Obesity-related NCDs account for over 4.7 million deaths globally each year, half of which occur amongst people under the age of 70
The Economic Impact of Overweight & Obesity in 8 Countries
World Obesity and RTI International
March, 2022
Executive Summary
by Joaquim Cardoso MSc.
Chief editor of The Health Strategy Blog
March 3, 2022
What is the cost of obesity in non high-income countries?
Much of what we know about the economic impact of overweight and obesity come from studies in high-income countries, despite us knowing that the challenges we face are global and far-reaching. [9]
To address this, World Obesity and RTI International have joined forces to improve the economic evidence on the impact of overweight and obesity.
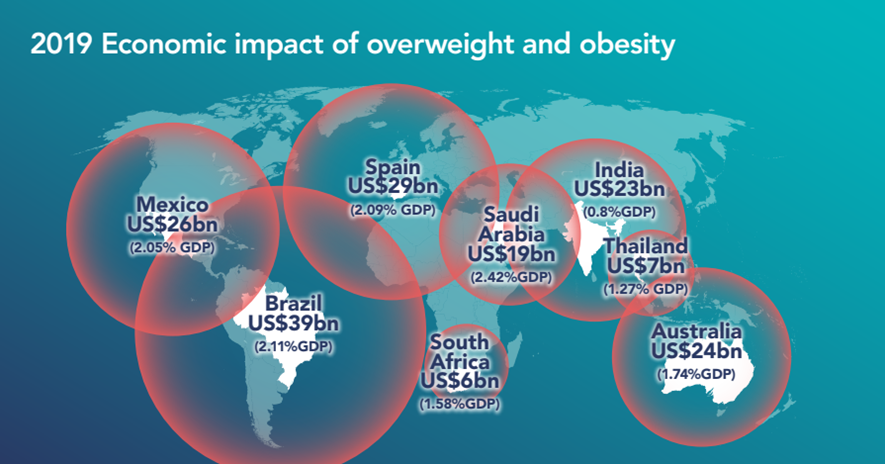
A new pilot study — published in BMJ Global Health — has estimated the economic impact of obesity at between 0.8–2.4% of annual GDP in eight countries.
- In Brazil the estimated the economic impact of obesity is 2.11% of GDP (in 2019)
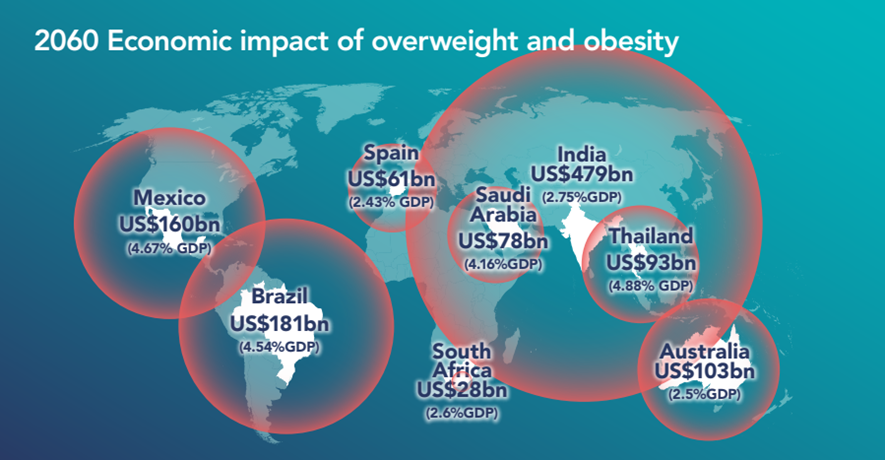
The study also calculates the cost of continued political inaction, with economic impacts projected to rise up to 4.8% by 2060 if urgent action is not taken by public health leaders around the world.
- In Brazil the estimated the economic impact of obesity for 2060 is 4.54 % of GDP , what is more than double of 2019 estimates (2.11%)
The economic and societal impact of overweight and obesity are substantial for countries at different income levels.
What are the components of obesity costs?
