This is a republication of the paper below, with the title above, highlighting the message in question.
Thematic analysis and natural language processing of job-related problems prior to physician suicide in 2003–2018
Wiley Online Library
Suicide and Life-Threatening Behavior
American Association of Suicidology
Kristen Kim MD,Gordon Y. Ye,Angela Maria Haddad BA,Nicholas Kos MD,Sidney Zisook MD,Judy E. Davidson DNP, RN, MCCM, FAAN
29 June 2022
Executive Summary by:
Joaquim Cardoso MSc.
health transformation . institute — research and strategy
mental health unit (suicide prevention initiative)
July 31, 2022 (acep image)
Through thematic analysis, six overarching themes were identified:
- 1.Incapacity to work due to deterioration of physical health
- 2.Substance use jeopardizing employment
- 3.Interaction between mental health and work-related issues
- 4.Relationship conflict affecting work
- 5.Legal problems leading to work-related stress
- 6.Increased financial stress
Natural language processing analysis confirmed five of these themes and elucidated important subthemes.
- This study highlights that the interplay between these factors and one’s work as a physician can lead to unique stressors that erode a physician’s wellbeing and ultimately lead to their demise.
- Physician wellness and burnout are no longer regarded as problems of individual physicians but rather that of institutions
- Similarly, physician suicide is a systemic problem reflective of the shortcomings of the medical profession.
- In accordance with the Hippocratic Oath, physicians swear to apply all measures required to heal the sick, and it is time to recognize that this applies even when the patient is one’s self or colleague.
- After all, healers cannot optimally heal unless they themselves are first whole.

ABSTRACT
Introduction
- Although previous studies have consistently demonstrated that physicians are more likely than non-physicians to experience work-related stressors prior to suicide, the specific nature of these stressors remains unknown.
- The current study aimed to better characterize job-related problems prior to physician suicide.
Methods
- The study utilized a mixed methods approach combining thematic analysis and natural language processing to develop themes representing death investigation narratives of 200 physician suicides with implicated job problems in the National Violent Death Reporting System database between 2003 and 2018.
Results
Through thematic analysis, six overarching themes were identified:
- incapacity to work due to deterioration of physical health,
- substance use jeopardizing employment,
- interaction between mental health and work-related issues,
- relationship conflict affecting work,
- legal problems leading to work-related stress, and
- increased financial stress.
Natural language processing analysis confirmed five of these themes and elucidated important subthemes.
Conclusions
- This is the first known study that integrated thematic analysis and natural language processing to characterize work-related stressors preceding physician suicide.
- The findings highlight the importance of bolstering systemic support for physicians experiencing job problems associated with their physical and mental health, substance use, relationships, legal matters, and finances in suicide prevention efforts.
The findings highlight the importance of bolstering systemic support for physicians experiencing job problems associated with their : (1) physical and (2) mental health, (3) substance use, (4) relationships, (5) Legal matters, and (6) finances in suicide prevention efforts.
ORIGINAL PUBLICATION (excerpt of the full version)
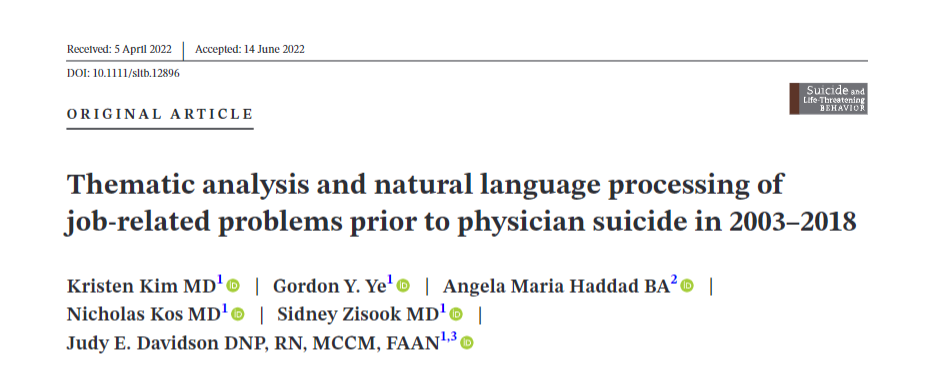
Thematic analysis and natural language processing of job-related problems prior to physician suicide in 2003–2018
Wiley Online Library
Suicide and Life-Threatening Behavior
American Association of Suicidology
Kristen Kim MD,Gordon Y. Ye,Angela Maria Haddad BA,Nicholas Kos MD,Sidney Zisook MD,Judy E. Davidson DNP, RN, MCCM, FAAN
29 June 2022
INTRODUCTION
Physician suicide is both a deeply personal matter and a broader public health concern requiring systemic interventions (Moutier, Myers, Feist, Feist, & Zisook, 2021).
