential factor to better care. A recent study by the non-profit United States-based Mayo Clinic showed that physicians spent one to two hours on EHRs and documentation for every hour spent face-to-face with patients.4A strong dose-response relationship between EHR usability and the odds of burnout was observed.
Usability and user friendliness, these are the key words. When we look at other sectors — such as the consumer good industry — there is much healthcare could learn. Companies like Cincinnati, Ohio-based Procter & Gamble (P&G) have long understood that standing side-by-side with their customers and observing them in their natural environment leads to continued innovation and better business results. The reason is simple: because customer needs are constantly being addressed with user-friendly solutions. Now, bringing in digital solutions, Guy Peri, Chief Data & Analytics Officer at P&G, said, “In order for us to understand and best serve consumers, we need to drive a data-enabled culture and operationalize algorithms into every major business decision.”5
In healthcare instead, the initial attempt to bring in digital data capture has created a bottleneck, multiplied paperwork, and otherwise worsened mistrust.
The first gen EMRs even forged a disbelief with healthcare workers that things will ever change for the better.
Breaking under the burden to produce and the pressure to meet relative value unit not only disheartens doctors, but also makes a patient feel like another number in a healthcare factory.
Dr Emanuel hits the nail on its head by calling out physician burnout — namely depression and disengagement — as one of the key challenges hampering quality patient care.
One way out of the dilemma “would be to reduce the hassle factors related to administration and… the burdens of the EHRs,” he concludes.
Next Gen EMRs, to Enable Better Data Analytics, Workflows and Empowerment
Now, the tide is turning.
People increasingly recognize the need for more customer-centricity in healthcare, e.g., patient-centricity, and for more connectedness to bring this patient-centric view to life.
The benefits are obvious: better care, higher quality, lower cost, and more satisfaction. There is ample literature describing that the move toward digitally, AI-powered value-based healthcare, which rewards results that matter to patients, will fix our broken systems.
What we need for this to become a reality is for software developers, tech experts and hardware companies to work hand-in-glove with clinicians, patients and the people who are eventually using that new data processing software, and this since the earliest stages of inception of the idea with true co-creation in cross-functional project teams.
The starting point of that co-creation is setting the right purpose.
If the ingoing goal for electronic data capture is to improve billing, the outgoing result in the clinics will be failure.
Conversely, first defining a common purpose and second, involving providers and patients into the user-testing is the secret sauce to success for the next generation of EMRs.
There is good news on the horizon as we generally see more and more cooperation of various important actors on the horizon. Recently, one example hit the headlines.
With a mega-deal of close to US$30 billion, Texas-based Oracle has incorporated a digital health data giant in an unprecedented Business Mergers and Acquisition Act late in 2021.
“With this transaction, Oracle’s corporate mission expands to assume the responsibility to provide our overworked medical professionals with a new generation of easier-to-use digital tools that enable access to information via a hands-free voice interface to secure cloud applications,” said Larry Ellison, the company’s cofounder, chairman and chief technology officer, in a statement.6
As a leading customer-centric expert in the field of electronic finance data, accounting and business administration, Oracle has the disruptive potential to lead to the next level of innovation for digital healthcare.
Their premise is encouraging, “We see big opportunities to expand cloud, AI and machine learning applications… with the goal to deliver zero unplanned downtime in the medical environment.”
This example sounds like music to our ears. Getting back that doctor’s visit time, for them to be able to look at you and listen to your needs? It certainly does to me.
Bridging engineering sets of expertise with clinicians’ experience and using electronic data as an empowerment for patients to master their own health is what next-gen EMRs and electronic patient records can deliver for us: healthier lives and happier work forces.
Bridging engineering sets of expertise with clinicians’ experience and using electronic data as an empowerment for patients to master their own health is what next-gen EMRs and electronic patient records can deliver for us: healthier lives and happier work forces.
References:
- Verena Voelter, 2021: “It Takes 5 to Tango — from Competition to Cooperation in Health Care” — Chapters 2 & 4
2. Bill Siwicki. Pandemic-era burnout: Nurses in the trenches say technology hurts and helps. www.HealthcareITnews.com, 9 Nov 2020.
3. Ezekiel J Emanuel. Which Country Has the World’s Best Health Care? Public Affairs New York, 2020
4. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc. 2020;95(3):476–487
5. Available at www.customers.microsoft.com, 17 Aug 2021.
6. Mike Miliard, www.HealthcareITnews.com, 20 Dec 2021
Originally published at https://www.the-yuan.com.
TAGS: Physician Burnout; Digital Health Issues, EMR usability; Patient Centric Health Care; EMR design