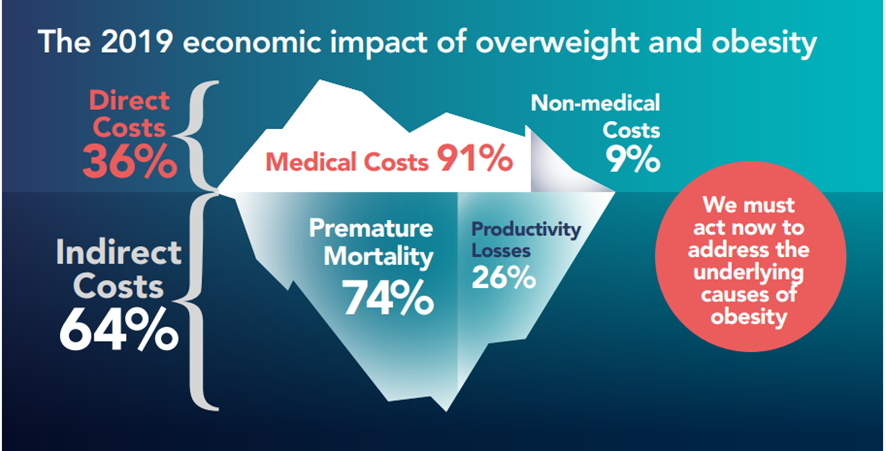
The economic impact of overweight and obesity across the 8 pilot countries is largely made up of indirect costs (64% of the total cost).
- Premature mortality contributes with 74% of the indirect costs
- Productivity losses account for the other 26% of the indirect costs
What is the business case for obesity?
Maintaining or reducing the prevalence of overweight and obesity can reduce the economic impacts of overweight and obesity in the future.
- Halting the overweight and obesity prevalence at 2019 levels would results average annual savings of 13.2% between 2020–2060 (That is equivalent to an average annual cost reduction of $12.5 billion)
- Slowing the increase in overweight and obesity by 5% from projected levels would result in an average annual savings of 5.2% between 2020–2060 (That is equivalent to an average annual cost reduction of $3.3 billion)
What is the stigma around obesity?
- Weight stigma is often the result of a misunderstanding of the complex causes of obesity.
- Weight gain is often attributed to individual failure alone and there is a lack of information and understanding about the complex mix of genetic, environmental, and biological factors that drive it.
What is the call?
- If urgent action is not taken, the study reports that the economic impact in all eight countries is projected to rise between 2.4% — 4.8% by 2060.
- However, the study is also optimistic that reversing this trend are possible. The authors found that maintaining or reducing the prevalence of overweight and obesity can reduce the economic impacts in the future.
What are the recommendations?
Ahead of the full report in spring 2022, World Obesity and RTI are calling for the implementation of evidence-based policies to support populations globally to live healthier lives.
Specifically, World Obesity are calling for the adoption of the obesity ‘ROOTS’ framework — which was agreed by a panel of global obesity experts in 2020 — to drive obesity policy and advocacy in national settings.
- R (Recognise) — Recognise obesity as a disease and a risk factor, and promote understanding of its complexities
- O (Obesity Surveillance) — Develop obesity surveillance and monitoring programmes and adopt evidence-based strategies for addressing obesity
- O (Obesity Prevention) — Implement obesity prevention and management policies across the life course
- T (Treatment) — Ensure treatment is equitably offered and accessible to all who want it
- S (Systems Based Approaches) — Adopt systems-based approaches to address obesity
ORIGINAL PUBLICATION (full version of the short report)

The Economic Impact of Overweight & Obesity in 8 Countries
World Obesity and RTI International
March, 2022
Summary report
By RTI International and World Obesity, with contributions from the University of California, Berkeley MDP Consulting Team
Introduction
Obesity is a complex, relapsing disease caused by various factors, including genetic susceptibility, high energy-dense nutrition, low physical activity, and stress. Obesity is also a risk factor for numerous other noncommunicable diseases (NCDs), such as cardiovascular disease, diabetes, and cancer.[1]
Obesity-related NCDs account for over 4.7 million deaths globally each year, half of which occur amongst people under the age of 70.[2]
Unfortunately, obesity is on the rise; between 1975 and 2016, obesity prevalence increased in every country around the world.[3]
Increasing obesity prevalence has both health and economic impacts but the latter has not been explored greatly at a global level.
