How the United States Compares (Insights for Brazil ad other countries)
Commonwealth Fund
Molly FitzGerald, Munira Z. Gunja, Roosa Tikkanen
MARCH 15, 2022
Dr. Megan Mahoney, center, examines patient Consuelo Castañeda, right, as medical scribe Anu Tirapasur documents the visit at the Stanford Family Medicine office on April 9, 2019, in Stanford, Calif. U.S. adults are the least likely to have a regular physician or place of care, or a longstanding relationship with a primary care provider. Photo: Jeff Chiu via AP Photo
Toplines
- From access to care to coordination of patient services, the U.S. lags far behind other wealthy countries in primary care, a new Commonwealth Fund report finds
- The U.S. primary care system has been weakened by decades of chronic underinvestment.
- Policymakers should act now to strengthen it, including by narrowing the wage gap between generalists and specialists.
Primary care providers (PCPs) serve as most people’s first point of contact with the health care system.
These clinicians build relationships with their patients over time and help coordinate care delivered by other health care providers.1 Evidence shows that a strong foundation of primary care yields better health outcomes overall, greater equity in health care access and outcomes, and lower per capita health costs.2
But in the United States, decades of underinvestment and a low provider supply, among other problems, have limited access to effective primary care.3
This brief highlights gaps in the U.S. primary care system by comparing its performance to systems in 10 other high-income countries. We draw on data from the Commonwealth Fund’s 2019 and 2020 international surveys, along with data from the Fund’s 2020 International Profiles of Health Care Systems. (See “How We Conducted This Study” for further details.)
Highlights
- U.S. adults are the least likely to have a regular physician or place of care, or a longstanding relationship with a primary care provider.
- Access to home visits or after-hours care is lowest in the U.S.
- U.S. primary care providers are the most likely to screen for social service needs.
- Half of U.S. primary care physicians report adequate coordination with specialists and hospitals — around the average for the 11 countries studied.
Table of Contents (TOC)
- Accessibility
- Care Continuity
- Comprehensiveness of Care
- Care Coordination
Findings: Accessibility
Good access to primary care includes the ability to a book an appointment with your doctor or regular place of care when care is needed.
Research shows that in countries with better access to primary care, patients are less likely to forgo needed care and, as a result, more likely to have better health outcomes.4
Good access to primary care includes the ability to a book an appointment with your doctor or regular place of care when care is needed.

Having a regular doctor or place of care is important for preventing disease, managing chronic conditions, and coordinating specialty care.
Prior research has found the U.S. has a lower supply of physicians compared to other countries.5
The majority of adults in all 11 countries reported having a regular doctor or place of care, but adults in the U.S. and Sweden reported this at significantly lower rates than adults in most of the countries.
Having a regular doctor or place of care is important for preventing disease, managing chronic conditions, and coordinating specialty care.
Findings: Care Continuity
Continuity of care is critical to the quality of treatment over time. There are several policies that can support the establishment of long-term patient–provider relationships.
In Norway, patients are automatically registered with a PCP, while in the United Kingdom, patients are registered6 with a general practitioner, or GP, of their choice.7
In the United States, such registration is far less common, usually mandatory only for patients enrolled in certain managed care plans.
In Norway, patients are automatically registered with a PCP, while in the United Kingdom, patients are registered6 with a general practitioner, or GP, of their choice
Prior research shows that patients who have a long-term relationship with their PCP are less likely to go to the emergency department.8
Primary care continuity is also associated with improved care coordination and increased patient satisfaction.9
… patients who have a long-term relationship with their PCP are less likely to go to the emergency department.
Continuity of care is critical to the quality of treatment over time. There are several policies that can support the establishment of long-term patient–provider relationships.

Among adults with a regular PCP, those in the U.S. were significantly less likely to report having a longstanding relationship — five years or more — with this provider, compared to all other countries but one (Sweden).
In the Netherlands and Germany, nearly three of four adults reported having a longstanding relationship with their PCP.
Several factors may contribute to the relative lack of continuous care in the U.S., including financial barriers, changes in insurance coverage, provider networks and location, and the nation’s low supply of PCPs.
