The is a short article by the editor of the blog, based on the paper below published in 2019, considering the Palliative Care Day in October 9 th, 2021.
Palliative care in Brasil: present and future (with demand estimates up to 2040)
Revista da Associação Médica Brasileira
Cledy Eliana dos Santos 1,2,5Luciana Silveira Campos 1,6Newton BarrosJosé Américo Serafim 1 4Daniel Klug 3Ricardo Pedrini Cruz 1
June 2019
Credit to the image: site care
Key messages (edited by the author of the blog)
Results
The Current Supply of Palliative Care Services in Brazil is far from meeting the needs of the population today. And the demand is growing fast:
- The expected increase in the Brazilian population for 2000–2040 is ~31%.
- The minimum estimate of patients with palliative care needs was 662,065 in 2000 and 1,166,279 in 2040 (76% increase)
- The staff required, number of doctors and number of nurses will increase by more than 30 % in the 2000 – 2040 period;
Conclusion:
- Given the aging of the population and the increased life expectancy, a national strategy foreseeing care needs becomes imperative.
- The expansion of the support network for chronic and non-transmissible diseases is necessary,
- but the training of existing human resources at all levels of attention to perform palliative actions can be a feasible alternative to minimize the suffering of the population.
ORIGINAL PUBLICATION
OBJECTIVE:
To estimate the human resources and services needed to meet the demand of the Brazilian population who would benefit from palliative care, based on the population growth projection for 2040.
METHODS:
Population and mortality estimates and projections were obtained from the Brazilian Institute of Geography and Statistics. Service needs were estimated based on literature data.
RESULTS:
- The expected increase in the Brazilian population for 2000–2040 is 31.5%.
- The minimum estimate of patients with palliative care needs was 662,065 in 2000 and 1,166,279 in 2040 (76% increase)
- The staff required for each hundred thousand inhabitants would increase from 1,734 to 2,282, (32% increase)
- the number of doctors needed would increase from 4,470 to 6,274, and (40% increase)
- the number of nurses from 8,586 to 11,294, for the same period (32% increase)
CONCLUSION:
- The definition of a national strategy predicting the increasing palliative care needs of the population is necessary.
- The expansion of the support network for chronic and non-transmissible diseases is necessary, but the training of existing human resources at all levels of attention to perform palliative actions can be a feasible alternative to minimize the suffering of the population.
KEYWORDS:
Palliative care; Hospice care; Terminal care
OBJETIVO:
Estimar as necessidades de recursos humanos e serviços necessários para o atendimento de pacientes que se beneficiariam de cuidados paliativos a partir da projeção de crescimento da população brasileira até 2040.
MÉTODO:
As estimativas e projeções populacionais e de mortalidade foram obtidas nos dados do Instituto Brasileiro de Geografia e Estatística e do Sistema Único de Saúde. As estimativas de estrutura de serviços e recursos humanos foram realizadas a partir de dados da literatura.
RESULTADOS:
A expectativa de aumento da população brasileira entre 2000 e 2040 é de 31,5%. A estimativa mínima de pacientes com necessidades de cuidados paliativos foi de 662.065 em 2000 e é de 1.166.279 em 2040. O número de equipes necessárias para cada 100 mil habitantes passaria de 1.734 para 2.282 no mesmo período; o número de médicos foi de 4.770 para 6.274 e o número de enfermeiros necessários para atender as demandas dessa população foi de 8.586 para 11.294 nesse espaço de tempo.
CONCLUSÃO:
A definição de uma estratégia nacional prevendo a necessidade de cuidados crescentes da população se torna necessária. A expansão da rede de assistência a doenças crônicas e não transmissíveis se mostra necessária, porém a capacitação de recursos humanos já existentes em todos os níveis de atenção para desempenhar ações paliativas pode ser uma alternativa factível para minimizar o sofrimento da população.
PALAVRAS-CHAVE:
Cuidados paliativos; Cuidados paliativos na terminalidade da vida; Assistência terminal
FULL VERSION (English)
Introduction
Chronic non-communicable diseases (CNCD) are the primary causes of death worldwide, corresponding to 70% of all deaths (40 million people each year).
Approximately 80% of these deaths occur in low- and middle-income countries. In Brasil, CNCDs correspond to approximately 74% of the total number of deaths.
Between 2008 and 2015, the four CNCDs prioritized by the World Health Organization (WHO) were circulatory diseases, cancer, respiratory diseases, and diabetes, which accounted for 60% of all deaths recorded in the Mortality Information System — Single Health System.
Due to the characteristics of the CNCDs, patients often evolve to conditions under which there is no possibility of cure, with a prognosis of death in about a year, requiring palliative care (PC) to manage the suffering caused by the disease and improve the quality of life.