A better understanding of the economic consequences of overweight and obesity should help strengthen the case for action.
To help build the body of economic evidence, RTI International and the World Obesity Federation conducted this pilot study to examine the economic impact of overweight and obesity over the next 40 years across eight countries.
These eight countries were selected as they represented a range of geographies and income levels, and they all had previous estimates for comparison purposes.
This study will be expanded to include most countries around the world in 2022.

Key takeaways
The economic and societal impact of overweight and obesity are substantial for countries at different income levels.
Differences in economic impact across countries can be partly explained by variations in:
- Overweight and obesity prevalence
- Strength of the health system
- Economic strength (GDP/capita)
- Wage differences
- Employment rates
- National healthcare expenditure
- Age distribution of attributable mortality
The economic impact of overweight and obesity across the 8 pilot countries is largely made up of indirect costs.
Projected increases in economic impact are largely driven by predicted increases in overweight and obesity prevalence, population changes and economic growth.
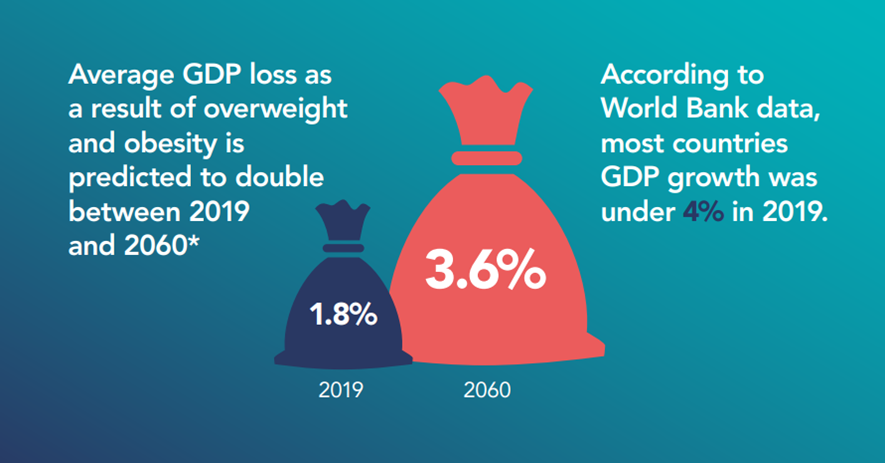
Maintaining or reducing the prevalence of overweight and obesity can reduce the economic impacts of overweight and obesity in the future.

“As patients, we don’t want to be looked at as an economic statistic, or a burden. We are people living with a disease, so any measures taken as a result of looking at the costs of obesity should be with a call to action for better care, improved access to treatment, and the removal of bias from society.”
GLOBAL OBESITY PATIENT ALLIANCE
Individuals living with obesity should not be held responsible for economic impacts related to obesity. There are many factors that play a role in obesity, and it’s important that any economic impact is not blamed on individuals.
Why does this matter?
Understanding the long-term impacts of overweight and obesity is essential to avoid rising future costs.
Measuring the economic impacts of NCDs helps us understand the scope of a disease’s impact, the urgency for action, and the costs of inaction. Economic impact studies demonstrate the potential benefits of acting to reduce diseases and have proven essential to galvanise policy actions to create a healthy society.
When looking to address the challenges of overweight and obesity, we already know the root causes of the obesity pandemic, but we need to push for commitment to policies. All governments around the world agreed to voluntary WHO targets in 2013 to halt the rising prevalence of obesity by 2025 — yet no country is on track to meet them. Calculating economic impacts — especially in resource-strapped countries — can get policymakers’ attention and help make the case that the most economically beneficial solution is to take action now.
The primary impetus for evidence-based action on obesity should be for the health and wellbeing of our populations, including those living with overweight and obesity. We all deserve to thrive in healthier environments and to have access to affordable healthcare.