In the Netherlands and Germany, nearly three of four adults reported having a longstanding relationship with their PCP.
Home visits can strengthen the patient–provider relationship, evidence shows
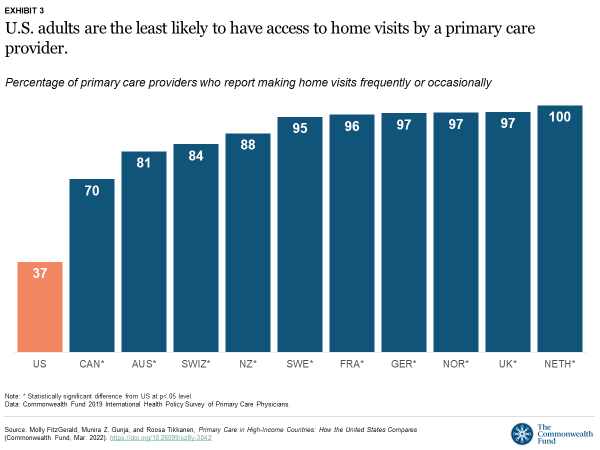
Home visits can strengthen the patient–provider relationship, evidence shows.10
Yet PCPs in the U.S. are significantly less likely to offer home visits than PCPs in all other countries in this analysis.
In contrast, all PCPs in the Netherlands, and nearly all in France, Germany, Norway, Sweden, and the United Kingdom offer home visits.
…all PCPs in the Netherlands, and nearly all in France, Germany, Norway, Sweden, and the United Kingdom offer home visits.
The lack of home visits in the U.S. also may be because of the low supply of providers. But a lack of financial incentives, time, and training for U.S. physicians, as well as safety and liability concerns, are additional possible factors.11
Making sure primary care is accessible outside standard practice hours can help patients avoid emergency department trips for nonurgent care.12
Among the 11 countries, PCPs in the U.S. are the least likely to report having after-hours arrangements for their patients.
Nearly all PCPs in Germany, the Netherlands, New Zealand, and Norway have after-hour care arrangements.
In fact, nearly all general practitioners in Norway provide at least 50 hours of after-hours care annually to maintain their registration as GPs.13
Making sure primary care is accessible outside standard practice hours can help patients avoid emergency department trips for nonurgent care
Nearly all PCPs in Germany, the Netherlands, New Zealand, and Norway have after-hour care arrangements.

Findings: Comprehensiveness of Care
Comprehensive primary care is about more than just physical health; it also focuses on behavioral health and social needs that affect health, such as access to nutritious food, safe housing, and stable income.
PCPs are ideally positioned to monitor this range of needs and provide referrals to specialists as well as service providers outside the health care system.
Comprehensive primary care is about more than just physical health; …
PCPs are ideally positioned to monitor this range of needs and provide referrals
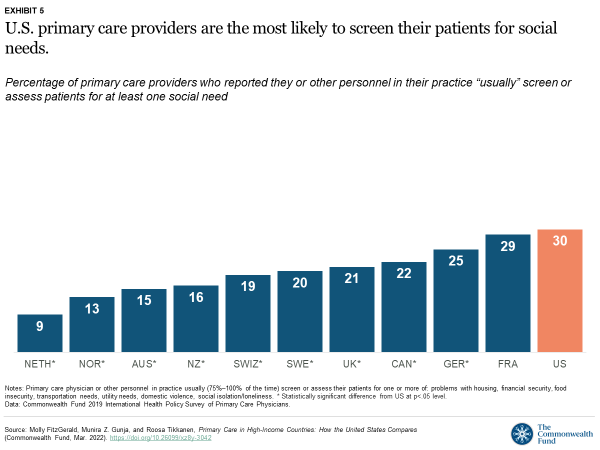
Across all the countries, it is still relatively uncommon for PCPs to assess patients’ social needs, including for housing, food security, transportation, and ability to pay for basic needs like utilities, as well as to screen for exposure to domestic violence or feelings of social isolation or loneliness.