One in fifteen physicians experience suicidal ideation (Shanafelt et al., 2021).
Suicidality occurs across all stages of training starting from medical school: 27.2% of medical students experience depression and 11.1% endorse suicidal ideation (Rotenstein et al., 2016).
One in fifteen physicians experience suicidal ideation (6,6%)
Suicidality occurs across all stages of training starting from medical school: 27.2% of medical students experience depression and 11.1% endorse suicidal ideation
While older studies have found that both male and female physicians are at increased risk for suicide (Dutheil et al., 2019), more recent works suggest that only female physicians are at a higher risk for suicide compared to their non-physician counterparts (Davis, Cher, Friese, & Bynum, 2021; Duarte et al., 2020; Ye, Davidson, Kim, & Zisook, 2021).
Regardless of the relative prevalence of physician suicide, each death is a personal, social, and community tragedy, and the medical community has an ethical responsibility to prevent further needless deaths (DeCamp & Levine, 2021; Gold & Schwenk, 2020).
Physicians with recent suicidal ideation compared to those without are more likely to endorse situational stressors including personal, financial, health, and occupational problems (Brooks, Gendel, Early, & Gundersen, 2017).
The impact of job-related stressors, in particular, has recently gained increased attention as physicians experience heightened occupational stress during the COVID-19 pandemic (Moutier et al., 2021).
Previous studies have consistently demonstrated that physicians are more likely than non-physicians to have work-related stressors including recent job crises prior to suicide (Duarte et al., 2020; Gold, Schwenk, & Sen, 2021; Gold, Sen, & Schwenk, 2013; Ji, Robertson, Patel, Peacock, & Resnick, 2020; Ye et al., 2021).
Existing literature has also revealed a correlation between professional burnout and suicidal ideation (Van Der Heijden, Dillingh, Bakker, & Prins, 2008).
However, a 2018–2019 study of 1354 physicians found that this association disappeared when adjusted for depression (Menon et al., 2020).
The specific nature of the job-related problems contributing to physician suicide remains unclear.
Clarifying the nature of such stressors is a necessary step in designing and implementing effective suicide prevention strategies.
Existing literature has also revealed a correlation between professional burnout and suicidal ideation …However, a 2018–2019 study of 1354 physicians found that this association disappeared when adjusted for depression
The National Violent Death Reporting System (NVDRS) of the Centers for Disease Control and Prevention (CDC) integrates data from certified medical examiner (CME) and law enforcement (LE) death investigation narratives, toxicology data, and death certificates (National Violent Death Reporting System (NVDRS), 2021).
It is the most comprehensive database of violent deaths in the US and the only one with occupation codes available.
The NVDRS is a voluntary, state-based reporting system.
The number of participating states increased from six in 2003 (Maryland, Massachusetts, New Jersey, Oregon, South Carolina, and Virginia) to 42 in 2018 (including District of Columbia and Puerto Rico and all states except Arkansas, Florida, Idaho, Mississippi, Montana, North Dakota, South Dakota, Tennessee, Texas, and Wyoming).
This study examined NVDRS death investigation narratives to examine the specific nature of job-related problems prior to physician suicide with the goal of informing future suicide prevention efforts.
The National Violent Death Reporting System (NVDRS) of the Centers for Disease Control and Prevention (CDC) integrates data from certified medical examiner (CME) and law enforcement (LE) death investigation narratives, toxicology data, and death certificates (National Violent Death Reporting System (NVDRS), 2021).
It is the most comprehensive database of violent deaths in the US and the only one with occupation codes available.
The NVDRS is a voluntary, state-based reporting system.

METHODS
Study sample and design
The study sample included 200 physicians who died by suicide and had known job-related problems prior to death in the NVDRS dataset between 2003 and 2018. The cases were selected using pre-coded fields for occupation and job problem.
Each death had up to two, paragraph-long death investigation narratives (one CME and/or one LE), which described the circumstances surrounding the suicide.
Adapting a previously published study design (Davidson et al., 2021), the authors conducted a mixed methods approach integrating manual thematic analysis (Braun & Clarke, 2006) and natural language processing (NLP) to determine overarching themes of the job-related problems cited in the narratives.