Economic impact studies demonstrate the potential benefits of acting to reduce diseases and have proven essential to galvanise policy actions to create a healthy society
Methodology
How did we measure the impact of overweight and obesity?
This study estimates the current and future economic impact (2019 and 2020–2060, respectively) of overweight and obesity from 28 obesity-related diseases, for eight countries: Australia, Brazil, India, Mexico, Saudi Arabia, South Africa, Spain, and Thailand.[4] The estimated economic impacts are adjusted to 2019 USD values.
In this study, overweight in adults is defined as a body mass index (BMI) of 25–29.9 kg/m2 and obesity as a BMI of 30 kg/m2 and above. For children, overweight is defined as weight one to two standard deviations above the median weight and obesity as more than two standard deviations above the median.
Our data sources
We used country-specific data sourced from published studies and databases published by international organisations.[5]
Our approach:
World Obesity and RTI International developed a model to estimate the economic impact of overweight and obesity from a societal perspective. The components of the model are depicted in Figure 1. Our model is mainly divided into two components: direct economic impacts and indirect economic impacts.
- Direct economic impacts include the costs of obesity-related healthcare needs.
- Indirect economic impacts include the costs of productivity losses and reduction in human capital from premature mortality. Studies show that some people with obesity miss more days of work and many are unable to work to their full potential when they are at work.[6] This is likely due to medical issues they are managing. Additionally, premature mortality from obesity-related conditions indicates a loss of potential future contributions to the economy.