Across all the countries, it is still relatively uncommon for PCPs to assess patients’ social needs …
Such screenings were most common in the U.S. and France and least common in the Netherlands and Norway
Such screenings were most common in the U.S. and France and least common in the Netherlands and Norway — a difference that, at least for the U.S., may be attributable to chronic underinvestment in social services that support healthy living conditions and population health.14
Patients in the Netherlands and Norway are less likely than those in the U.S. to say they worry about getting their social needs met (data not shown).15
Patients in the Netherlands and Norway are less likely than those in the U.S. to say they worry about getting their social needs met

Adults in Canada, the U.S., and Norway were more likely to report that their PCP provided them with information on how to get help for their social needs — although this difference is only statistically significant with respect to Sweden, Switzerland, and Australia.
In some countries, like the United States, higher rates of receiving such information may be a response to higher rates of material hardship, along with a weaker social safety net.
In addition to having universal health care, robust welfare states like Sweden offer free or low-cost education, subsidized childcare and transportation, generous parental leave policies, and guaranteed pension payments.

Comprehensive primary care is best provided by multidisciplinary teams of health professionals that include social workers, mental health providers, and others specially trained to address social and behavioral health needs.
Comprehensive primary care is best provided by multidisciplinary teams of health professionals — that include social workers, mental health providers, and others specially trained to address social and behavioral health needs.
PCPs in Canada and the U.S. are the most likely to have social workers on their care teams, while this is almost never the case with German or Swiss PCPs.
The relatively higher rate of social workers on U.S. primary care teams may be a function of underinvestment in certain types of social services.
For example, comparatively less U.S. funding is directed to meeting the needs of young and working-age people through early childhood education and parental leave allowances.16
The presence of social workers in U.S. primary care settings may therefore reflect the complexity and uncertainty of existing safety-net programs. Relatively small changes in earnings for people with low income, for instance, can result in Medicaid enrollment “churn” — cycling on and off coverage — as well as ineligibility for the Supplemental Nutrition Assistance Program (SNAP).17
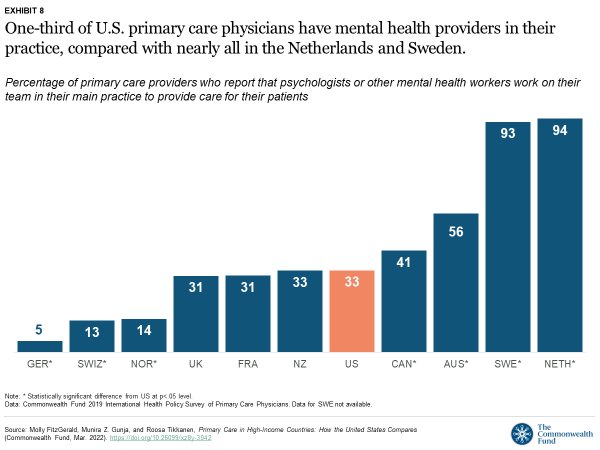
Nearly all Dutch and Swedish PCPs reported having a mental health worker on their team, compared to one-third of PCPs in the U.S. and only 5 percent in Germany. This is despite the burden of mental health needs being among the highest in the U.S.18
Nearly all Dutch and Swedish PCPs reported having a mental health worker on their team, compared to one-third of PCPs in the U.S. and only 5 percent in Germany.This is despite the burden of mental health needs being among the highest in the U.S.
Findings: Care Coordination
Another central feature of primary care is the purposeful coordination of treatment provided by a patient’s PCP with that provided by other clinicians in different settings.
Because primary care is first-contact care, PCPs are well positioned to coordinate with the wider health care system, making referrals to other health professionals as needed.
Because primary care is first-contact care, PCPs are well positioned to coordinate with the wider health care system, making referrals to other health professionals as needed.
