The Health Strategist
research and strategy institute
for continuous transformation,
for in person health and digital health
Joaquim Cardoso MSc
Chief Research and Strategy Officer (CRSO)
May 8, 2023
ONE PAGE SUMMARY
A nationwide nursing survey conducted in September 2022, aimed to understand the factors contributing to nurse attrition and retention.
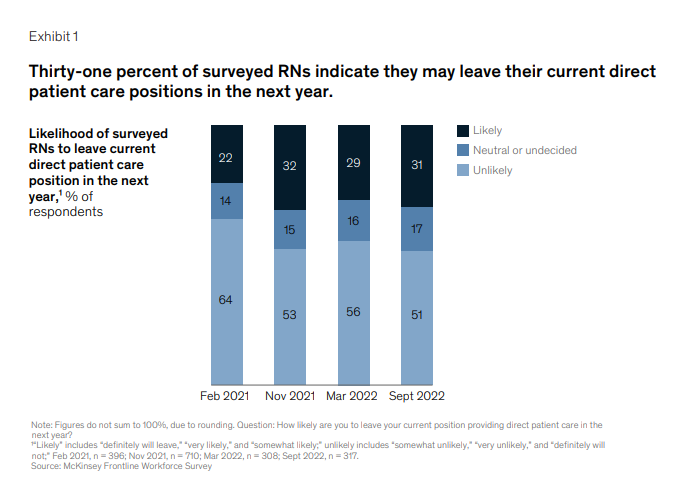
- The survey reveals that a significant number of nurses still express an intent to leave their current jobs, with 31 percent indicating a likelihood of leaving direct patient care roles within the next year.
- This trend has persisted since the onset of the COVID-19 pandemic, leading to a decrease in the overall active nursing workforce.
- However, there is some cause for optimism as healthcare organizations have implemented practices to improve the nurse experience, showing promising results.
The summary highlights the importance of attracting, supporting, and retaining a vibrant nursing workforce and promoting long-term stability.
- It emphasizes the need for healthcare organizations to design and deploy initiatives that address workforce needs, considering the evolving preferences of nurses in the post-pandemic era.
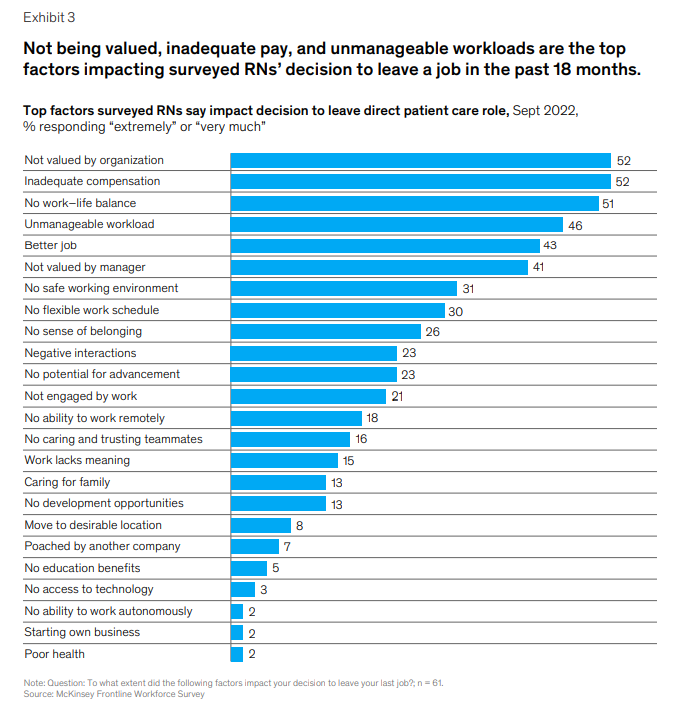
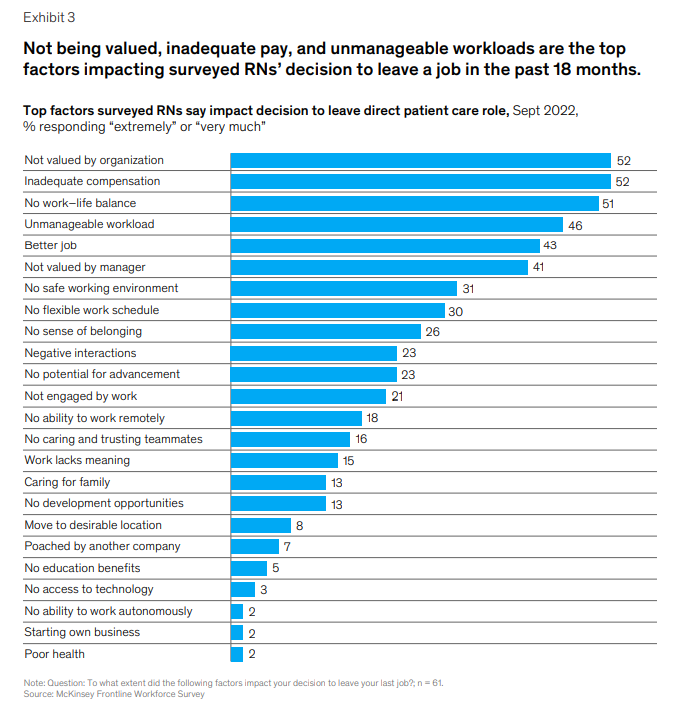
Factors contributing to attrition and retention among nurses are explored — with flexibility, meaning, and balance consistently ranked as the most important elements affecting nurses’ decisions to stay in direct patient care.
- Recognition, open communication, and well-being support initiatives, such as embedding breaks into the operating model, are also identified as crucial in supporting nurses’ job satisfaction.
1.Short-term strategies for stakeholders include appropriately recognizing nurses’ contributions and valuing them within the organization.
Implementing recognition initiatives and creating a supportive workplace culture are recommended to address the recognition gap and support nurses’ well-being.
2.In the medium term, stakeholders should focus on incorporating flexibility into nurses’ work schedules, as it is ranked highly effective for their well-being.
Health systems have successfully implemented creative approaches to provide schedule flexibility, despite the specialized and demanding nature of nursing work.
3.For the long term, investing in new-graduate nurses and building infrastructure for successful onboarding into the profession is vital.
Collaborative partnerships at the city and regional levels have proven effective in training and upskilling job seekers, creating meaningful career opportunities, and building a pipeline of healthcare workers.
To address the nursing shortage, healthcare organizations must continue their efforts to attract, strengthen, and grow a vibrant nurse workforce.
- The concerns and needs of nurses on the front line should be prioritized, and a multi-faceted approach involving various stakeholders is necessary.
- By addressing the core drivers behind nurses’ intentions to leave, the challenges facing the nursing profession can be overcome with consistent and dedicated attention.
Selected Image(s)