The CDC provided ethical oversight for this study.
The study did not meet the requirements for oversight from the institutional review board because it involved research with deceased individuals.
The authors followed Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines (Tong, Sainsbury, & Craig, 2007).
Thematic analysis
Inductive thematic analysis was performed by reviewing the death investigation narratives before generating relevant codes and themes. Three authors (KK, AH, NK) independently read the CME and LE narratives before generating codes that best characterized the job-related problems. The authors collaborated to achieve consensus on codes and to identify overarching themes that best captured the codes. To protect the identity of the decedents, the CDC prohibits use of direct quotes from the dataset and recommends use of blinded composite cases. The authors revisited the narratives to create composite cases for each theme.
Deductive thematic analysis was performed based on codes and themes developed in a previous study on job-related problems prior to nurse suicide (Davidson, Ye, Parra, et al., 2021). The authors examined the physician narratives to determine whether the codes and themes derived from the nurse suicide study were applicable to physician suicide.
Natural language processing
Latent Dirichlet Allocation (LDA) (Blei, Ng, & Jordan, 2003) was performed (GY) on the narratives of the 205 suicides initially coded as physicians with a known job problem. LDA is an NLP topic modeling technique that assumes a small number of abstract themes exists within a collection of documents: in this case, the CME and LE death investigation narratives for the physician suicides. Each theme may then be described as a list of words or phrases that occur frequently in or are unique to the specific theme.
Standard NLP preprocessing steps were followed: investigation narratives with five or fewer characters were removed, yielding the 204 CME and 188 LE narratives for analysis. Remaining NLP preprocessing and analysis steps have been described previously (Davidson et al., 2021) and may be found in Appendix A.
To interpret the LDA-determined themes, three investigators with clinical domain knowledge (KK, AH, NK) assessed topic definitions for clinical and real-world relevance. During this manual review stage, five non-physicians were identified and removed from consideration, yielding a total of 200 physicians included for analysis. LDA was not rerun because removal of these five suicides did not impact the clinical and real-world significance of LDA results.

RESULTS
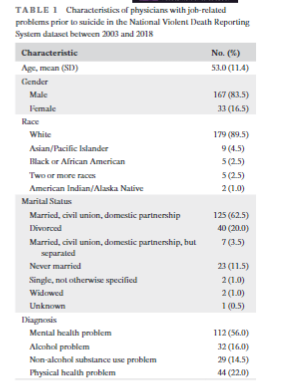
The 200 physicians were predominantly male (n = 167 males, 83.5%), White (n = 179, 89.5%), and married (n = 125, 62.5%); the mean (SD) age was 53.0 (11.4) years.
Furthermore, 56.0% had mental health problems, 16.0% had alcohol problems, 14.5% had non-alcohol substance use problems, and 22.0% had physical health problems (Table 1).
TABLE 1. Characteristics of physicians with job-related problems prior to suicide in the National Violent Death Reporting System dataset between 2003 and 2018
See the original publication
Inductive thematic analysis determined the following themes: incapacity to work due to deterioration of physical health; substance use jeopardizing employment; interaction between mental health and work-related issues; relationship conflict affecting work; legal problems leading to work-related stress; and increased financial stress.
NLP analysis also identified each of these themes, except incapacity to work due to deterioration of physical health.
NLP analysis also identified each of these themes, except incapacity to work due to deterioration of physical health.
NLP analysis also elucidated important subthemes: alcohol under substance use jeopardizing employment; depression and anxiety under interaction between mental health and work-related issues; divorce and affair under relationship conflict affecting work; and malpractice and civil litigation under legal problems leading to work-related stress.
Other important concepts that arose from NLP analysis were “forced into retirement” and “resign.”
Upon re-examination, the data showed that the majority of physicians were unemployed or pending job loss and typically not by choice; they were forced to retire or resign due to their health, substance use, or legal issues.
- 1.Incapacity to work due to deterioration of physical health
- 2.Substance use jeopardizing employment
- 3.Interaction between mental health and work-related issues
- 4.Relationship conflict affecting work
- 5.Legal problems leading to work-related stress
- 6.Increased financial stress
1.Incapacity to work due to deterioration of physical health
Physicians suffered from physical health problems that hindered their work performance, leading to emotional distress.
These problems were sometimes acute, such as recent surgery, injury, or illness:
The victim had been suffering from back pain and recently underwent surgery.