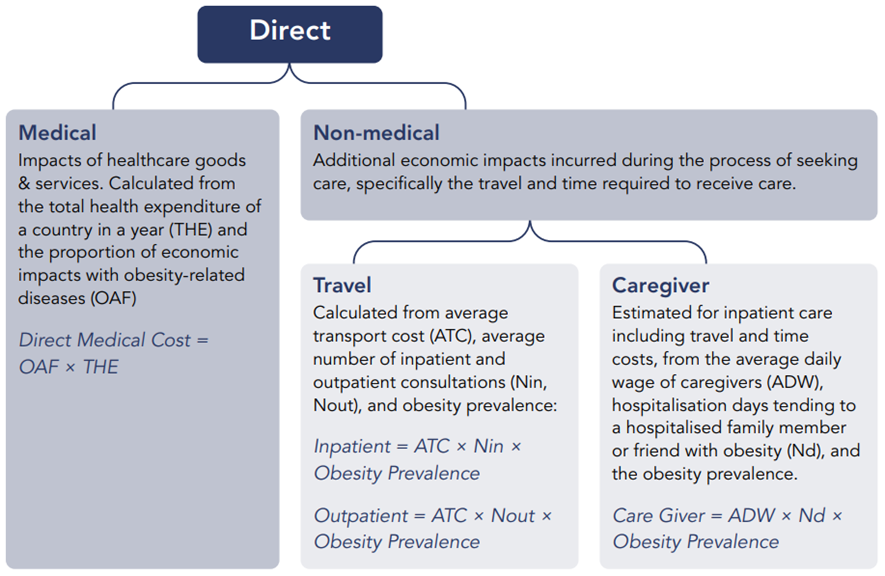
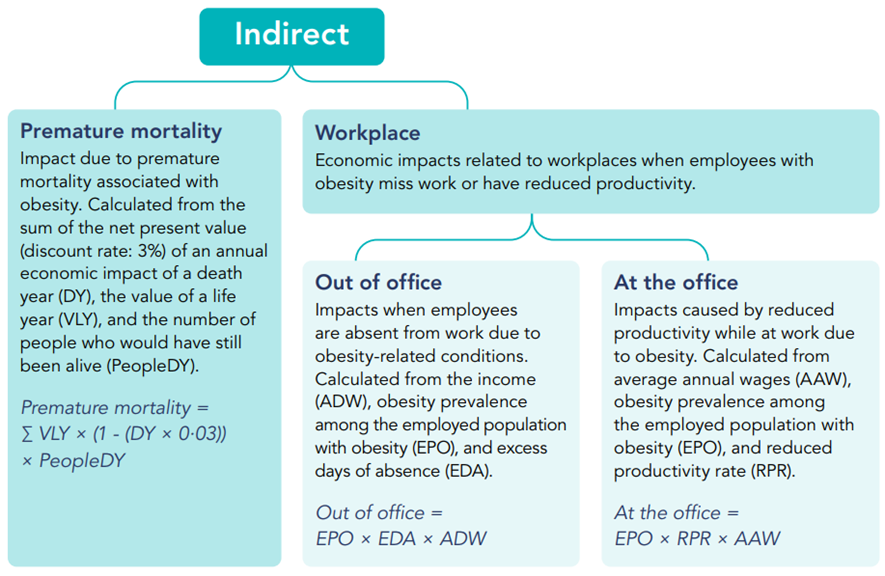
The economic impacts are defined as the cost of medical treatment for obesity-related diseases and the economic loss from obesity-attributable mortality and morbidity
Costs of weight stigma and discrimination that fall on individuals are not included.[7]
Economic impact = Direct impact + Indirect impact
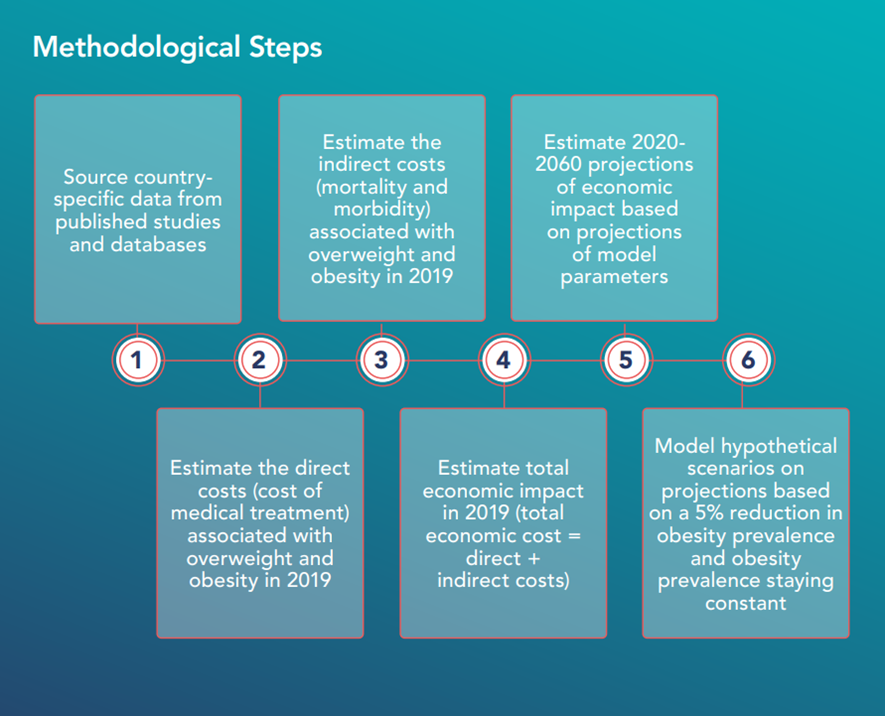
Estimation process
Our two-step estimation process:
STEP 1: Using the model outlined on the previous page we estimated the economic impact of overweight and obesity in 2019.
STEP 2: We estimated future economic impact from 2020 to 2060. Projections extended the modeling approach used in Step 1 and were based on three hypothetical scenarios around obesity prevalence.
- Projection: We estimated country-level obesity prevalence based on NCD-RisC data from 1975 to 2016 for men, women, boys, and girls.
- A 5% Reduction of Projection: We estimated economic impact based on a 5% reduction in obesity prevalence from our Scenario 1 projection.
- Constant: We estimated economic impact based on holding obesity prevalence constant at 2019 levels.
Addressing stigma
Weight stigma refers to the discriminatory acts and ideologies targeted towards individuals because of their weight and size.
Weight stigma is often the result of a misunderstanding of the complex causes of obesity.
Weight gain is often attributed to individual failure alone and there is a lack of information and understanding about the complex mix of genetic, environmental, and biological factors that drive it.