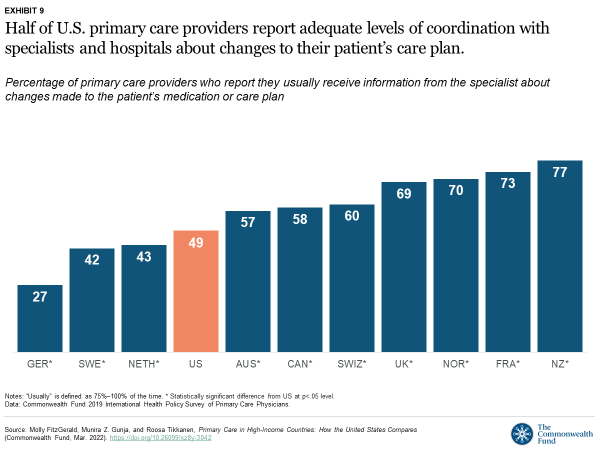
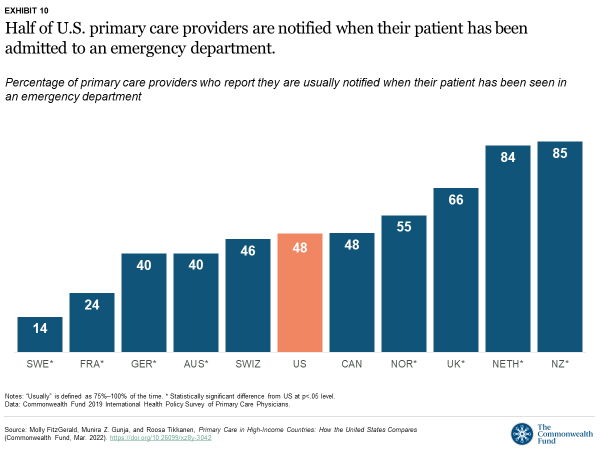
Less than half of U.S. PCPs reported that they are usually informed when another provider changes their patient’s care plan or medication regimen, and that they are usually informed if their patient is admitted to a hospital or emergency department.
hat’s about the average for the 11 countries we studied. PCPs from New Zealand were the most likely to usually receive this information from specialists and hospitals.
Less than half of U.S. PCPs reported that they are usually informed when another provider changes their patient’s care plan or medication regimen, and that they are usually informed if their patient is admitted to a hospital or emergency department.
Commonwealth Fund researchers have found that a substantial proportion of U.S. PCPs do not routinely receive timely notification when their patients are seen by other providers, nor do they routinely receive important information resulting from these visits.19

Discussion
While there is a shortage of health workers globally, our analysis demonstrates that the U.S. primary care system trails far behind those of other countries in many areas, particularly when it comes to health care access and continuity. These findings are consistent with prior research on the challenges facing primary care more broadly and are likely an outcome of chronic underinvestment in primary care in the United States.20 Evidence suggests that the shortcomings of U.S. primary care disproportionately affect predominantly Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.21
There are several policy options for U.S. policymakers to consider as they work to improve primary care:
- Narrow the U.S. wage gap between generalist and specialist physicians and subsidize medical school tuition fees to incentivize medical students to opt for primary care practice.
- Invest in telehealth to allow more patients to access primary care.
- Expand payment reforms that reward and hold providers accountable for the continuity of care.
- Acknowledge the importance of meeting social service needs to people’s health and well-being.
- Create financial incentives to facilitate communication between patients’ providers.
1.Narrow the U.S. wage gap between generalist and specialist physicians and subsidize medical school tuition fees to incentivize medical students to opt for primary care practice.
The United States has the largest wage gap and highest tuition fees among the countries we studied.22
2.Invest in telehealth to allow more patients to access primary care.
This is particularly important for rural residents and people with low income, who face some of the tallest barriers to getting care.23
Only one in five U.S. PCPs reported that their practice provided video consultations before the COVID-19 pandemic, and just over a third of U.S. patients with a regular doctor or place of care said they have used a secure website or patient portal to communicate with their provider within the past two years (data not shown).24
3.Expand payment reforms that reward and hold providers accountable for the continuity of care.
Countries with top-performing health systems are able to reduce avoidable mortality through investment in primary care models that ensure continuity of care.25
Ensuring that patients can receive care after-hours, and get treatment in their own homes, is critical to avoiding unnecessary trips to the emergency department.
There has been some recent progress in this area: Medicare eliminated the requirement for providers to provide documentation that a home visit, instead of an office visit, is medically necessary.26
By removing this administrative hurdle, this change should allow physicians to care for patients more easily in their homes and reduce fragmentation of care.
4.Acknowledge the importance of meeting social service needs to people’s health and well-being.