The pain had continued to be so severe that they were unable to work and had to leave their job. The victim had become depressed due to their condition, worsening health and inability to practice medicine.
In other narratives, the physical issues were chronic, such as chronic pain gradually wearing down the physician’s ability to work.
Some affected physicians’ mental ability (e.g., worsening cognition), while others affected physical ability (e.g., a surgeon with a tremor).
As elucidated by NLP, “forced into retirement” was a common phrase that depicted the lack of control that physicians felt when transitioning out of their career due to such ailments.
The victim had chronic medical issues that included tremor and arthritis.
Their physical symptoms had been worsening for several years. The victim was recently forced to retire from their career as a physician. Their partner stated that the victim had become dissatisfied with life during the progression of their physical symptoms.
2.Substance use jeopardizing employment
Physicians also struggled with substance use (e.g., alcohol or prescription drug use), which negatively impacted employment.
The substance use would escalate and interfere with work performance.
This would lead to investigation by their workplace and/or state medical board, jeopardizing medical licensure and employment.
The victim had a long history of addiction to alcohol and prescription drugs.
They were under investigation by the medical board and the hospital had revoked their privileges. On the morning of the incident, the victim had failed a urine toxicology and was informed that their medical license would be suspended.
3.Interaction between mental health and work-related issues
It is known that uncontrolled mental health problems increase risk for suicide, but the current analysis elucidated that the interaction between mental health and work may be an additional risk factor.
Occupational stressors sometimes led to mental health problems, most commonly depression and anxiety.
The victim had a mental breakdown due to the immense stress that the victim was under at work. The victim had started antidepressant and anti-anxiety medications. They were supposed to begin work again during the week of the incident.
In other cases, mental health issues were longstanding and affected physicians’ ability to work.
Importantly, many physicians were reluctant to engage in mental health treatment.
The victim had a long history of depression and suicide attempts.
They had previously been taking medications but recently stopped due to concerns that the medications interfered with their work. They were worried that they might have to quit their job if they did not start improving their work performance.
Importantly, many physicians were reluctant to engage in mental health treatment.
4.Relationship conflict affecting work
Interpersonal conflicts were regularly implicated in the death narratives. Relationship issues with colleagues led to hostile and uncomfortable work environments.
The victim had felt they had been mistreated at work. They experienced intimidation and bullying from superiors, and they had verbal altercations with other coworkers.
More frequently, strained relationships with family members, including recent or impending divorce and extramarital affairs, affected physicians’ work and vice versa.
The victim had been having marital difficulties related to work stress.
Their partner recently discovered that the victim had an extramarital affair with a coworker, which further strained the marriage.
5.Legal problems leading to work-related stress
The narratives cited legal problems related to clinical matters (e.g., malpractice or misconduct cases) that jeopardized medical licensure and/or employment.
Common legal problems were related to over-prescription of narcotics, sexual misconduct toward patients, and substance use (e.g., substance use leading to loss of licensure).
Victims were often under active investigation by the state medical board, employer, and/or law enforcement.
The acuity and uncertainty of pending litigation appeared to heighten suicide risk.
A patient had filed a complaint about the victim treating them inappropriately.
The victim was also dealing with a malpractice lawsuit. They were under investigation by the medical board and was awaiting a hearing about whether they would be able to continue working at the hospital.
6.Increased financial stress
Finally, the narratives mentioned increased financial stress due to work-related matters (e.g., closure of one’s medical practice) as a source of increased suicidality.
Sometimes the financial stress was related to the aforementioned legal problems (i.e., legal problems would lead to job loss, which would increase financial stress).
The victim was dealing with increased financial stress and was at the risk of losing their home and closing their medical practice.

Deductive thematic analysis
A previous study on job-related problems prior to nurse suicide conceptualized themes as events in a timeline leading to suicide: chronic struggle, peri-job loss, trapped in crisis, no way out, and finding a way out [through suicide] (Davidson, Ye, Parra, et al., 2021).
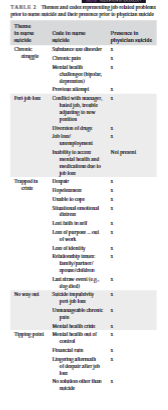
Though these themes differed from those generated in the current study in their scope, re-examining the physician data with the codes and themes extracted from the nurse death investigation narratives in mind revealed substantial overlap in job-related problems across both disciplines (Table 2).