Although the evidence suggesting that patients with chronic non-neoplastic diseases require end-of-life care, in most countries, PC is directed at patients with terminal neoplastic diseases with no therapeutic possibility of a cure.
The PC model comprises some measures to be taken well before the final stage of the disease.
- PC requires early identification, assessment, impeccable management of pain and other problems of physical, psychosocial, and spiritual nature in the period close to death.
- Ideally, PC should juxtapose the curative treatments in cases of poor prognosis, in a patient-centered integral approach, taking into account existential, psychosocial, and clinical needs.
Several studies have been conducted to estimate the population in need of palliative care.
Usually, these needs are estimated using epidemiological approaches or by evaluating the use of these services by the population.
The epidemiological approach uses cause-specific mortality from diseases that would benefit from PC, per type and frequency of symptoms patients would probably experience at the end of life.
This method is useful to identify all patients in palliative care because it does rely on the provision of services.
The first measurement of PC needs in Brasil was presented more than a decade ago, comparing the mortality data registered in 2004 with international parameters.
A recent Brazilian publication that used the national registry of deaths and hospital admissions of 2014 and included all adults who died in that year estimated that between 24.6% and 85.2% of the patients who died of CNCD would have had an indication for PC, depending on the method used.
The authors concluded that the method closest to the Brazilian reality would be the one that estimates that 57.2% of [11] of the patients who died of CNCD would have had an indication for PC, which would amount to 702,195 patients.
… the demand estimates for palliative care (PC) in 2016 are in the range of 700.000 patients, considering that ~ 57 % of the patients who died of NCDs in 2016 would have had an indication for PC …
The objective of this study is to estimate the human resources and the structure of services required, as well as the number of patients who would benefit from PC, using the projection of Brazilian population growth for 2040 and the parameters for estimates of PC needs proposed in the literature.
Demographic Database
The population data for 2000–2015 and projections of population growth and mortality for 2016–2040 were obtained from the website of the Brazilian Institute of Geography and Statistics (IBGE). The mortality data for 2000–2015 were obtained from the Mortality Information System of the Single Health System (SIM-SUS). The variables used to generate the SIM-SUS tables were Chapters of the International Classification of Diseases, deaths per household, during 2000–2015.
Criteria for:
1) Estimate of the population with palliative care needs
The basis of calculation for the population that would benefit from PC was the absolute number of deaths per year..The minimum proportion of patients was 57.2% of the number of deaths, based on what is proposed by Murtagh et al., and the maximum was 85.2% of the total number of deaths, based on the proposal by McNamara et al.
2) Estimate of the number of hospital beds
The basis of calculation for the number of hospital beds needed to assist people in PC were the population data for 2000–2015 and estimates of population growth for 2016–2040 by the IBGE. The estimate was performed based on the parameters of the United Kingdom,.also used in Portugal: 45 hospital beds for every million inhabitants.
3) Estimate of the type of hospital beds
The basis of calculation was the number of hospital beds needed to assist people in PC (45 hospital beds for every million inhabitants),,, and the estimate of type of hospital bed was performed as proposed in the literature: 30% of the beds in general hospitals, 50% in an institution of medium and long stay, and 20% of the beds in homes or support homes.,,
4) Estimate of the number of inpatient units
The basis of calculation for the number of inpatient units necessary to assist people in PC was the number of hospital beds needed for that population. It was considered that the units should have between 10–15 beds, based on estimates from the literature.
5) Estimate of the of staff needed
The basis of calculation for the staff needed to assist people in PC were the population data for 2000–2015 and estimates of population growth for 2016–2040 by the IBGE. We considered the need for a staff of primary care/home care for every 100–150 thousand inhabitants, according to the criteria established in the literature..
6) Need for professionals with PC training in Brasil
The basis of calculation for the number of professionals with PC training needed for assistance was based on population data for 2000–2015 and estimates of population growth for 2016–2040 by the IBGE. For the estimate of the number of doctors, we considered the proposed 25–30 doctors per million inhabitants. The basis for calculating the number of nurses was the estimate of the number of hospital beds needed. We used as a criterion the proposal of 1 to 1.2 nurses for each hospital bed.
7) Data protection and ethical issues
The research project was approved by the Research Ethics Committee of the Conceição Hospital Group under the number 533.468, on 05/02/2014, thus complying with the ethical criteria for human research of the 466/2012 Resolution of the Ministry of Health. The need for a Free and Informed Consent Form was waived because we used free-access data by the Ministry of Health, not linked to any patient identification.