The dominant obesity narrative often results in blaming people with obesity for their disease, and perpetuates harmful stereotyping of people with obesity as lazy and lacking in willpower.
Weight gain is often attributed to individual failure alone and there is a lack of information and understanding about the complex mix of genetic, environmental, and biological factors that drive it.
As with economic impact studies of any major disease that looks at medical costs and lost productivity, measuring the economic impact of obesity demonstrates the need for both compassion and support for individuals.
It strengthens calls for investment in comprehensive care and policies that focus on the prevention and management of obesity in healthcare systems and beyond.
There are also recognised challenges with economic terminology when discussing obesity despite our intended focus on impact rather than cost.
We challenge ourselves and others to talk about obesity sensitively and with care and be conscious of how our language may be interpreted.
At the same time, this study demonstrates that investment in earlier, evidence-based treatment of obesity alongside the implementation of policies that address the obesogenic environment would result in better outcomes for individuals and economies.
The economic consequences of overweight and obesity highlighted in this study, along with the challenges to individual and population health, mean we must join forces to address the root causes of overweight and obesity and invest in evidence-based obesity care.
Insights from patient organisations
These range from the impact of bullying to professional costs such as the reduced likelihood of promotion. These costs are too often overlooked but are increasingly being explored.
“People living with obesity should have the right to evidence-based care. They should be treated with respect and should be free to join and contribute to the useful life of their countries, regardless of whether or not they have larger bodies. People under treatment (medical and psychological) tend to make decisions that help them stay healthy.”
Obesidades Mexico
“As patients, we don’t want to be looked at as an economic statistic, or a burden. We are people living with a disease, so any measures taken as a result of looking at the costs of obesity should be with a call to action for better care, improved access to treatment, and the removal of bias from society.”
Global Obesity Patient Alliance
“The global economic and personal costs of obesity are important. We need to disrupt the outdated blame narrative and invest in action for healthier and happier people. See our WIN report to learn more about the personal costs of obesity.”[8]
Weight Issues Network (Australia)
Policy recommendations
The economic impacts are far too great to ignore.
Leaders at the national and international level must take immediate action to reduce the economic impact of overweight and obesity in their countries and communities. Obesity has many root causes, all of which must be addressed for us to create a healthier future.
The obesity ‘ROOTS’ framework, launched by the World Obesity Federation in 2020, provides suggestions for obesity policy and advocacy that can be adapted to different national settings.
R (Recognise) — Recognise obesity as a disease and a risk factor, and promote understanding of its complexities
O (Obesity Surveillance) — Develop obesity surveillance and monitoring programmes and adopt evidence-based strategies for addressing obesity
O (Obesity Prevention) — Implement obesity prevention and management policies across the life course
T (Treatment) — Ensure treatment is equitably offered and accessible to all who want it
S (Systems Based Approaches) — Adopt systems-based approaches to address obesity
In recognition of the economic impact of obesity and in line with the ROOTs framework, we call on policymakers to:
R
Recognise obesity as a disease and a risk factor, and promote understanding of its complexities
Obesity is not only a risk factor for other diseases, it is also a complex, relapsing, multifactorial disease in its own right. Further, obesity has several drivers including genetics, the environment, commercial factors, healthcare access and mental health, among others. Recognising that obesity is a disease with multiple drivers is vital to help shift the public discourse away from an individual blame narrative. A shift in the narrative should in turn encourage people to seek medical care, increase access to treatment for all that need it, foster investments in obesity research, and demonstrate the need to prioritise and improve the education of health professionals to prevent and manage obesity. Recognising obesity as a disease and a risk factor can also help reduce weight bias and stigma, another driver of obesity that has repercussions on mental and physical wellbeing and prevents people from seeking necessary medical care.
O
Develop obesity surveillance and monitoring programmes and adopt evidence-based strategies for addressing obesity
All approaches to the prevention, management and treatment of obesity should be data-driven and evidence-based. Obesity monitoring and surveillance allows us to keep track of obesity trends and fully understand its determinants, treatment options, economic impact, and policy consequences. Research must be funded, supported and acted upon by governments, and must actively seek out the involvement of people with lived experience of obesity. Work such as this — that interrogates the long-term impacts of obesity — helps push for commitment to evidence-based policy action by making the case clear to national decision-makers.