Both disciplines had antecedents to suicide including relationship issues with job superiors, being investigated for substance use, threat of loss of license due to substance use, and mental health or physical health issues preventing work.
Conversely, absent in the physician data was the inability to access mental health and medications due to job loss.
Additionally, there was a notable addition of legal issues in the physician data, which was not present in nurse suicides.
TABLE 2. Themes and codes representing job-related problems prior to nurse suicide and their presence prior to physician suicide
See the original publication

DISCUSSION
This is the first known study that utilized thematic analysis and NLP to characterize job-related factors in physician suicide.
This integrated approach capitalized on the authors’ clinical and professional expertise and the objectivity and efficiency of machine learning.
The authors identified six themes among job-related problems preceding physician suicide.
NLP analysis confirmed all but one of these themes and revealed important subthemes. Incapacity to work due to deterioration of physical health was likely not identified by NLP because physical health issues were described as the various, specific conditions affecting work performance (e.g., back pain, tremor), which were not grouped as a common theme by NLP.
Comparing this data with themes and codes developed in a prior study (Davidson, Ye, Parra, et al., 2021) revealed significant overlap between job problems preceding suicide across the disciplines of nursing and medicine.
When reviewing the quantitative analysis of nurse and physician suicides, it was previously reported that both were older than the general population of suicides by approximately 10 years (Davidson, Proudfoot, Lee, Terterian, & Zisook, 2020; Davis et al., 2021; Ye et al., 2021).
Here, the results suggest that suicide risk is associated with premature retirement due to uncontrolled health issues preventing continued employment.
These findings inform future interventions for suicide prevention among healthcare professionals.
Physical health is often absent from lists of work-stressors (West, Dyrbye, & Shanafelt, 2018), but poor health leads to compromised work performance and subsequent work stress (Frank, 2004; Taub, Morin, Goldrich, Ray, & Benjamin, 2006).
Physicians traditionally have neglected their own health in favor of their professional and personal obligations (George, Hanson, & Jackson, 2014; Gross, Mead, Ford, & Klag, 2000), but this tendency has negative ramifications for patient care (Frank, 2004; Frank, Segura, Shen, & Oberg, 2010).
Physicians traditionally have neglected their own health in favor of their professional and personal obligations …, but this tendency has negative ramifications for patient care …
Barriers challenging physician self-care include embarrassment, lack of identified primary care manager, scheduling issues, and concerns regarding confidentiality (Kay, Mitchell, Clavarino, & Doust, 2008).
Perhaps even more detrimental to self-care is the unspoken culture of medicine, which engenders self-sacrifice, deferred needs and delayed rewards (Myers, Gabbard, & Myers, 2008).
Perhaps even more detrimental to self-care is the unspoken culture of medicine, which engenders self-sacrifice, deferred needs and delayed rewards …
Adding to this is the “compulsive triad” of doubt, guilt and an exaggerated sense of responsibility, which is considered the hallmark of the physician’s personality (Gabbard, 1985).
Adding to this is the “compulsive triad” of doubt, guilt and an exaggerated sense of responsibility, which is considered the hallmark of the physician’s personality
While these traits can be adaptive, they also can lead to problems allocating time for self-care. Indeed, the culture of medicine promotes the belief that physicians are never ill and often views attention to their own needs as a sign of weakness.
These barriers coupled with the novel finding of the prominent role deteriorating health plays in physician suicide beg for action.
Some barriers, such as lack of a primary care physician, scheduling challenges and concerns for confidentiality, are readily modifiable.
Addressing lifelong character traits and cultural issues is more challenging.
In a legendary yet timeless piece on the role of compulsiveness among physicians, Gabbard proposes that the first step toward a solution is the identification and recognition of the problem and its ramifications (Gabbard, 1985).
In a legendary yet timeless piece on the role of compulsiveness among physicians, Gabbard proposes that the first step toward a solution is the identification and recognition of the problem and its ramifications …
Identifying the personal, structural and cultural gaps that prevent physicians from attending to their own health is essential.
Medicine must dispel the myth of never-ill physicians who place the needs of their patients before their own to the detriment of their own health.
The culture of medicine must shift away from its outdated mandate of extreme self-sacrifice and embrace changes that promote optimal physician health as an avenue to improved patient care.
Physicians also experience mental health (Moutier, 2018) or substance use (Martinez et al., 2016) problems and are reluctant to seek help (Bonnie, Appelbaum, & Recupero, 2018; Center et al., 2003; Shanafelt et al., 2021).