DEEP DIVE

Nursing in 2023: How hospitals are confronting shortages
Nearly a third of surveyed nurses still report an intent to leave their current jobs. Will hospitals’ efforts bend the curve?
Gretchen Berlin, Faith Burns, Connor Essick, Meredith Lapointe, and Mhoire Murphy
May 2023
When we tabulated the results of our first nationwide nursing survey almost two years ago, we were surprised to see such a high reported likelihood of nurses planning to leave their jobs-and we did not expect this trend to persist for such an extended period of time.
But that is what has happened in the wake of the COVID-19 pandemic. In fact, we have seen some of this reported anticipated turnover actually occur, as well as a decrease in the overall active nursing workforce. And there is still cause for concern: today, 31 percent of nurses still say they may leave their current direct patient care jobs in the next year, according to our most recent survey. That said, we are cautiously optimistic that some of the practices implemented by healthcare organizations to improve the experience of nurses are bearing fruit.
In this article, we share the latest data from our September 2022 frontline nursing survey of 368 frontline nurses providing direct patient care in the United States (see sidebar, “About the research”).
We offer these insights as resources for organizations as they continue their journeys of attracting, supporting, and retaining a vibrant workforce, as well as promoting longer-term workforce

What’s been happening in the nursing workforce
Nursing turnover continues to be a substantial challenge for healthcare organizations as the number of individuals with the intent to leave their jobs remains high.
In our most recent nursing survey, 31 percent of respondents indicated they were likely to leave their current role in direct patient care, a figure that has stabilized over the past six to 12 months yet is still higher than the 22 percent rate observed in our first survey in February 2021 (Exhibit 1).
Our research further shows that the intent to leave varies across settings.
For example, inpatient registered nurses (RNs) have consistently reported a higher intent to leave than the average of all surveyed RNs. In our most recent pulse survey of inpatient RNs, we saw intent to leave rise again, from 35 percent in fall 2022 to over 40 percent in March 2023.
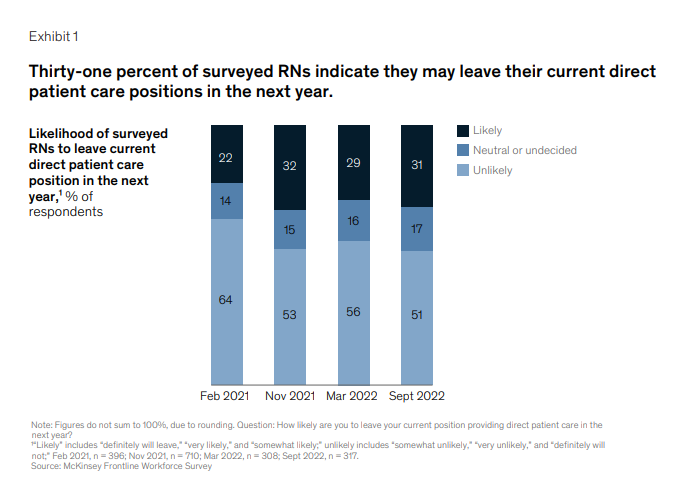
Recent analysis of studies comparing intent to leave to actual turnover show that both jumped meaningfully over the course of 2021. A study from Nursing Solutions Inc. (NSI) showed that actual reported hospital and staff RN turnover increased from 18 percent in fiscal year 2020 to 27 percent in fiscal year 2021; the same March 2022 study reported that the workforce lost about 2.5 percent of RNs in 2021. In the latest NSI report (March 2023), turnover reduced to 23 percent in fiscal year 2022 but still remains elevated compared with prepandemic levels. A Health Affairs study published in April 2022 found that the RN workforce fell by about 100,000 by the end of 2021, which is a “far greater drop than ever observed over the past four decades.”
This decline was particularly pronounced among midtenure nurses (aged 35 to 49). In terms of where they are going, nurses are both leaving the profession entirely as well as simply changing employers or roles. About 35 percent of respondents to our most recent survey who indicated they were likely to leave said they would remain in direct patient care (that is, at a different employer or role). The remainder said they intended to leave the bedside for nondirect patient care roles to pursue different career paths or education or to exit the workforce entirely.
With this persistently high turnover and the corresponding gathering storm in US healthcare, it is more important than ever for healthcare organizations to design and deploy initiatives that respond to and address workforce needs.
Most healthcare organizations have learned that attracting and retaining nursing talent in the postpandemic era will require a more nuanced understanding of what nurses are looking for in a profession and an employer.
Our four frontline nursing surveys over the past two years have enabled us to glean insights into factors contributing to both attrition and retention.
Frontline nursing respondents have consistently ranked elements of flexibility, meaning, and balance as the most important factors affecting their decision to stay in direct patient care (Exhibit 2).
