Site editor:
Joaquim Cardoso MSc.
Health Transformation — institute for research and strategy
October 6, 2022
This is an excerpt of the article “Mortality Rates for Medicare Advantage Are Actually Significantly Lower and Better, with Fewer Deaths ”, with the title above, focusing on the topic in question.
Intergroup Institute
George C. Halvorson
September 30, 2022
We live longer with Medicare Advantage.
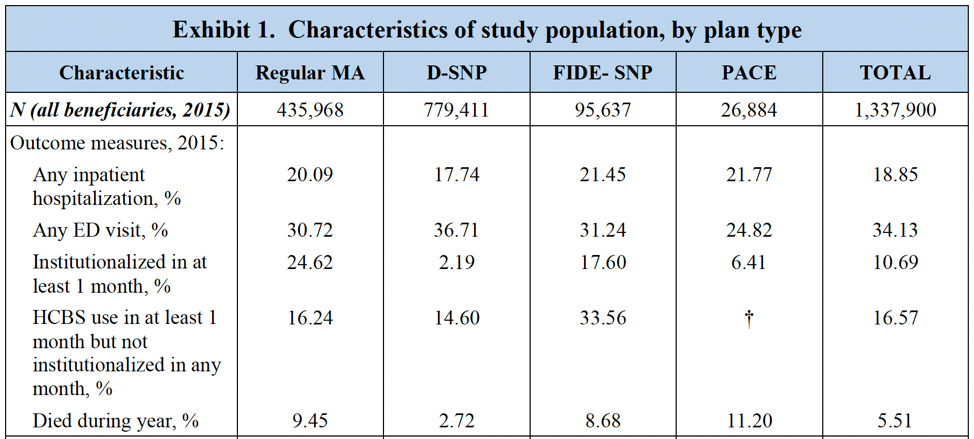
The final official report from The U.S. Department of Health and Human Services “Comparing Outcomes for Dual Eligible Beneficiaries in Integrated Care” shows that
- the mortality rate for each version of Medicare Advantage is both lower and better than the mortality rate that we currently have for standard fee-for-service Medicare in this country and
- the Medicare Advantage mortality results have been improving over time and will probably continue to improve.
When we are trying to figure out ways of measuring the value of the care we are receiving in any setting, one of the most effective measures of value for us both individually and collectively for each category of care should now be whether the care allows us and enables us to survive.
… one of the most effective measures of value for us both individually and collectively for each category of care should now be whether the care allows us and enables us to survive.
This new study breaks important and credible ground on that issue.
Survival rates can be a useful and legitimate way of determining whether or not we are receiving good care, and this study shows us those rates for our most important Medicare Advantage members.
We know that fee-for-service Medicare far too often delivers bad care [e.g. blindness, & amputation]
We know that fee-for-service Medicare has the highest rates of blindness for our older population in the world and we know that fee-for-service Medicare has the highest rates of amputations for our older population — with $6 billion worth of amputations being done each year for our older Americans.
- We know that diabetic blindness can be massively reduced and prevented for most people with the right treatment — and we know that adequate, appropriate and timely treatment is much more likely to happen in our Medicare Advantage settings and it is extremely rare in far too many of our fee-for-service Medicare settings.
- We also know that poor people with diabetes are much more likely to lose limbs in this country because fee-for-service Medicare has no programs to change that terrible pattern of care and only Medicare Advantage patients get the right care in large numbers of their settings.
Medicare Advantage plans are paid by the month for each patient and they are not paid by the piece for each piece of care, so Medicare Advantage plans do the basic work to keep people from going blind and to keep people from losing limbs to amputation and the plans can do that because capitation both gives plans the resources they use to do that work and then rewards them financially when the care is successful.
Medicare Advantage plans are paid by the month for each patient and they are not paid by the piece for each piece of care, so Medicare Advantage plans do the basic work to keep people from going blind and to keep people from losing limbs to amputation …
… and the plans can do that because capitation both gives plans the resources they use to do that work and then rewards them financially when the care is successful.
The fee-for-service Medicare care sites make $100,000 on each amputation and they bill for $8 billion in amputations each year.
The care provided in the amputation situations can be extremely difficult and it is inherently dangerous and it should not be happening for most of those people.
The fee-for-service Medicare care sites make $100,000 on each amputation and they bill for $8 billion in amputations each year.
High mortality rates happen for that surgery.
That is clearly very wrong in terms of patterns of care in too many settings.
The Medicare Advantage plans have strong incentives to improve care and they respond directly and intentionally to those incentives at multiple levels.
The Medicare Advantage caregivers know that 90 percent of those amputations literally started with ulcers on the feet of the patients.