Physicians also experience mental health … or substance use … problems and are reluctant to seek help …
Such reluctance can be attributed to the abovementioned barriers with concerns about confidentiality being especially relevant (Rubanovich, Zisook, & Bloss, 2022).
A practical intervention is to establish confidential pathways for treatment of mental illness and substance use disorders, such as the UC San Diego Healer Education Assessment and Referral program (Moutier et al., 2012; Norcross et al., 2018; Zisook et al., 2016), through which physicians can receive counseling and referral to outpatient treatment.
The importance of anonymous screening to encourage engagement in health-seeking behaviors cannot be over-stated (Rubanovich et al., 2022).
The importance of anonymous screening to encourage engagement in health-seeking behaviors cannot be over-stated …
Furthermore, medical institutions must cultivate a sense of community at work and promote work-life integration (Shanafelt & Noseworthy, 2017).
Workplace harassment has been associated with suicidal ideation among attendings (Eneroth, Gustafsson Sendén, Løvseth, Schenck-Gustafsson, & Fridner, 2014).
Conversely, supportive meetings to discuss demanding experiences at work correlated with a lower level of suicidal ideation among attending and empowering leadership with a lower level of suicidal ideation among residents (Eneroth et al., 2014).
At all stages of their career, physicians need safe supportive work environments to thrive.
Furthermore, medical institutions must cultivate a sense of community at work and promote work-life integration
Despite assumptions that physicians are financially stable, the narratives frequently mentioned financial insecurity as a source of distress prior to suicide.
Physicians in training have low financial literacy and investment-risk tolerance, high debt, and deficits in their financial preparedness (Ahmad, White, Hiller, Amini, & Jeffe, 2017).
Incorporating personal finance education into medical school curricula and advocating for policies that reduce student debt can alleviate financial burdens.
The findings also suggest that legal and psychological support, especially during malpractice investigations and “fit for duty” evaluations, is warranted.
Incorporating personal finance education into medical school curricula and advocating for policies that reduce student debt can alleviate financial burdens
… legal and psychological support, especially during malpractice investigations and “fit for duty” evaluations, is warranted.
This study has several limitations. It is a post-mortem evaluation with qualitative data limited to two paragraphs per death. The narratives are largely based on objective data and interviews with loved ones and may not fully capture the reasons behind the decision to suicide. Additionally, the physicians included were predominantly male and White; thus, the results may not reflect the impact of specific work-related stressors of underrepresented minorities in medicine, for example, stress due to microaggressions. Finally, at the time of writing, the database did not include all states or data on suicides after 2018. Healthcare workers have experienced increased emotional distress during the COVID-19 pandemic (Laboe, Jain, Bodicherla, & Pathak, 2021; Moutier et al., 2021); future study of the NVDRS database will be required to understand the specific impact of the pandemic on physician suicide.

CONCLUSION
- This study highlights new and important findings regarding physician suicide that provide meaningful pathways to prevention.
- It is unsurprising that health problems, substance use, and psychosocial stressors heighten suicide risk as these are known risk factors for physician suicide (Brooks et al., 2017; Ye et al., 2021).
- However, this study highlights that the interplay between these factors and one’s work as a physician can lead to unique stressors that erode a physician’s wellbeing and ultimately lead to their demise.
- Physician wellness and burnout are no longer regarded as problems of individual physicians but rather that of institutions (Shanafelt & Noseworthy, 2017).
- Similarly, physician suicide is a systemic problem reflective of the shortcomings of the medical profession.
- In accordance with the Hippocratic Oath, physicians swear to apply all measures required to heal the sick, and it is time to recognize that this applies even when the patient is one’s self or colleague.
- After all, healers cannot optimally heal unless they themselves are first whole.
In accordance with the Hippocratic Oath, physicians swear to apply all measures required to heal the sick, and it is time to recognize that this applies even when the patient is one’s self or colleague.
After all, healers cannot optimally heal unless they themselves are first whole.
About the authors & affiliations:
Kristen Kim MD 1
Gordon Y. Ye 1
Angela Maria Haddad BA 2
Nicholas Kos MD1
Sidney Zisook MD 1
Judy E. Davidson DNP, RN, MCCM, FAAN 1,3
1 Department of Psychiatry,
University of California San Diego, La Jolla, California, USA
2 Universidad Autónoma de Guadalajara Facultad de Medicina,
Zapopan, Mexico
3 University of California San Diego Health,
La Jolla, California, USA