The projection of the Brazilian population for 2000–2040 by the IBGE shows a growth of 31.5%.
Figure 1 presents the population data for 2000–2015, projections of the population for 2016–2040, the mortality rates for 2000–2015 from the SIM-SUS, the estimate of mortality for 2016–2040 by the IBGE, and the minimum and maximum estimates of the population that would benefit from PC during 2000–2040..
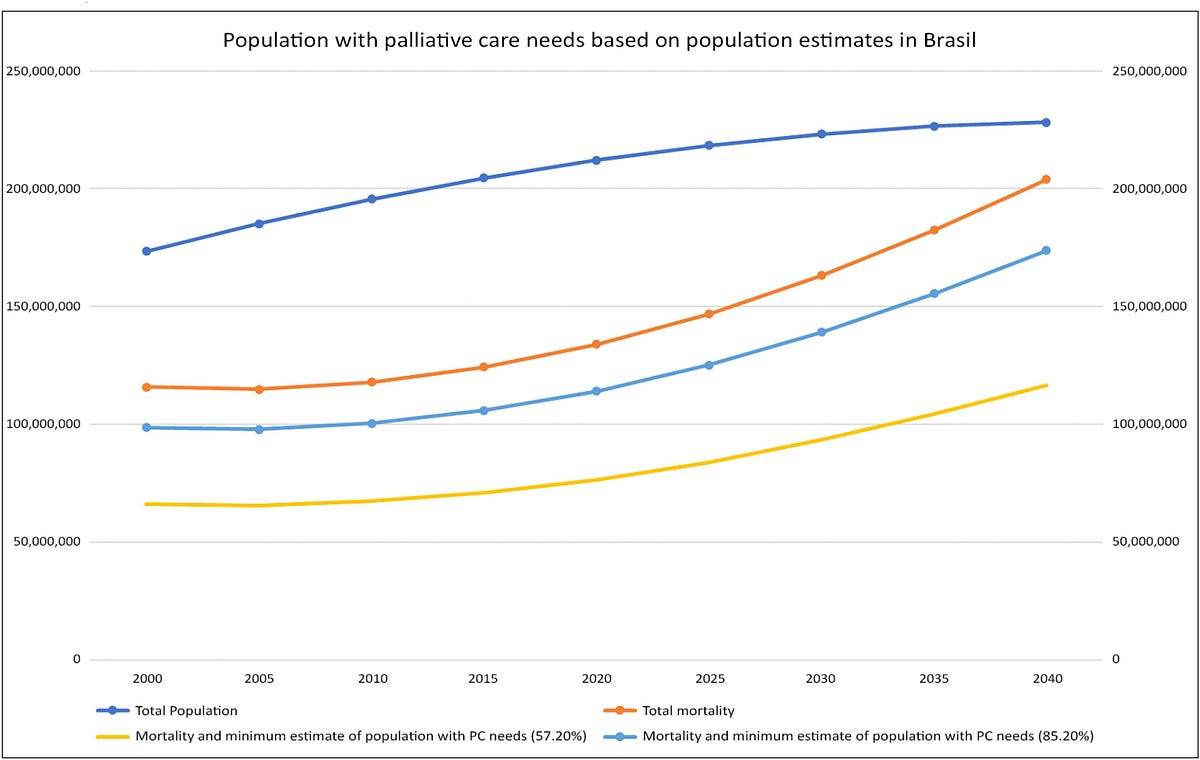
Table 1 shows the number of inpatient units, staffs, doctors, and nurses for the care of patients with palliative care needs.
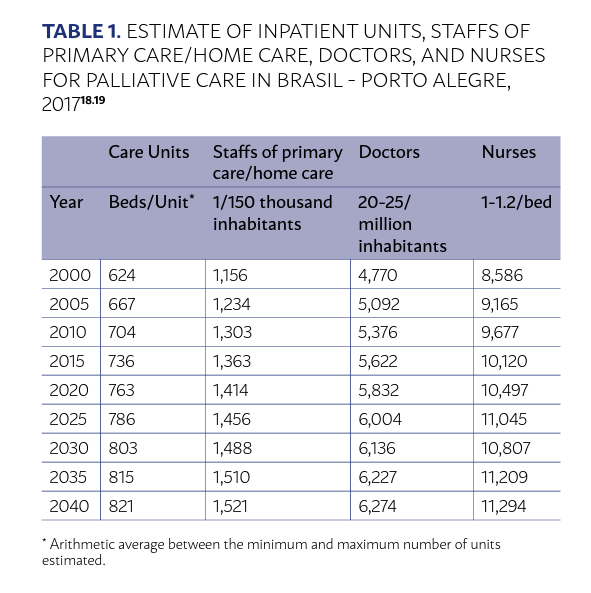
The inpatient units should have between 10 and 15 beds, and a staff of primary care/home care should be organized for every 150 thousand inhabitants.