Recognition, open lines of communication, and embedding breaks into the operating model (for example, during shifts, between shifts, and formal paid time off) have consistently been rated as the top initiatives to support well-being.
The nursing workforce has evolved over the course of the pandemic, and the strategies aimed at attracting and retaining tomorrow’s workforce have evolved as well.
To start, structural solutions that help to ensure a manageable workload-for example, consistent support staff, a safe environment, reduced documentation and administrative requirements, predictability of schedule, and ability to take paid time off-continue to be critical.
Surveyed nurses who left a direct patient care role in the past 18 months indicated that not being valued, unmanageable workloads, and inadequate compensation were the top factors in their decision to exit (Exhibit 3).
There are no one-size-fits-all solutions, but many healthcare organizations have adapted their approaches and carried out interventions that appear to be yielding results.
What stakeholders can do in the short term
- Our most recent survey found that 75 percent of nurses who left a job in the past 18 months reported that not being valued by their organization was a factor in their decision.
- In addition, 56 percent of total respondents reported that appropriately recognizing nurses for their contributions was the most effective initiative to support well-being.
- Surveyed nurses suggested various ways to respond to the recognition gap, including simple acknowledgement, appreciation of excellence, and reinforcement through broader workplace culture and support in the field.
Many healthcare systems have found ways to implement the nurses’ suggestions.
While more research is needed to understand the full impact of these efforts, they may be helpful short-term starting points in the attempt to show support for the workforce.

What stakeholders can do in the medium term
In the medium term, finding ways to incorporate flexibility into work schedules is an initiative that 63 percent of surveyed nurses ranked as the most effective for their well-being.
We saw similar responses regarding nurses’ decision to stay in their current position: 86 percent cited a flexible work schedule as the reason, which ranked second after “doing meaningful work.”
The nature of nurses’ work-typically specialized and always in demand-may make providing schedule flexibility seem daunting. But health systems have pursued several creative ways to address the issue.
The nature of nurses’ work-typically specialized and always in demand-may make providing schedule flexibility seem daunting.

What stakeholders can do in the long term
As health systems look beyond retaining the current workforce and meeting the expected demand for nursing talent, they could have a role to play in building a longer-term pipeline through investing in new-graduate nurses and in the infrastructure required to ensure successful onboarding into the profession.
The commitment to building a longer-term talent pipeline has expanded beyond individual health systems. Many city and regional partnerships have developed across the United States, bringing together critical stakeholders across the healthcare ecosystem to train and upskill unemployed and underemployed job seekers into healthcare occupations.
For example, the Birmingham Region Health Partnership, the result of close collaboration among government, healthcare employers, and other community partners, including Birmingham Business Alliance and Innovate Birmingham, won a $10.8 million grant from the Good Jobs Challenge to train and place over 1,000 jobseekers in the region.
Similar collaborative partnerships exist in Chicago, Baltimore, Philadelphia, among others, to build a pipeline of healthcare workers and to create meaningful career opportunities for historically excluded job seekers.

Retaining the current nursing workforce while looking ahead to the longer-term talent pipeline will be critical to meeting the projected shortfall in registered nurses.
There isn’t one answer to the challenges confronting healthcare organizations, and indeed, they have begun taking steps to address nurses’ stated needs through short-, medium-, and longer-term strategies that attract, strengthen, and grow a vibrant nurse workforce.
There is more to be done, especially in taking account of the voices of the front line and addressing the core drivers behind why nurses are planning to leave.
We are optimistic that the issues facing the nursing profession can be addressed, but this will require consistent and dedicated attention from many parties.
Originally published at https://www.mckinsey.com on May 5, 2023.