Social determinants of health account for as much as 55 percent of health outcomes.27 While U.S. primary care appears to be somewhat more comprehensive in terms of screening for social needs, our analysis also finds that U.S. adults are more likely to worry about their social needs in the first place — especially compared to adults in Germany, the Netherlands, Norway, and Sweden.28
5.Create financial incentives to facilitate communication between patients’ providers.
The fragmentation in care between U.S. PCPs and specialists can have a negative impact on care quality, cost, and outcomes.29
In New Zealand, primary health organizations received additional per capita funding to promote health and coordinate care.30
Introducing similar incentives in the U.S. could help.
Conclusion
In its efforts to improve primary care, the United States can learn a lot from what other high-income countries are doing.
But there are also ample lessons to be learned from lower-income countries, such as Costa Rica, whose health system is anchored by robust, community-oriented primary health care.31
And, in the era of COVID-19, a greater understanding of changes and challenges to primary care, particularly from the perspective of the physician, is needed.
To that end, the Commonwealth Fund will release findings from its latest international survey, focusing on primary care physicians, in summer 2022.
In its efforts to improve primary care, the United States can learn a lot from what other high-income countries are doing.
But there are also ample lessons to be learned from lower-income countries, such as Costa Rica, whose health system is anchored by robust, community-oriented primary health care.31

HOW WE CONDUCTED THIS STUDY
This analysis used data from the Commonwealth Fund’s 2019 and 2020 international health policy surveys.
2019 Commonwealth Fund International Health Policy Survey of Primary Care Physicians
The 2019 Commonwealth Fund International Health Policy Survey of Primary Care Physicians was administered to nationally representative samples of practicing primary care doctors in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. These samples were drawn at random from government or private lists of primary care doctors in each country except France, where they were selected from a nationally representative panel of primary care physicians. Within each country, experts defined the physician specialties responsible for primary care, recognizing that roles, training, and scopes of practice vary across countries. In all countries, general practitioners (GPs) and family physicians were included, with internists and pediatricians also sampled in Germany, Switzerland, and the United States.
The questionnaire was designed with input from country experts and pretested in most countries. Pretest respondents provided feedback about question interpretation via semistructured cognitive interviews. SSRS, a survey research firm, worked with contractors in each country to survey doctors from January through June 2019; the field period ranged from seven to 19 weeks. Survey modes (mail, online, and telephone) were tailored based on each country’s best practices for reaching physicians and maximizing response rates. Sample sizes ranged from 500 to 2,569, and response rates ranged from 15 percent to 49 percent — comparable to those in the 2015 survey. Final data were weighted to align with country benchmarks along key geographic and demographic dimensions.

2020 Commonwealth Fund International Health Policy Survey
For the 2020 Commonwealth Fund International Health Policy Survey, data were collected from nationally representative samples of noninstitutionalized adults age 18 and older in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Switzerland, Sweden, the United Kingdom, and the United States. Samples were generated using probability-based overlapping landline and mobile phone sampling designs in all but three countries. In Norway, Sweden, and Switzerland, respondents were randomly selected from listed or nationwide population registries. In the U.S., an address-based sampling frame was also incorporated to ensure a representative sample of respondents. Respondents completed surveys via landline and mobile phones, as well as online, in Sweden, Switzerland, and the United States.
International partners cosponsored surveys, and some supported expanded samples to enable within-country analyses. Final country samples ranged from 607 to 4,530 participants. The survey research firm SSRS was contracted to conduct the survey with country contractors from February through May 2020. The field period across countries ranged from four to 15 weeks.
Response rates varied from 14 percent to 49 percent. Data were weighted using country-specific demographic variables to account for differences in sample design and probability of selection.
ACKNOWLEDGMENTS
The authors thank the Commonwealth Fund’s Melinda Abrams, Corinne Lewis, Reginald Williams, and Laurie Zephyrin for their helpful review comments; and Evan Gumas and Relebohile Masitha for their careful data review.
Originally published at https://www.commonwealthfund.org on March 15, 2022.
This analysis used data from the Commonwealth Fund’s 2019 and 2020 international health policy surveys.