In the table, we present the arithmetic average between the minimum and maximum numbers of units estimated according to the number of beds in each one of them.
- For the year 2000, the average projection was 624 units, and for 2040, the projection was a total of 821 inpatient units.
- The number of staffs of primary care/home care needed to meet the demand of the population ranged from 1,156 in 2000 to 1,521 in 2040.
In 2000, there was a need for approximately
- 4,770 doctors and
- 8,586 nurses.
For the year 2040, a total of
- 6,274 doctors and
- 11,294 nurses would be needed for the care of patients with PC needs.
The distribution of beds was made according to the following:
while for the year 2000 an average of 7,805 beds was estimated — 2,342 in general hospitals, 3,903 in institutions of medium/long stay, and 1,561 in support homes -, for 2040, 10,267 hospital beds would be necessary — 3,080 beds in general hospitals, 5,133 in units of medium/long stay, and 2,053 in support homes.
The objective of this study was to analyze the needs of PC based on demographic data and projections of population growth and mortality of the Brazilian population.
There are several estimates and parameters developed to estimate the PC needs of a given population, and there is no consensus among authors about which is the most appropriate.
Using the criterion that seemed most appropriate for the Brazilian population, in the year 2020, 765,855 people would have an indication for PC in Brasil.
Another study by this group examined 1.7 million hospital admissions in Brasil of patients under ICD-10 (Code of the International Classification of Diseases — 10), “clinical complications for the treatment of cancer” and the network available for patients in PC.
In Brasil, it is estimated that 90% of these hospitalizations are related to a possible indication for PC.
- Between 2008 and 2016, there were 1.7 million hospital admissions under this CID, distributed among 3,374 health units in Brazilian territory, 91% of them in 380 hospitals.
- In December 2016, there were 115 institutions providing PC registered at the National Academy of Palliative Care.
- Seventy-nine percent were hospital units, 12.3% were clinics/health centers, 4.7% were home care services, and 3.8 corresponded to university leagues.
The installed capacity is far from meeting the needs of the population today.
In Brasil, it is estimated that 90% of these hospitalizations are related to a possible indication for PC.
The installed capacity is far from meeting the needs of the population today.
Palliative care treats death as a natural process of life, with no intention to postpone or hasten it. Its objective is to relieve the pain and other distressing symptoms.
It integrates psychological, social, and spiritual aspects in the care of the patient, provides a support network so that the patient can live as actively as possible until their death, and supports the family during the mourning process.
Moreover, studies suggest that the survival of patients under PC with neoplasia is equal to or even greater than patients who receive curative treatment until the end of life, with better scores for quality of life.
In addition, PC is cost-effective,.which justifies the investment in service structures and human resources.
Currently, the training of human resources and the provision of services are a challenge in countries of medium and high income that already have a more organized network, in comparison with that of Brasil, to serve the population.
Given the aging of the population and the increased life expectancy, a national strategy foreseeing care needs becomes imperative.
Although it is necessary to expand health care networks, the training of already existent human resources on all levels of care, which are capable of spreading the concept of PC across their workplaces of activity and perform palliative actions, would likely be a feasible alternative to alleviate the suffering of the population affected by progressive and incurable diseases after its evolution makes it irreversible.
Given the aging of the population and the increased life expectancy, a national strategy foreseeing care needs becomes imperative.
Although it is necessary to expand health care networks, the training of already existent human resources on all levels of care … would likely be a feasible alternative to alleviate the suffering of the population affected …
References
See original publication.
About the authors & Affiliations:
Cledy Eliana dos Santos 1,2,5
Luciana Silveira Campos 1,6
Newton Barros José Américo Serafim 1, 4
Daniel Klug 3
Ricardo Pedrini Cruz 1
- Palliative Care and Pain Services. Hospital Nossa Senhora da Conceição — Conceição Hospital Group — Porto Alegre, Brasil
- Community Health Service — Conceição Hospital Group — Porto Alegre, Brasil
- Research and Education Management — Conceição Hospital Group — Porto Alegre, Brasil
- Department of Informatics of the Single Health System — Ministry of Health — Brasília, Brasil
- Research Center on Health Services and Technologies — Faculty of Medicine of the Porto University — Porto, Portugal
- Public Health Institute of the Porto University — Faculty of Medicine of the Porto University — Porto, Portugal
Originally published at https://www.scielo.br.