They know that 90 percent of the ulcers on patients’ feet could have been either prevented or cured. Simply having patients wearing clean socks and having dry feet can stop over 40 percent of those ulcers.
The Medicare Advantage caregivers know that 90 percent of those amputations literally started with ulcers on the feet of the patients. They know that 90 percent of the ulcers on patients’ feet could have been either prevented or cured.
Simply having patients wearing clean socks and having dry feet can stop over 40 percent of those ulcers.
There is a huge differences in care for many of our lowest income Medicare members when they join Medicare Advantage plans.
Patients with chronic conditions do particularly well when they are in Plans because each member has their own link to the care delivery network of each plan and their Medicare Advantage care teams are delivering patient specific care for their conditions.
The basic care delivery model for Medicare Advantage is based on doing the right things to improve care.
The basic care delivery model for Medicare Advantage is based on doing the right things to improve care.
The major epidemic of blindness going on for far too many of our senior Americans today can be dealt with just by managing the blood sugar for each of the diabetic patients.
The capitation payment to the Medicare Advantage plans creates the resources needed to do that work and then the capitation payment approach rewards plans when patients do not have expensive vision loss and blindness remediation expenses.
It’s much less expensive to save vision than to lose it.
Far too many health care economists and too many health care journalists and media outlets do not understand the massive impact that capitation payment model has on everyday care.
They think of it as an alternative cash flow device.
It actually restructures care by putting the financial rewards into better care outcomes and then provides the resources needed to reengineer care and deliver the better model.
Far too many health care economists and too many health care journalists and media outlets do not understand the massive impact that capitation payment model has on everyday care.
It actually restructures care by putting the financial rewards into better care outcomes and then provides the resources needed to reengineer care and deliver the better model.
Some examples of those differences are relatively easy to see.
- The plans prevent $100,000 amputations by intervening with the foot ulcer development and
- they also prevent a very high percentage of congestive heart failure crisis events …
… by intervening as quickly as a patient with that disease starts to show sudden weight gains in their home.
Medicare Advantage plans have a long history of successes on preventing bad outcomes and crisis events with congestive heart failure as a disease.
The plans know that you can avoid hospital admissions for that disease by identifying all of the people at risk for a congestive heart failure crisis and by interacting directly with each patient to keep those future crisis from happening.
The CHF crisis events cost $20,000 to $40,000 each.
They are a favorite care event for many fee for service Medicare care sites because they are so profitable and functionally easy to treat.
They are part of the $4 trillion in billable events that make up the American health care economy.
The CHF crisis events cost $20,000 to $40,000 each. They are a favorite care event for many fee for service Medicare care sites because they are so profitable and functionally easy to treat.
Medicare Advantage plans do some basic things to keep those costs and those care events out of the system.
The functional reality is that when the care team from the Medicare Advantage plan intervenes very early in each crisis, almost half of them simply don’t happen.
More than 40 percent of those crisis are avoided with proactive care by the Medicare Advantage plans.
… when the care team from the Medicare Advantage plan intervenes very early in each crisis, almost half of them simply don’t happen.
Plans often assign nurses directly to each patient and some plans even put easy to use scales in the home because the easiest detection tool is often significant and rapid weight gain by the patient.
Some plans even put scales in people’s homes that have direct telephone links on the scale to alert the care team as soon as possible when the weight gain happens.
Congestive heart failure crises can be very painful and sometimes frightening and they can be both damaging and fatal.
So cutting them by over 40 percent is good for the patients and their families and it saves significant money for the plans because those unnecessary admissions don’t happen.
When you look at the massive reduction in patient mortality rates that the Health and Human Services study of people in the Medicare Advantage plans for dual eligible showed to everyone in America who looks at that data,…
… those kinds of programs that reengineer care to change the level of care crisis for their members clearly added up to important gains in peoples life expectancy and lives.
Similar programs have a similar and obvious positive impact on reducing asthma attacks for a significant number of patients.
Those attacks can also be painful and frightening and life threatening — and a high percentage of those attacks can be avoided with patient focused team care from the plans.
… asthma attacks …can also be painful and frightening and life threatening — and a high percentage of those attacks can be avoided with patient focused team care from the plans.
Those normal care improvement programs for standard Medicare Advantage patients work extremely well and they are far overshadowed daily on a patient focused basis by the full array of support needs that happen for the Medicare Advantage special needs patients and particularly for the low-income and high medical need patients who are enrolled in the Medicare Advantage special needs plans and in Medicaid simultaneously.
Those programs and their impacts were all included in the new government report that looked at all four approaches to funding care.
Originally published at: https://www.intergroupinstitute.org
To be continued …