O
Implement obesity prevention and management policies across the life course
Halting the rise in overweight and obesity requires policies that can help prevent obesity throughout the life course and create healthy environments. Investing in childhood obesity prevention and treatment is vital to halt a course of poor health and social outcomes in adulthood, while addressing adult obesity can prevent the risk of obesity being passed down through generations. Equally, addressing the commercial determinants of health and improving the environment we live in is essential for halting the rise in overweight and obesity, supporting the maintenance of a healthy weight, and helping people to retain health gains from interventions.
To help address the environmental drivers of obesity, we encourage policymakers around the world to reaffirm their previous commitments to childhood obesity and NCDs and prioritise population-based regulatory and fiscal measures to create health-promoting environments, by:
- Restricting the marketing of foods and drinks to children
- Taxing sugar-sweetened beverages
- Mandating front of pack labelling
- Limiting portion and package sizes
- Increasing access to safe spaces for physical activity
As well as addressing the drivers, policymakers must adopt rigorous principles of engagement to prevent commercial interests from undermining health goals.
T
Ensure treatment is equitably offered and accessible to all who want it
In recognition of the fact that obesity is a disease, we call for obesity treatment to be integrated into Universal Health Coverage as an “essential health service.” This would ensure that children, adolescents and their families have equitable access to adequate prevention and treatment services. In addition, health services should build multi-disciplinary teams to support people living with obesity and provide specialist and general training in weight management for healthcare professionals and medical students. We urge political leaders to build strong health systems that are equipped to manage and treat obesity and related illnesses.
S
Adopt systems-based approaches to address obesity
Interventions to address obesity will require a ‘whole of government’ approach and actions from multiple sectors to create a healthier environment for all children and their families. It is important to use a systems-based approach and engage the food, health, education and other key sectors, as well as involving communities, families and children, and civil society organisations. Ministries of health, education, social development, finance, media/culture, food/agriculture, welfare and transport all have a responsibility in supporting the development of healthy, sustainable environments for everyone.
Conclusion
Obesity is a growing issue with deep, societal roots that requires decisive action from everyone.
The magnitude of the economic impacts — present and future — associated with overweight and obesity are significant and widespread. The time for evidence-based action on our obesogrenic environment and the other roots of obesity has long passed.
COVID-19 has demonstrated that we are capable of worldwide, societal responses to health challenges when there is political will and resources are made available. As a major risk factor for severe COVID-19 disease, obesity has been in the spotlight. We argue that we must use this renewed energy for evidence-based, sustainable change.
Improved understanding of the long-term impact of overweight and obesity on individuals, communities and health systems must push us forward and onwards in our pursuit for a healthier world for us all. Comprehensive, cross-sectoral policies that help prevent, manage and treat obesity will be vital to reducing its prevalence globally. Adopting the ROOTS framework on obesity gives us the tools to get there.
Endnotes
See the original publication
Note
Novo Nordisk, who provided the unrestricted educational grant received by the World Obesity Federation that supported this work, had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
All authors had full access to the data and had final responsibility for the decision to submit for publication.
References
See the original publication
Table of Contents (TOC)
- Introduction
- Key takeaways
- Why does this matter?
- Methodology
- Economic impact breakdown
- Estimation process
- Addressing stigma
- Insights from patient organisations
- Policy recommendations
- Conclusion
Originally published at https://www.worldobesity.org
World Obesity Federation, 2021. The Economic Impact of Overweight & Obesity In 8 Countries. Summary report. [online] Available at: https://data.worldobesity.org/publications/ [Accessed 3 November 2021].
Economic impacts of overweight and obesity: current and future estimates for eight countries
http://orcid.org/0000-0002-7486-5176
Adeyemi Okunogbe1,
Rachel Nugent2,
Garrison Spencer2,
Johanna Ralston3,
John Wilding3












